Bilateral Spontaneous Anterior Lens Dislocation in a Retinitis Pigmentosa Patient
Article information
Abstract
Purpose
To report a case of bilateral spontaneous anterior lens dislocation associated with retinitis pigmentosa (RP).
Methods
A 45-year-old male with RP presented with elevated intraocular pressure (IOP) in the right eye and was treated with laser iridotomy (LI). After LI, complete crystalline lens dislocation into the anterior chamber occurred. Surgical intervention, including anterior vitrectomy, intracapsular cataract extraction (ICCE), and IOL scleral fixation was performed. Two years later, the same episode occurred in his left eye and a similar treatment was done.
Results
Surgery was successful in both eyes.
Conclusions
This is the first report of bilateral spontaneous anterior lens dislocation in a RP patient.
RP is characterized by night blindness, visual field loss, central vision dysfunction, rod-cone dystrophy, and abnormal retinogram findings.1 Ocular abnormalities associated with RP are vitreoretinal abnormalities, cataracts, glaucoma, keratoconus, and refractive abnormalities.2 Posterior lens dislocation associated with RP was first described by Sato et al. in 2005.3
We report a case of bilateral spontaneous complete anterior lens dislocation associated with RP and elevated IOP that was successfully treated by surgical intervention. As far as we know, this is the first report of bilateral spontaneous anterior lens dislocation in a RP patient.
Case Report
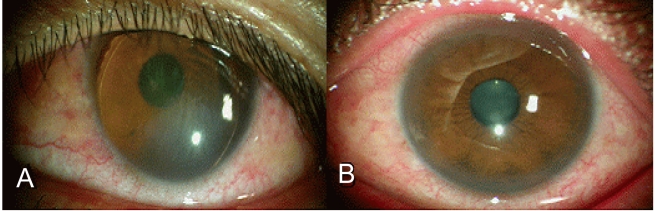
A 45-year-old Korean male presented on March 27, 2003 with right ocular pain. Family history included an older brother with RP. The patient had no systemic disorders. Right and left IOP, measured by a Goldman applanation tonometer, was 66 and 11 mmHg, respectively. Right and left eye best corrected visual acuity (BCVA) was 20/70 with -4.50 +1.00×165 and 20/100 with -3.50 +1.00×180, respectively. Right eye slit lamp examination showed steamy opaque cornea and a central anterior chamber depth of 2 corneal thickness (CT). The left eye cornea, conjunctiva, and anterior chamber were normal. Phacodonesis was noted bilaterally. A slightly hazy fundus, bone-spicule pigmentation sparing macula, and pale optic disc was noted in the right eye (Fig. 1). The patient was given intravenous 15% mannitol (300 mL), oral acetazolamide (Diamox) (500 mg), oral 50% glycerin (Glycerol) (50 cc), carbonic anhydrase inhibitor (Cosopt), and 0.2% Brimonidine (Alphagan) eye drops.
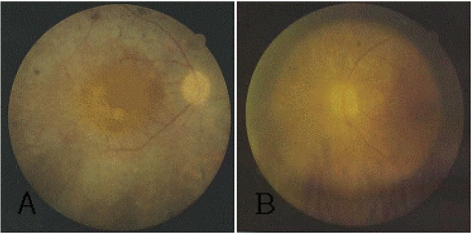
Fundus photograph of the right (A) and left (B) eye. Bone-spicule pigmentation in the entire retina with sparing of the macula and pale optic discs were noted.
All medications were given twice during the night. One day after treatment right eye IOP decreased to 50 mmHg, the cornea became clear, and the central anterior chamber depth remained 2 CT. Therefore, LI was done; 3 hours later IOP decreased to 20 mmHg. Six days later, the cornea was clear, the anterior chamber was deep and clear bilaterally, and the right eye LI opening was patent. Using the Humphrey Visual Field (model 750, Humphrey Instruments, Inc, Dublin, California; C24-2 program) examination showed narrowing to central 10° in both eyes (Fig. 2), and electroretinogram findings were prolonged in a and b amplitudes (Fig. 3).

Visual field of the right (A) and left (B) eye. Extensive peripheral field defect is noted (central 10°). Visual field using the Humphrey Visual Field Analyzer (model 750, Humphrey Instruments, Inc, Dublin, California; C24-2 program).
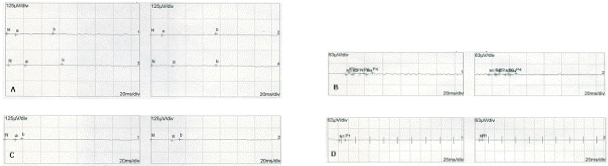
(A) Scotopic ERG shows prolonged rod a-wave implicit times. (B) Oscillatory ERG. (C) Photopic ERG shows prolonged cone b-wave implicit times. (D) 30Hz Flicker ERG.
Two months later, the patient presented with high left eye IOP. The right and left IOP was 14 and 33 mmHg, respectively. The cornea was clear bilaterally. The right eye LI opening was patent, and the anterior chamber was deep and clear. The left eye central anterior chamber depth was 2 CT. Therefore, LI was done. Left eye IOP after 6 weeks was 10 mmHg.
Six months later, on December 19, 2003, the patient presented with right ocular pain. He did not have any episode of ocular trauma. Right and left BCVA was 20/70 and 20/100, respectively. Slit lamp examination showed complete anterior lens dislocation in the right eye. Other ocular findings were unremarkable bilaterally. Right eye anterior vitrectomy, ICCE, and IOL scleral fixation was done. For the surgical procedure, pupillary constriction was achieved using 4% pilocarpine, administered 3 times in 5 minute intervals. A 7 mm wide scleral tunnel was made 1.5 mm posterior to the limbus at the superotemporal side. Healon GV was injected into the anterior chamber to create space between the posterior lens capsule and iris. ICCE was done successfully using capsule forceps. Prolapsed vitreous in the anterior chamber was removed by vitrector. A posterior chamber lens (Alcon CZ70BD) was introduced and sutured to the sclera by the ab interno method. Three days postoperatively, the IOL was well positioned and no abnormal ocular findings were noted.
Two years later, on June 8, 2005, the patient presented with left ocular pain lasting one day. Right and left BCVA was 20/50 with -1.50 +2.00×165 and 20/160 with -3.50 +1.00×10, respectively. Right and left pressure was 11 and 12 mmHg, respectively. Slit lamp showed anterior lens dislocation with mild inflammatory cells, and there were no abnormal findings in the right eye (Fig. 4). Anterior vitrectomy, ICCE, and IOL scleral fixation was done on the left eye. Four weeks post-operatively, left BCVA and IOP was 20/200 with -1.50+1.25×15 and 10 mmHg, respectively. IOL was well positioned in the left eye (Fig. 4). On the patient's last examination, October 10, 2005, right and left BCVA was 20/40 and 20/200, respectively. The IOP was 10 mmHg bilaterally. The cornea, conjunctiva, anterior chamber, and pupil were normal bilaterally. LI opening was patent and IOL was well positioned in both eyes.
Discussion
The causes of ectopia lentis are trauma, pseudoexfoliation syndrome, spontaneous dislocation, and various heredofamilial diseases including Marfan syndrome, homocystinuria, and RP.4,5
In RP patients, Hayashi et al. has suggested that zonular weakness can cause ectopia lentis6 and Namiki et al. showed unilateral zonular dehiscence.7 We report the first case of anterior lens dislocation in an RP patient following high IOP. After glaucomatous attack, mid-dilated pupil occurred with a weakened iris and ciliary body; these structure caused anterior segment lens dislocation.
The mechanisms of glaucoma associated with a dislocated lens are pupillary block, lens degenerative changes, and concomitant anterior chamber angle damages.8 Allingham et al. has suggested three types of pupillary block glaucoma induced from lens dislocation. These include pupillary block by subluxating the lens posterior to the iris, lens incarceration directly within the pupil, and complete lens dislocation into the anterior chamber.9 In this case, IOP elevation was due to posterior pupillary block, which responded dramatically to laser iridotomy.
If the lens is displaced into the anterior chamber, it may be possible to relieve the condition by dilating the pupil and allowing the lens to reposition into the posterior chamber. However with a totally dislocated lens in the anterior chamber, it is better to constrict the pupil and surgically remove the lens. Choi et al. have treated anteriorly dislocated lens by lensectomy, vitrectomy, phacoemulsification, and ab externo scleral IOL fixation.10 For scleral fixation, Young et al. used a scleral tunnel to relieve IOL fluctuation and to maintain anterior chamber depth.11
In this case, the anteriorly dislocated lenses were removed using a 7 mm wide scleral tunnel, combined with an anterior vitrectomy and ab interno scleral fixation. Surgery was successful in both eyes.
This is the first case of bilateral spontaneous anterior lens dislocation in an RP patient reported in the literature.
Notes
* This study was presented in part at the Korean Ophthalmological Society Meeting, Seoul, Korea, October 2005.