Visual Performance and Optical Quality after Implantation of a New Generation Monofocal Intraocular Lens
Article information
Abstract
Purpose
To evaluate the performance of two intraocular lenses (IOLs). The new monofocal IOL using a higher-order aspheric optic (Tecnis Eyhance ICB00) was compared to a standard monofocal IOL (Tecnis monofocal ZCB00) of the identical platform and material.
Methods
The medical records of the patients who had undergone cataract surgery with implantation of either the ZCB00 or the ICB00 in the dominant eye from March 2020 to August 2020 and with available data from the 3-month visit were reviewed. Subjects with ocular comorbidities or corneal astigmatism greater than 1.00 diopters were excluded. The uncorrected near, intermediate, distance visual acuity and corrected distance visual acuity were the main outcome measures. Optical quality parameters measured using an optical quality analysis system, clinical records including age, sex, laterality, ocular dominance, and information related to refractory errors was also collected. Parameters related to the refractory errors were all uniformly based on the Barrett Universal II formula.
Results
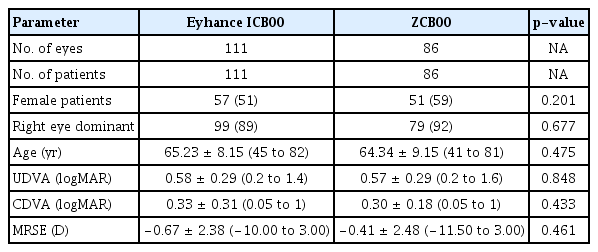
Of the 197 recruited patients, 111 and 86 were implanted with the ICB00 and ZCB00, respectively. No statistically significant differences in baseline parameters were observed between the two groups. While no statistically significant differences in distance visual acuity or optical quality were found between the two groups, compared to the ZCB00 group, the ICB00 group showed significantly higher intermediate visual acuity (p < 0.001) and near visual acuity (p < 0.05) 3 months postoperatively.
Conclusions
ICB00 provided superior intermediate vision and comparable distance performance and photic phenomena compared to a standard monofocal IOL.
Cataracts are a significant cause of visual loss and cataract extraction is the most commonly performed ophthalmic surgery worldwide [ 1,2 ]. More recently, optimal postoperative distance vision has been taken for granted and patients have increasingly higher expectations for cataract removal and correction of presbyopia at the time of cataract operation is increasingly requested by patients [ 3].
Intraocular lens (IOL) technology has advanced in the last decade, with high patient expectations not only for distance but also near and intermediate vision [4]. Since the monofocal lOL provides, by definition, one focus, long-distance glasses or reading glasses were necessary for near or far targets. Intermediate vision tasks include different dai ly life activities such as working on a computer, tablet and phone; playing music or sports; looking at the car dashboard, and walking on uneven surfaces [5]. However, monofocal IOLs are still the most frequently inserted because of their relatively low cost, their outstanding results for far distance, and the low rate of photic phenomena such as halos and glare [3]. In contrast, multifocal IOLs have a high frequency of photic phenomena [6]. To overcome these issues, there is a growing interest in new technology that may improve the intermediate performance of monofocal IOLs and minimize the unwanted photic phenomena of multifocality. More than one-third of patients receiving multifocal IOLs reported often experiencing halos or glare [7]. The newly developed monofocal lens, Tecnis Eyhance ICB00 (Johnson & Johnson Vision, Santa Ana, CA, USA) provides reasonable distance vision as well as aspherical lenses with increased power from the periphery to the center and strengthened intermediate vision [3,8 ].
The objective of this study was to compare the visual outcome and optical qualities of the ICB00 to those of an existing standard monofocal aspheric IOL, the Tecnis ZCB00 IOL (Johnson & Johnson Vision).
Materials and Methods
Subjects
This single-center, retrospective, comparative study was conducted in accordance with the tenets of the Declaration of Helsinki and approved by the institutional review board at Kim’s Eye Hospital, Seoul, Korea (2020-10-001). Due to the retrospective nature of the study, the requirement for informed consent was waived. This study did not include subject identifying information. We thoroughly inspected and carefully reviewed the medical charts of the patients who had undergone cataract surgery with implantation of either of the ZCB00 or ICB00 in their dominant eye between March 2020 and August 2020 at Kim’s Eye Hospital, Seoul, Korea. Overall, this retrospective study included 197 eyes from 197 patients who underwent cataract surgery and who available for the 3-month visit. The ICB00 was implanted in 111 eyes of 111 patients, while the ZCB00 was implanted in 86 eyes of 86 patients.
The main outcome measures were the uncorrected distance (at 4 m) visual acuity (UDVA), uncorrected intermediate (at 66 cm) visual acuity (UIVA), uncorrected near (at 40cm) visual acuity (UNVA), and corrected distance visual acuity (CDVA) at 3 months postoperatively. Optical quality parameters using the optical quality analysis system (OQAS), clinical records including age, sex, laterality, ocular dominance, and information related to postoperative refractory errors were also collected. Parameters related to the refractory errors were all uniformly assessed using the Barrett Universal II formula.
The inclusion criteria were patients aged over 40 years and able to report for follow-up of at least 3 months. The exclusion criteria were relevant comorbidities such as pseudoexfoliation syndrome, corneal pathologies, corneal astigmatism greater than 1.00 diopters (D), previous ocular surgery, ocular trauma, glaucoma, iris disease, retinal problems, nystagmus, and any other ocular pathology that could restrict postoperative visual outcome.
Dominant eye testing
Ocular dominance is the propensity to favor visual input from one eye over the other [9]. Thus, the dominant eye is predominantly used for monocular activities such as sighting through a telescope or microscope [10]. Ocular dominance was determined in this test by applying the hole-in-the-card dominance test (Dolman test), in which the patients were offered a paper with a central circular hole 3 cm in diameter [9]. The patients were requested to hold the paper with both hands and look at a target 6 m away over the hole, with both eyes open. Each eye was then blocked-in turn. When the dominant eye was occluded, the target could not be seen over the hole, while with the nondominant eye being occluded, the dominant eye could see the target over the hole.
Optical quality assessment
The ocular optical quality was assessed using the OQAS (Visiometrics, Terrassa, Spain). This system is based on a double-pass technique that analyzes the visual quality of eyes based on aberration, scatter, and diffraction [11]. The device uses a 4.0-mm pupil to measure the objective scatter index (OSI), the modulation transfer function (MTF) cutoff, and the point spread function (PSF) expressed as the Strehl ratio. The OSl, which indicates the intraocular light scatter, is calculated by sizing the sum of light on the periphery of the double-pass image based on the quantity of light on the center [3]. The MTF is the proportion between the contrast of the image and the object, in terms of the frequency of the object; thus, the MTF cutoff is the spatial frequency at which the MTF falls to zero. The MTF is a useful interpreter of the distance image quality in IOLs [12]. The PSF defines the quality response of an imaging system and is indicated by the Strehl ratio, with a value of 1 indicating a perfect optical system [13]. The Strehl ratio is the proportion between the strength of the real PSF and the diffraction limited PSF [14].
Surgical procedures
All surgeries were performed by two experienced surgeons using a standard phacoemulsification technique through a 2.8-mm clear corneal incision. All the main clear corneal incisions were made at the steepest axis. Topical anesthesia and mydriatic drops were applied before the surgery. After completion of a capsulorhexis with a diameter of approximately 5.2 mm and phacoemulsification, the IOLs were implanted into the capsular bag. The incisions were closed with stromal hydration. A postoperative topical therapy of combined antibiotics (gatifloxacin 0.3%; Gatiflo, Samil, Seoul, Korea) and steroid (fluorometholone 0.1%; Fulleylone, Binex, Busan, Korea) was prescribed to be instillated four times daily for 1 month. All the surgeries ended well without any intraoperative complications and no postoperative problems or side effects were reported.
IOLs
This study assessed two monofocal IOLs (ZCB00 and ICB00) produced by the same manufacturer (Johnson & Johnson Vision). The ZCB00 is a single-piece 6.0 mm biconvex hydrophobic acrylic monofocal IOL with an aspheric anterior surface that results in a negative spherical aberration of −0.27 μm and a translucent, continuous 360-degree posterior square edge [ 12,15 ]. The ICB00 is a newly created monofocal IOL that has equal characteristics to the ZCB00 widely preferred worldwide, except for the modified aspheric anterior surface of the optic [ 16]. This novel optic provides a thickness variance of 1.5 microns with a diameter of about 2 mm in the center and a continuous power profile (a continuous power increase of approximately 0.5 D from the periphery to the center of the lens), which is intended to improve vision for intermediate tasks as compared to a standard monofocal IOL [16]. The ICB00 has no diffractive rings and zones and is visually indistinguishable from the ZCB00 [8].
Statistical analysis
IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. Kolmogorov-Smirnov tests were used to verify the normality of the data samples. Student t-tests and Pearson chi-square tests were used to test the differences between paired data. Paired t-tests were used to compare data before and after surgery in both groups. In all cases, p < 0.05 was considered statistically significant. Data are indicated as means ± standard deviation.
Results
A total of 197 patients were implanted with the ICB00 (n = 111) or the ZCB00 (n = 86) IOL and had available data from their 3-month visit. All the surgeries were conducted by two expert surgeons. Table 1 summarizes the preoperative characteristics of patients by group. No statistically significant differences were found between the two groups in baseline parameters. In the ICB00 group, 51% of the patients (57/111) were women, and the mean age was 65.23 ± 8.15 years. In the ZCB00 group, 59% of the patients (51/86) were women and the mean age was 64.34 ± 9.15 years. In the ICB00 group, 89% of the patients (99/111) were right-eye dominant and the mean UDVA, CDVA, and spherical equivalent (SE) were 0.58 ± 0.29, 0.33 ± 0.31, and −0.67 ± 2.38, respectively. In the ZCB00 group, 92% of the patients (79/86) were right-eye dominant and the mean UDVA, CDVA, and SE were 0.57 ± 0.29, 0.30 ± 0.18, and −0.41 ± 2.48, respectively.
Table 2 shows the 3-month postoperative visual outcomes in the two groups. Distance vision was comparable between the ICB00 and ZCB00 groups at 3 months. The UDVA showed excellent results in both groups (ICB00, 0.11 ± 0.10; ZCB00, 0.10 ± 0.14), with no significant difference between the groups. The CDVA also showed excellent results in both groups (ICB00, 0.04 ± 0.06; ZCB00, 0.03 ± 0.06), with no significant difference between the groups. The UIVA values were 0.24 ± 0.10 and 0.34 ± 0.12 for the ICB00 and ZCB00 groups, respectively, while the UNVA values were 0.46 ± 0.14 and 0.51 ± 0.19, respectively. Compared to the ZCB00 group, both UIVA (p < 0.001) and UNVA (p = 0.038) were significantly higher in the ICB00 group.
In both groups, emmetropia or minimal myopia were targeted in the IOL power calculations using the Barrett Universal II formula. The target SE was −0.21 ± 0.23 D in the ICB00 group and −0.25 ± 0.27 D in the ZCB00 group. The manifest refraction spherical equivalent was −0.22 ± 0.39 D in the ICB00 group and −0.21 ± 0.37 D in the ZCB00 group. The mean error was −0.01 ± 0.35 D in the ICB00 group and 0.04 ± 0.36 D in the ZCB00 group. The mean absolute error was 0.29 ± 0.21 D in the ICB00 group and 0.31 ± 0.20 D in the ZCB00 group. The percentage of refractive outcomes within 0.5 D was 93% in the ICB00 group and 94% in the ZCB00 group. There were no statistically significant differences in these five parameters related to postoperative refractive errors between the two groups.
The defocus curve is an analysis of the visual performance at various levels of defocus corresponding to different watching distances [17]. The defocus curves of each group are shown in Fig. 1. The ICB00 showed a smoother curve with a broader landing zone than those of the ZCB00 along the whole curve. The defocus curve showed that the ICB00 provided a visual acuity equal or better than 0.22 logMAR between defocus levels of +1.00 to −1.50 D.
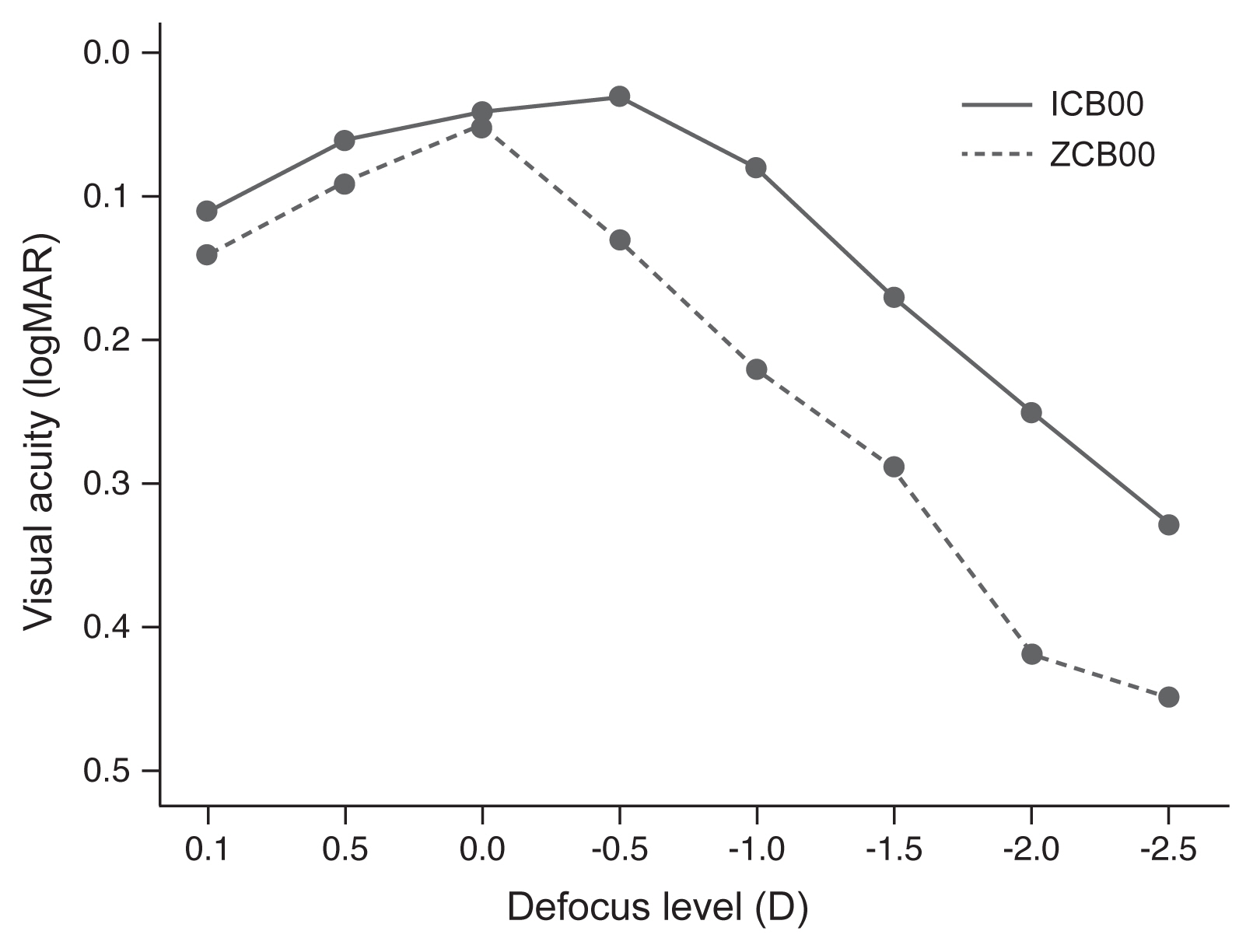
Mean monocular defocus curves obtained in Tecnis Eyhance ICB00 and Tecnis monofocal ZCB00 groups. logMAR = logarithm of the minimal angle of resolution; D = diopters.
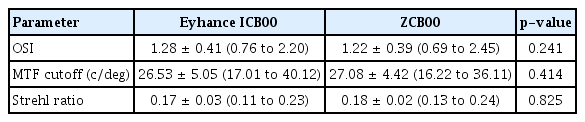
Table 3 shows the optical quality parameters measured by the OQAS for a 4.0-mm pupil. The OSI, MTF cutoff, and Strehl ratio of the ICB00 were 1.28 ± 0.41, 26.53 ± 5.05, and 0.17 ± 0.03, respectively, and 1.22 ± 0.39, 27.08 ± 4.42, and 0.18 ± 0.02, respectively, for the ZCB00. There were no significant differences in these three parameters related to optical quality between the two groups.
Discussion
While multifocal IOLs were designed to provide far, intermediate, and near vision together, possible variations in vision quality may occur due to reduced contrast sensitivi ty and increased photic phenomena [18]. To meet patient’s needs for spectacle independence without a loss in vision quality, new-concept IOLs were developed [19]. In this refractive technology, continuous changes of power in the optic zone are created with higher-order asphericity. The higher-order aspheric monofocal IOLs are intended to provide improved intermediate vision [20]. They are visually indistinguishable from the same platform-standard monofocal lOLs. Their unique anterior surface and a thickness difference of 1.5 microns with a diameter of nearly 2 mm in the optical center enable a power increase of approximately 0.5 D [21]. The increase in power distribution from the periphery to the center enhances the depth of focus and enriches intermediate vision [8].
Previous studies have reported a monocular UIVA of 0.24, 0.26, and 0.28 for the ICB00 and 0.39, 0.40, the 0.45 for the ZCB00 and a monocular UNVA of 0.46, and 0.50 and 0.50, and 0.81, respectively [3,8, 22 ]. In this study, the UIVA values were 0.24 ± 0.10 and 0.34 ± 0.12 and the UNVA values were 0.46 ± 0.14 and 0.51 ± 0.19 for the ICB00 and ZCB00 groups, respectively. Compared to the ZCB00 group, both UIVA (p < 0.001) and UNVA (p = 0.038) were significantly superior in the ICB00 group. In this study, the postoperative monocular UDVA and CDVA results were similar between the ICB00 and ZCB00, consistent with previous reports [3,8,22]. Contrary to previous studies, the present study observed significant differences in near visual acuity between the two IOLs. This might be due to racial differences. While previous studies were conducted on Westerners [3,8,22], this is the first study to be reported on the use of the ICB00 in Asian subjects. As is well known, the prevalence of myopia is far higher in Asians than Westerners [23]. It is reported that the amplitude of accommodation in myopia population is larger than emmetropia or hyperopia population [24].
Previous study has indicated that ICB00 had a greater error range of manifest refraction than ZCB00 postoperatively [3]. However, there was no significant difference between the two groups in our study. The absence of a significant difference in error range of manifest refractions between the two groups in this study may be due to the significant difference in the number of participants. Because of the large number of participants, Student t-tests for comparison were available because the data had a normal distribution.
Monovision is a surgical option that corrects distance vision in the dominant eye while the non-dominant eye focuses for near or intermediate vision [ 25]. This leads to the development of neural adaptation where the brain can use both images to achieve a broader range of functional vision [26]. It is a simple and cost-effective method to become spectacles-independent [27]. In aiming for monovision during cataract surgery, the importance of ocular dominance is highlighted [28]. Previous studies on the ICB00 were conducted on both eyes without distinction between the dominant and non-dominant eye [3,8, 22 ]. However, we compared only one eye from one patient. While research conducted on both eyes may be more meaningful in identifying the need for near glasses, it may be more meaningful to compare one eye to another to evaluate the differences in characteristics between IOLs. In our study, the ratios of right eye dominance in the two groups were 89% and 92%, respectively (Table 1), comparable to the 87.5% and 92% dominance reported previously [ 29,30]. In developing the initial study plan, we tried to determine whether there were any differences in the usefulness of the ICB00 between dominant and non-dominant eyes; however, the ratio of non-dominant eyes was too low to proceed. The results of this study, which was conducted only on the dominant eye, provide a reference for future studies on operations for binocular cataracts with monovision. Future studies are also needed to explore the differences in the depths of focus between dominant and non-dominant eyes in a larger number of participants.
The optical quality describes the image clarity [11]. A major drawback of multifocal IOLs is photic phenomena [6]. Most multifocal IOLs split light into several foci, which decreases the visual quality. The glare incidence rate is reportedly higher for multifocal than for monofocal IOL [11,15, 31]. Moreover, the objective OSI value for multifocal IOLs was significantly correlated with subjective degrees of glare [ 13]. The optical quality measured using the OQAS in our study was comparable between the two groups, based on the OSI, MTF cutoff, and Strehl ratio, consistent with previous reports [3]. However, few studies have analyzed the optical quality in pseudophakic eyes using the OQAS and the contributions of the material and design features of IOLs have not yet been fully characterized [11,15, 16 ]. Higher OSI values have been observed in multifocal IOLs, with mean OSIs of 1.45 in eyes implanted with the ZCB00 and a mean of 2.50 in eyes implanted with the ZMB00 (Advanced Medical Optics, Santa Ana, CA, USA), a multifocal IOL made of hydrophobic acrylic material [ 11]. Furthermore, a significant correlation was observed between OSI values and glare in the multifocal group, indicating that the OSI may be a reliable index for the visual quality of multifocal IOLs. The OQAS values for the ZCB00 and ICB00 did not differ significantly, indicating similar optical qualities between the two IOLs [3,11, 16 ].
The major limitation of this study was its retrospective designs. For more accurate results, a longer-duration prospective study with a larger number of participants is required. Moreover, it would be interesting to compare the ICB00 outcomes to the results obtained for the Tecnis Symfony (Johnson & Johnson Vision) IOL, which is made of the same material as the ICB00 but which has an achromatic echelette design that broadens the range of vision [ 32]. This study was conducted with the results of two operators. Both operators are expert surgeons, and in the same way they make the same size wound on the steepest axis, using the same machine. Nevertheless, it is a limitation because it can cause unnecessary errors in the results.
The major strength of this study is that it included a larger number of participants compared to previous reports on the ICB00, which assessed only 15, 16, and 20 patients who received this implant [3,8, 22 ]. These limited numbers were not sufficient for comparisons of the effects of this IOL, which has just been released. When new IOLs are introduced, research should be conducted on many participants. Therefore, research such as that performed in the present study is essential to determine if the results are reproducible in large numbers of target groups. Moreover, this numerical inferiority required the analysis of statistics by Mann-Whitney U-tests to compare the difference in results between data that did not follow a normal distribution. However, this study applied Student t-tests for comparisons because the data had a normal distribution. Finally, while existing studies were conducted on Westerners, this is the first study to be reported on the use of the ICB00 in Asian subjects.
In conclusion, the ICB00 offered comparable far vision and optical quality with superior intermediate and near vision compared to the ZCB00 in the dominant eye. Thus, the ICB00 is a good choice for improved intermediate and near visual acuities while maintaining a visual quality comparable to that of the standard monofocal IOL.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by the Kim’s Eye Hospital Research Centrer.