Late-Onset Citrobacter koseri Endophthalmitis with Suture Exposure after Secondary Intraocular Lens Implantation
Article information
Abstract
A 54-year-old male patient was seen in clinic for ocular pain and decreased vision in the right eye with duration of two days. He underwent a cataract operation for his right eye 12 years ago, then a sclera-fixated secondary intraocular implantation and pars plana vitrectomy three years ago due to intraocular lens dislocation. At the initial visit, his visual acuity was restricted to the perception of hand motion. An edematous cornea, cells, flare with hypopyon, and exposed suture material at were observed at the six o'clock direction by slit lamp. Vitreous opacity was noted from B-scan ultrasonography. The patient was diagnosed with late-onset endophthalmitis and an intravitreal cocktail injection was done. On the next day, the hypopyon was aggravated, and therefore a pars plana vitrectomy was performed. A vitreous culture tested positive for Citrobacter koseri. After 12 weeks, the best corrected visual acuity of the right eye improved to 0.7 and a fundus examination revealed a relatively normal optic disc and retinal vasculature. We herein report the first case of endophthalmitis caused by Citrobacter koseri in Korea. Exposed suture material was suspected as the source of infection in this case and prompt surgical intervention resulted in a relatively good visual outcome.
Infectious endophthalmitis is a serious condition in which the internal structures of the eye are invaded by microorganisms such as bacteria, resulting in an inflammatory response that ultimately may involve entire ocular tissues. The majority of cases of endophthalmitis occur after surgery, and most cases follow cataract extraction, with almost all being bacterial in origin. Thus, postoperative endophthalmitis is an extremely worrisome and potentially devastating complication of cataract surgery.
A significant percentage of cases of infectious endophthalmitis proved to be culture-negative [1,2]. In pseudophakic endophthalmitis, culture-negative cases account for 25% to 35% of all cases [2-4]. Among culture-positive cases, Gram-positive organisms account for 75% to 90%. Gram-negative organisms, such as Pseudomonas and Haemophillus, accounted for about 6% of culture-positive cases in the Endophthalmitis Vitrectomy Study [2,3]. Despite its rarity, endophthalmitis caused by Gram-negative bacteria is known to have a worse prognosis than that caused by Gram-positive bacteria. Among cases of culture-positive endophthalmitis, Citrobacter species are a relatively rare species, and postoperative endophthalmitis caused by Citrobacter koseri has not been reported in Korea [5-8].
We herein report a case of late-onset infectious endophthalmitis caused by Citrobacter koseri (previously called Citrobacter diversus), which occurred three years after a secondary intraocular lens implantation (IOL).
Case Report
A 54-year-old male patient was seen in clinic for ocular pain and decreased vision in the right eye for with duration of two days. The patient denied any history of diabetes mellitus, hypertension, pulmonary tuberculosis, or any other systemic diseases. He underwent a cataract operation in his right eye 12 years ago. He underwent a secondary IOL implantation with sclera fixation and pars plana vitrectomy of the right eye three years ago, due to IOL dislocation.
Initial visual acuity of the right eye was limited to the perception of hand movement, while that of the left eye was 0.8 according to the Snellen visual acuity chart. Initial intraocular pressure was 17 mmHg and 12 mmHg in right and left eyes, respectively, according to readings from a non-contact tonometer. The patient had mild flu-like symptoms 3 to 4 days before the onset of ocular pain, although his body temperature at clinic presentation was 36.4℃. Following a slit lamp examination of the right eye, it was found that the conjunctiva was severely injected and exposed prolene suture material was noted at the 6 o'clock direction. The cornea was edematous with Descemet's membrane folds and the pupil was mid-dilated and fixed. The anterior chamber was hazy with cells and flares, and an approximately 3.0 mm-height hypopyon was observed (Fig. 1). The lens, vitreous, and fundus were not visualized. Opacity was noted in the vitreous cavity according to B-scan ultrasonography (Fig. 2). An orbital computed tomography with contrast was done for further examination and showed no remarkable abnormal finding. Routine lab tests, including blood culture, were done and revealed no remarkable result.
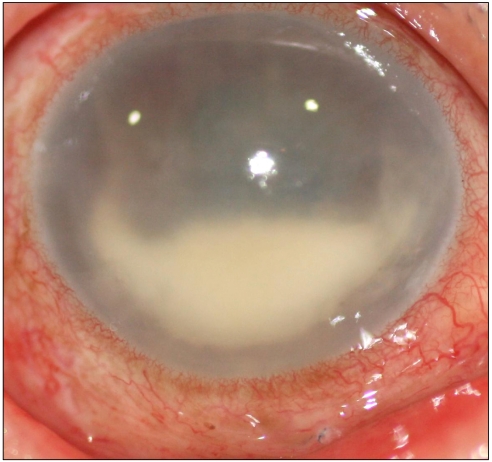
Slit lamp photography of the right eye at initial presentation. Severe conjunctival injection and exposed suture material at 6 o'clock direction were observed. Also, an edematous cornea with 3.0-mm-height hypopyon was observed.
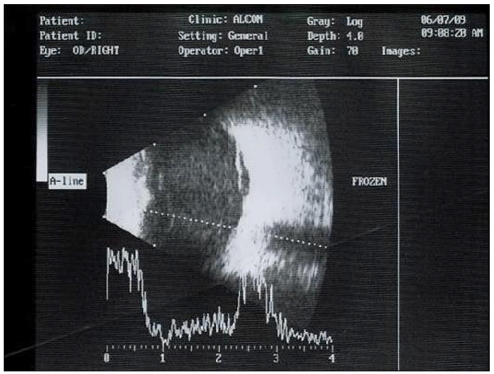
B-scan ultrasonography of the right eye at initial presentation. Significant vitreous opacity was observed.
We diagnosed the patient as having delayed postoperative infectious endophthalmitis due to suture exposure. On the same day, samplings of the anterior chamber fluid and vitreous were done under local anesthesia. After sampling, 1.0 mg/0.1 mL vancomycin (1 g/vial, Vancocin CP; Eli Lilly, Seoul, Korea), 2.0 mg/0.1 mL ceftazidime (1 g/vial, Ceftazidime; Youngjin Pharmaceutical, Seoul, Korea), and 400 µg/0.1 mL dexamethasone (5 mg/mL, Dexamethasone; Daewon Pharmaceutical, Seoul, Korea) were injected into the vitreous cavity. Anterior chamber fluid and vitreous were sent to the lab for cytology, smear, and culture for bacteria and fungi.
Fortified cefazolin (1 g/vial, Cefamezin; Donga Pharmaceutical, Seoul, Korea) and fortified tobramycin eye drops (50 mg/2 mL/vial, Tobra Inj., Daewoong Pharmaceutical; 5 mL/bottle, Tobra eye drops, Daewoong Pharmaceutical) were administered every hour alternatively, along with a topical steroid eye drop (5 mL/bottle, Predforte eye drops 1%; Allergan, Irvine, CA, USA), administered every 2 hours, to be used used along with systemic antibiotic and steroid treatments. On postoperative day 1 after injection, ocular pain decreased but the hypopyon of the anterior chamber increased slightly to 4 mm of height and corneal edema was the worsened slightly as well. We decided to undergo a pars plana vitrectomy and removal of the IOL with exposed suture material, which was thought to be the source of the infection.
Pars plana vitrectomy (PPV) with removal of the IOL and suture material was done under general anesthesia. During the operation, a pus-filled vitreous cavity and some retinal hemorrhages were observed. However, significant corneal edema and vitreous haziness obscured a detailed examination of fundus. At the end of the operation, an intravitreal cocktail injection was done following the same regimen as that of the previous injection.
On postoperative day 1 after the vitrectomy, visual acuity was limited to the perception of hand motion and intraocular pressure was within normal range. Following lamp examination, it was observed that the cornea was still edematous, but hypopyon was not observed. The posterior segment was not observed due to severe corneal edema, but there was a significant decrease in vitreous opacity based on the findings of B-sound ultrasonography. All ophthalmic solutions and systemic medications were continued. On postoperative day 2, a culture of the vitreous tap revealed growth of Citrobacter koseri. This Citrobacter koseri was only resistant to ampicillin, and susceptible to second- and third-generation cephalosporins by antibiotic sensitivity test, and therefore we continued with the medication. After one week, the visual acuity of the right eye had improved to counting of fingers at 30 cm. Corneal edema was decreased, and the optic disc was visible on fundus examination. After 12 weeks, the best corrected visual acuity was improved to 0.7 (refractive errors +12.0 sph -1.50 cyl Ax90), according to Snellen chart examination. The cornea was clear and a fundus examination revealed a relatively normal optic disc and retinal vasculature (Fig. 3).
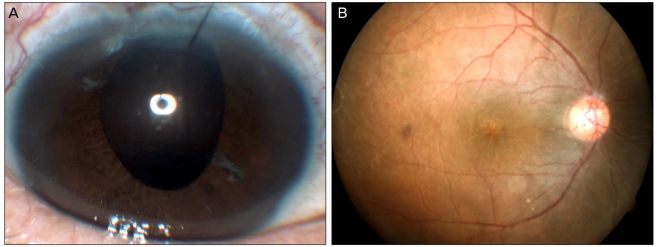
Twelve weeks after vitrectomy, best corrected visual acuity was improved to 0.7 (refractive errors +12.0 sph -1.50 cyl Ax90), according to a Snellen chart examination. (A) Cornea and anterior chamber were both clear. (B) According to a fundus examination, a relatively normal optic disc and retinal vasculature were observed.
Discussion
The incidence of postoperative endophthalmitis is now decreasing in tendency, and reported to have a frequency of 0.05 to 0.68% after cataract extraction surgery [9]. According to Doft et al. [10], the incidence of postoperative endophthalmitis was 0.072% (17 / 23,625) after cataract extraction with or without IOL implantation, 0.30% (3 / 988) after secondary IOL implantation, and 0.051% (1 / 1,974) after PPV. The incidence of endophthalmitis is also known to be increased after secondary IOL implantation and most likely caused by other associated risk factors, including diabetes, transscleral suture fixation of the posterior chamber IOL, polypropylene haptics, preoperative eyelid abnormalities, reentrance through a previous wound, and postoperative wound defects [11].
The microbiologic spectrum is one of the most influential factors in determining visual outcome in endophthalmitis. Less virulent organisms, such as Staphylococci, are associated with better initial visual acuity and final visual outcome [2,12,13]. The association of the virulence of microorganisms with poor visual outcome is proven in several studies [14-17].
Citrobacter koseri, which was found in our patient, is an anaerobic, motile, Gram-negative bacilli and belongs to the genus Citrobacter, within the family of Enterobacteriaceae. Citrobacter koseri is one of the most common species of the Citrobacter genus, and is commonly found in water, soil, and as occasional colonizers of the gastrointestinal tract of humans [17,18]. Like other virulent Gram-negative organisms, endophthalmitis caused by Citrobacter species can be associated with a poor visual outcome in spite of maximal treatment. Chen et al. [8] reported 6 cases of endophthalmitis caused by Citrobacter species, of which 4 cases were caused by Citrobacter freundii and 2 cases were caused by Citrobacter koseri. Final visual acuity was limited to no light perception in 5 eyes among 6 cases, although maximal medical and surgical treatment were undertaken after diagnosis of endophthalmitis. However, in one case caused by Citrobacter koseri, the patient was able to achieve 20 / 30 vision, according to their report [8].
In the current case, we also observed a relatively good visual outcome with a best corrected visual acuity of 0.7 at 12 weeks. The initial visual acuity in the patient was limited to the perception of hand movement. The Endophthalmitis Vitrectomy Study has demonstrated that the vitrectomy was beneficial for eyes presenting with vision of light perception [2]. Thus, the intravitreal cocktail injection was done immediately after the ophthalmic examination and then the systemic evaluation for general anesthesia was performed for further vitrectomy and removal of the IOL in case they became necessary. Postoperative follow-up revealed a definite worsening of the hypopyon and inflammation without improvement, while the suture remained exposed. The corneal edema had worsened as well and we decided to perform a PPV with removal of the secondary IOL, in case further decompensation of the cornea might obscure the proper view for the vitrectomy and IOL removal, which was thought to be the ultimate way to improve the endophthalmitis in the patient. Prompt surgical intervention, including PPV, removal of the IOL with suture material, and intravitreal antibiotic injections resulted in a good prognosis for this case, indicating that early surgical intervention might result in a better visual outcome in cases of Citrobacter koseri infection. Also, the patient previously had a PPV at the time of secondary IOL implantation. The vitrectomized eye might have limited the virulent growth of the organism, as less endophthalmitis has been reported after the vitrectomy, when compared to cataract surgery or secondary IOL implantation [10].
Antimicrobial therapy for Citrobacter infections can be problematic, because these species encode chromosomal, inducible ampC β-lactamase genes, which can be expressed constitutively at high levels due to mutational changes, conferring resistance to multiple antibiotics [19,20]. Thus, Citrobacter species are resistant to β-lactams such as ampicillin and carbenicillin, and are typically also resistant to erythromycin and other macrolides, clindamycin, and vancomycin. Acquired resistance to quinolones and aminoglycosides has also been reported. Antibiotic therapy with extended-spectrum cephalosporins is known to work against Citrobacter species [21]. In the current case, the organism was resistant to ampicillin but sensitive to the rest of the antibiotics and responded well to the vitrectomy and intravitreal cocktail injection.
As far as we are aware, this is the first report of postoperative endophthalmitis caused by Citrobacter koseri in Korea. In the current case, the source of the infection was thought to be the exposed suture material and Citrobacter koseri may have penetrated into the eye along the exposed suture material. Thus, it is emphasized again that any exposed suture material after secondary intraocular implantation or other surgical procedures must be regarded as a possible source of endophthalmitis. The exposed suture material, thus, must be treated with cauterization or covered with the conjunctival flap to prevent any possible infection. Once the endophthalmitis occurs, early surgical intervention with PPV, removal of the IOL, and intravitreal antibiotics injection might result in a good visual outcome.
Notes
No potential conflict of interest relevant to this article was reported.