Multiple Evanescent White Dot Syndrome with Submacular Fluid in Dome-shaped Macula Following COVID-19 Vaccination: A Case Report
Article information
Dear Editor,
Multiple evanescent white dot syndrome (MEWDS) is a unilateral inflammatory chorioretinopathy characterized by multiple small white dots scattered at the posterior pole. It is a benign and self-limiting condition that usually occurs in healthy young women [1]. There is an ongoing global pandemic of coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2. Herein we report a case of MEWDS as an ocular adverse effect after BNT162b2 messenger RNA (mRNA) COVID-19 vaccination (Pfizer Inc., Philadelphia, PA, USA). The patient provided written informed consent for the publication of the research details and clinical images.
A 33-year-old healthy female patient visited a local clinic with a 1-day history of a steadily enlarging dark spot over her right central vision and metamorphopsia in the right eye. Notably, she had received her second dose of the BNT162b2 vaccine 6 days before symptom onset. In the right eye, fundus examination revealed multiple gray-white lesions at the posterior pole and nasal and temporal periphery, and optical coherence tomography (OCT) revealed a dome-shaped macula (DSM) with subretinal fluid and interruption of the ellipsoid zone (Fig. 1A, 1B).
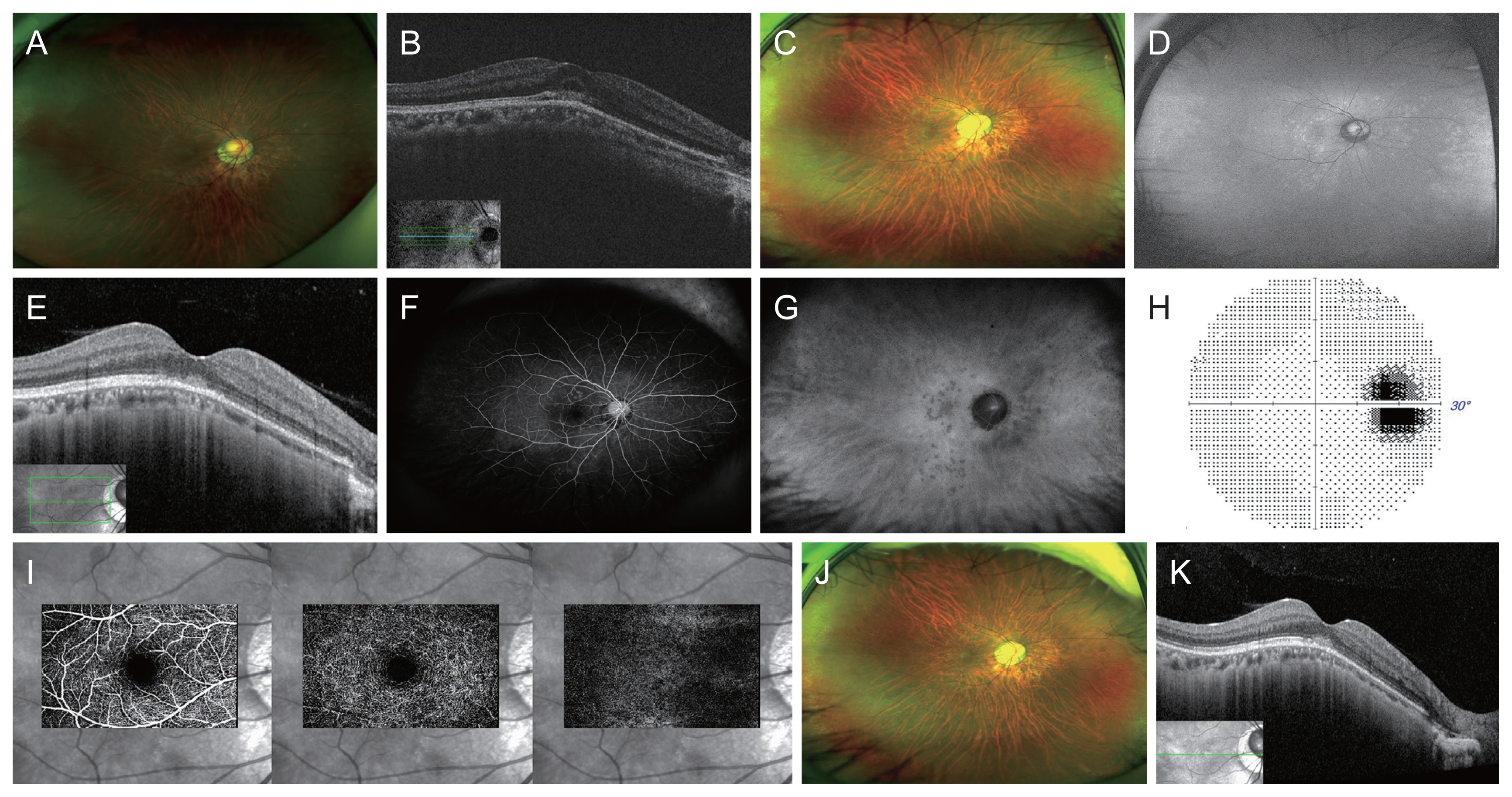
Multimodal imaging findings of the right eye of a patient with multiple evanescent white dot syndrome. On the first visit at a local clinic, (A) a fundus photograph shows multiple gray-white dots at the posterior pole and nasal and temporal peripheral retina and (B) an optical coherence tomography (OCT) image shows a dome-shaped macula with subretinal fluid and interruption of the ellipsoid zone. (C–I) Images 2 weeks later. (C, D) A fundus photograph show that the small gray-white hyperautofluorescent lesions have slightly subsided. (E) An OCT image shows hyperreflective subfoveal material without subretinal fluid and ellipsoid zone disruption. (F) An early-phase fluorescent angiography image shows multiple hyperfluorescent dots in a wreath-like pattern, while (G) a late-phase indocyanine green angiography image shows hypofluorescent dots in areas corresponding to the autofluorescent fundus lesions. (H) Visual field test results reveal an enlarged blind spot. (I) An OCT angiography image does not show a typical neovascular network. (J, K) Ten weeks after initiating oral prednisolone therapy and intravitreal bevacizumab injection. (J) The fundus lesions have regressed further. (K) However, subfoveal hyperreflective material is still observed on the OCT image.
Two weeks later, the patient was referred to Severance Hospital. She revealed that the dark spot become slightly lighter 4 to 5 days after onset, but the metamorphopsia remained. The best-corrected visual acuity was 20 / 40 with spherical equivalents −10.12 diopter in the right eye. Fundus examination revealed regression of the small gray-white hyperautofluorescent lesions at the posterior pole and nasal and temporal periphery (Fig. 1C, 1D). OCT revealed a few vitreous cells, hyperreflective subfoveal material without fluid, and ellipsoid zone disruption (Fig. 1E). Early-phase fluorescein angiography revealed multiple hyperfluorescent dots in a wreath-like pattern, while late-phase indocyanine green angiography revealed hypofluorescent dots in areas corresponding to the autofluorescent fundus lesions (Fig. 1F, 1G). The 30-2 Humphrey visual field test (Humphrey, San Leandro, CA, USA) showed enlargement of the blind spot (Fig. 1H). Choroidal neovascularization was not evident on OCT angiography (Fig. 1I). With the diagnosis of MEWDS, she was prescribed 15 mg of oral prednisone per day, which was tapered over 2 weeks. Additionally, she was administered intravitreal bevacizumab (Avastin, 1.25 mg/0.05 mL; Genentech, South San Francisco, CA, USA) in hopes of hastening her recovery. Ten weeks later, her symptoms improved with increased visual acuity to 20 / 50. The fundus lesions resolved further, but subfoveal hyperreflective material was still observed on OCT (Fig. 1J, 1K).
Recent case studies have shown that MEWDS can occur or recur within a month of COVID-19 vaccination [1,2]. The cause of MEWDS is unknown; both infectious and immune-mediated origins have been proposed. The presence of antecedent flu-like symptoms in approximately half of all affected patients supports an infectious origin [3]. However, the presence of increased levels of circulating immunoglobulins in the acute phase [4] and the occurrence of MEWDS after vaccination support an immune-mediated origin. Vaccine-associated inflammation has been thought to occur via molecular mimicry, direct antigen-mediated cellular and/or humoral immune response, adjuvant-mediated immune response, or activation of common and/or specific loci in genetically predisposed individuals [1]. The COVID-19 vaccine generates the viral spike protein. Therefore, the spike proteins themselves or immune reactions elicited by their presence could trigger inflammatory reactions that could lead to MEWDS. Administration of mRNA vaccines such as the BNT162b2 vaccine can lead to upregulation of type 1 interferon secretion, resulting in an autoimmune response in susceptible patients [2].
Our case was unusual in that multiple focal lesions were present at the posterior pole and at the nasal and temporal peripheral retina, with sparing of the mid-peripheral zone. Another unusual feature was subretinal fluid with a DSM. Serous retinal detachment associated with a DSM in patients with high myopia is a well-known phenomenon, which may be due to retinal pigment epithelium dysfunction. Macular serous retinal detachment rarely occurs in patients with MEWDS; a PubMED search revealed only one such case, in which high myopia with a DSM was also present [5]. Therefore, our patient might have developed submacular fluid due to MEWDS-induced transient dysfunction of retinal pigment epithelium that was already impaired due to a DSM.
The temporal relationship observed in this report suggests an association between MEWDS and COVID-19 vaccination, but a causative association could not be demonstrated. In the scenario of an ongoing pandemic, vaccination against COVID-19 is being carried out globally. Further research is needed to clarify the causal relationship between vaccination and inflammatory diseases, including MEWDS.
Acknowledgements
None.
Notes
Conflicts of Interest: None.
Funding: None.