A Case of Vogt-Koyanagi-Harada Disease in a Patient With Graves Disease
Article information
Abstract
A case of Vogt-Koyanagi-Harada disease (VKH) that developed in a 36-year-old woman with Graves' disease was described. The patient was treated with Lugol's solution and presented with bilateral serous retinal detachment. She had also suffered from methimazole-induced hypersensitivity and steroid-induced myopathy. Fluorescein angiography showed multiple leakage points and a lumbar puncture revealed pleocytosis, which was compatible with VKH. High dose steroid pulse therapy was successful. Altered immune regulation associated with drug-induced hypersensitivity may contribute to the development of VKH in patients with Graves' disease.
Vogt-Koyanagi-Harada disease (VKH) is a systemic autoimmune disorder affecting pigmented tissues in the ocular, auditory, integumentary and central nervous systems.1 Graves' disease is an immune disorder, most commonly caused by hyperthyroidism. Previously, a case of VKH that developed in a patient with Hashimoto's thyroiditis was reported.2 However, the explanation for the association of hyperthyroidism and VKH remains unclear. Here, we describe a case of VKH that developed in a patient with Graves' disease.
Case Report
A 36-year-old woman was referred for blurred vision in both eyes that had lasted for three days. She complained of a stiff neck and headache occurring over the same period. She had been diagnosed with Graves' disease one year previously and was treated with methimazole. However, she had discontinued the methimazole seven months prior, because she was diagnosed with methimazole-induced hypersensitivity following development of a skin rash. After discontinuing the methimazole, the patient was treated with Lugol's solution with 30 mg of prednisolone. After three months, she complained of lower limb weakness. A muscle biopsy was performed, revealing prednisolone-induced myopathy. The dose of prednisolone was reduced to 10 mg. After symptoms developed, she was taken to the hospital for evaluation of systemic diseases in the allergy division of the Department of Internal Medicine. She was referred to retinal clinic for ocular examination.
On examination, her best-corrected visual acuities (BCVA) were 20/100 in both eyes. The anterior chamber was within normal limits. A fundus examination showed disc edema accompanied by a serous retinal detachment in both eyes (Fig. 1 A and B). Fluorescein angiography (FAG) showed multiple leaks at the posterior pole (Fig. 1 C and D). In addition, optical coherence tomography (OCT) revealed subretinal fluid (Fig. 1 E and F). Initially, we suspected prednisolone-induced central serous chorioretinopathy. We decided to observe the patient closely with predisolone tapering to 5 mg for 1 week.
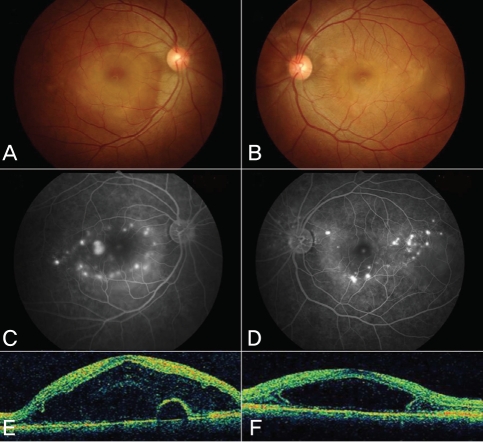
Fundus photography, fluorescein angiography (FAG) and optical coherence tomography (OCT) performed at the initial visit. At that time, predisolone dosage was 10 mg. (A and B) Fundus photography of both eyes. (C and D) FAG showed multiple leakage points. (E and F) OCT showed subretinal fluid affecting macula.
After seven days, the patient's visual acuity did not change, but the subretinal fluid buildup and the retinal detachment worsened. Simultaneously, anterior chamber reaction and vitreous haze developed in both eyes. The leakage pattern on FAG changed (Fig. 2 A and B), and indocyanine green angiography revealed multiple hypofluorescent spots (Fig. 2 C and D). A lumbar puncture revealed pleocytosis with 21 mononuclear cells/dL. The patient was diagnosed with VKH disease and treatment with high dose steroid pulse therapy was recommended. Although the internal medicine physicians were reluctant to use steroids due to the patient's steroid-induced myopathy, intravenous administration of 500 mg of methylprednisolone for three days followed by 30 mg prednisolone with 75 mg of cyclosporine per day was provided. After 40 days, her BCVA recovered to 20/40 OD, 20/25 OS. Fundus examination showed attached retinas bilaterally, and FAG revealed that the leaks had resolved in both eyes (Fig. 3).
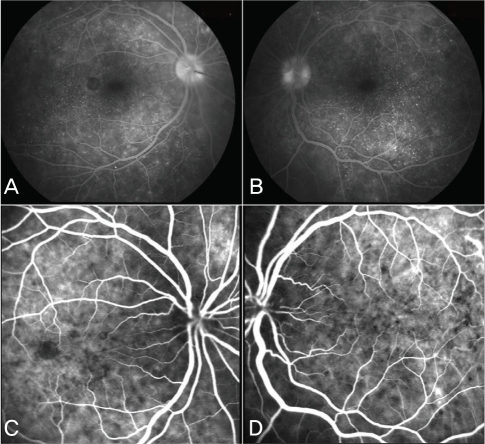
Fluorescein angiography (FAG) and indocyanine green angiography (ICG) performed after 1 week of close observation using 5 mg predisolone under the impression of steroid induced central serous retinopathy. Anterior chamber reaction with vitritis developed. (A and B) FAG showed multiple pin point size leakages. (C and D) ICG showed multiple hypofluorescent spots.

Fundus photography, fluorescein angiography (FAG) and optical coherence tomography (OCT) performed 4 weeks later. After high-dose steroid (500 mg methylpredisolone) pulse therapy, the patient was given 30 mg predisolone with 75 mg of cyclosporine. (A and B) Fundus photography of both eyes. (C and D) FAG showed the multiple leakages point had disappeared. (E and F) OCT showed that subretinal fluid.
Discussion
Since both VKH and Graves' disease are caused by T cell-mediated autoimmune dysfunction, they might share a common pathogenic process.3,4 Moreover, in this case, altered immune regulation that may have resulted from drug-induced hypersensitivity may have contributed to the development of VKH. Although our patient received 10 mg of prednisolone, this did not prevent the development of VKH. This case study illustrates the diagnostic and therapeutic challenges of VKH-associated autoimmune diseases.