Trabecular Microbypass Stent Insertion for Medically Uncontrolled Glaucoma in a Patient with Central Serous Chorioretinopathy: A Case Report
Article information
Dear Editor,
Filtering surgery is indicated for treatment of glaucoma when medication or laser treatment is not sufficient to lower intraocular pressure (IOP); however, the use of topical corticosteroid is mandatory in its postoperative period for modulation of wound healing process to minimize the risk of bleb failure [1]. Such postoperative steroid use may activate the development or progression of central serous chorioretinopathy (CSC) in eyes with or at risk of CSC [2–4]. In this regard, angle-targeted minimally invasive glaucoma surgery (MIGS) may be a better surgical option in glaucoma patients comorbid with CSC because of the shorter use of weaker steroids. Here we describe a case where in whom trabecular microbypass stents were inserted to treat medically uncontrolled glaucoma in an eye with CSC. Written informed consent was obtained from the patient.
A 68-year-old male patient with bilateral open angle glaucoma was referred due to uncontrolled IOP of his right eye despite maximal medical treatment. He had been using Hypadil (nipradilol 0.25%; Kowa, Nagoya, Japan), Alphagan-P (brimonidine 0.15%; Allergan, Seoul, Korea) and Travatan (travoprost 0.004%; Alcon, Korea) for 3 years and intolerant to dorzolamide/timolol fixed combination eyedrops. He also had systemic hypertension, diabetes mellitus and dermatitis treated with oral corticosteroids. On initial examination, corrected visual acuity and IOP of his right eye was 20 / 25 and 25 mmHg, respectively. Fundoscopy revealed macular edema in the right eye. Optical coherence tomography (OCT) showed the subretinal fluid and enlarged choroid beneath the macula of the right eye (Fig. 1A). Fluorescein and indocyanine green angiography demonstrated a focal lesion with fluorescein leakage in the same location. Although glaucoma surgery deemed necessary for control of medically unresponsive IOP of his right eye, we were concerned about the postoperative use of corticosteroid and the possible postoperative exacerbation of CSC. Therefore, we followed him up 3 weeks after cessation of the oral corticosteroid. We also added systemic acetazolamide 250 mg three times a day to his antiglaucoma medications. Thereafter, the subretinal fluid decreased on OCT; however, IOP of the right eye was 22 mmHg. To minimize the amount and duration of postoperative steroid use, trabecular microbypass stent insertion was performed in his right eye.
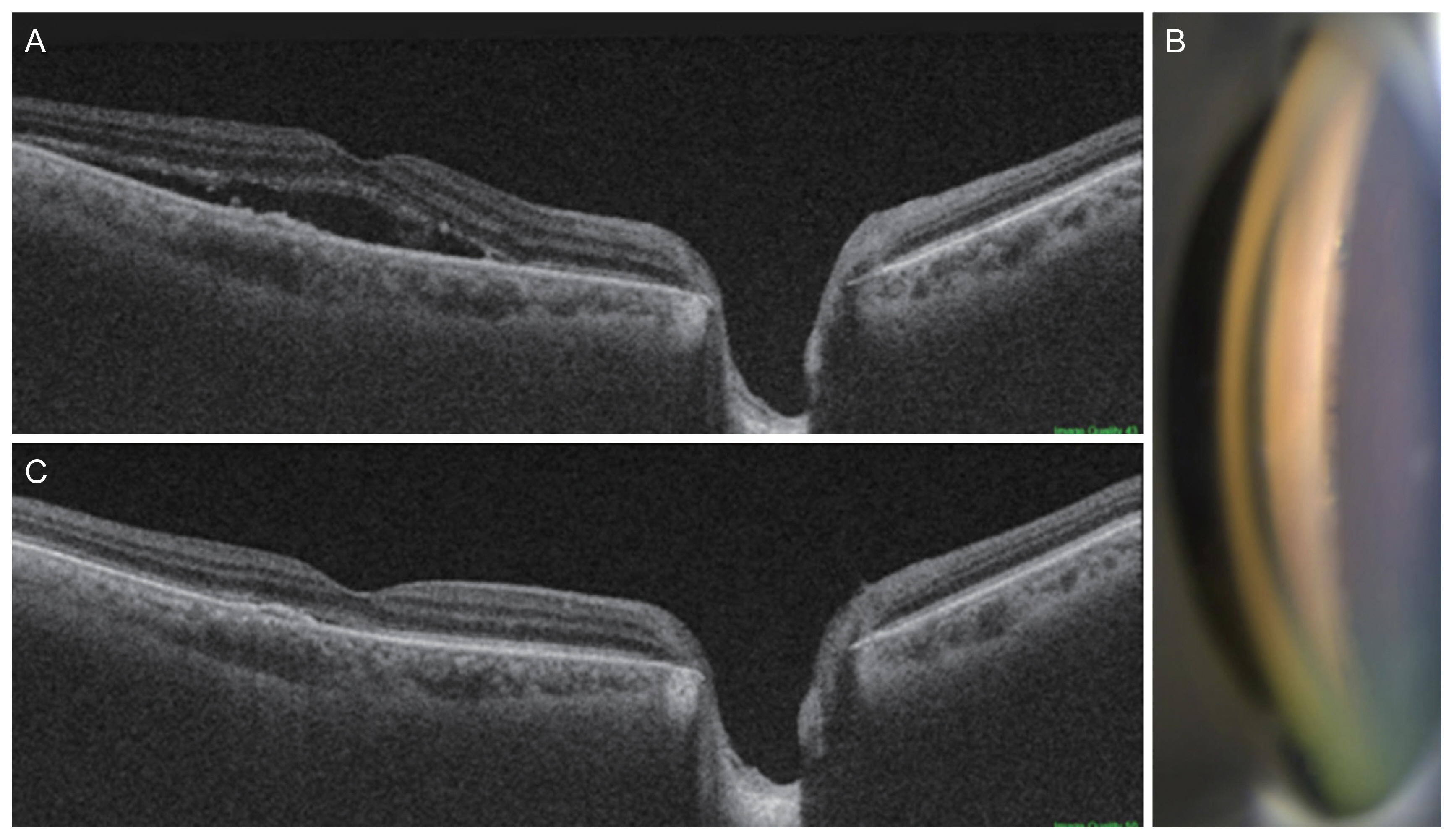
A photo of trabecular microbypass stents in the anterior chamber angle and optical coherence tomography scans of the right eye. (A) Subretinal fluid accumulation is noted on macular optical coherence tomography scan of the right eye. (B) Two trabecular microbypass stents are seen in the nasal angle. (C) Subretinal fluid accumulation decreased at 2 months after the microbypass insertion.
Briefly, under the topical anesthesia a 2.2-mm temporal corneal incision was created in the right eye. After intracameral injection of the Provisc (Sodium hyaluronate 10 mg/mL; Alcon, Seoul, Korea), two iStents (Glaukos, San Clemente, CA, USA) were inserted into at the nasal iridocorneal angle under visualization using a Swan Jacob gonioprism lens (Fig. 1B). His IOP of the right eye was lowered to 11 mmHg at postoperative day 1 and has remained below 17 mmHg with use of two antiglaucoma medications for the next 12 months. Fluorometholone 0.02% (Santen, Osaka, Japan) eyedrop was used four times a day for postoperative 3 weeks. The subretinal fluid of his right macula deceased gradually over 3 months (Fig. 1C).
CSC is a disease where the fluid accumulates in the subretinal space and causes a serous retinal detachment and vision loss. Although its causes are not completely understood, any exposure to exogenous corticosteroids may induce or worsen the CSC. Regarding the ophthalmic use of steroid, a new CSC case and a worsened CSC case were reported after intravitreal steroid use [2,3]. Moreover, Park and Park [4] reported a patient where CSC developed after trabeculectomy. The postoperative steroid use and prior history of CSC in the fellow eye were presumed as predisposing factors for the development of CSC.
Although the MIGS options are generally not superior to the conventional filtering surgery in the IOP-lowering efficacy, their advantages include the less invasiveness, better safety profile, shorter operation time, faster recovery, and easier combination with cataract surgery [5]. Especially the angle-targeted MIGS is more so and requires the shorter duration of exposure to the relatively weaker steroid.
In the present case, the insertion of two trabecular microbypass stents led to the successful control of IOP without exacerbation of the CSC. With short-term exposure to weaker topical steroids compared to the postoperative regimen for trabeculectomy or drainage device implantation, the subretinal fluids decreased gradually with recovery of visual acuity.
In conclusion, the trabecular microbypass stent insertion can be an effective surgical option to treat uncontrolled glaucoma in an eye with CSC. However, a further study of more cases will be necessary to confirm our observations.
Acknowledgements
None.
Notes
Conflicts of Interest: Chungkwon Yoo is a member of the Editorial Board of the Korean Journal of Ophthalmology since 2019. However, he was not involved in the peer reviewer selection, evaluation, or decision process of this article. Otherwise, no other potential conflicts of interest relevant to this article were reported.
Funding: None.