Rare Case of Nerve Sheath Myxoma of the Eyelid Misdiagnosed as Mucocele
Article information
Dear Editor,
Nerve sheath myxoma was first described by Harkin and Reed [1] as a rare, myxoid, and loosely cellular benign tumor of peripheral nerve origin. Nerve sheath myxoma usually develops in the extremities, but can rarely be found in the eyelid. Only 10 cases of eyelid nerve sheath myxoma and its similar entities, including neurothekeoma, have been previously reported to our knowledge, but none of these cases were reported in Korea [23]. Thus, here we report the first case of nerve sheath myxoma of the eyelid in Korea.
A 34-year-old male visited our hospital with a recurrent, painless, round and non-movable soft subcutaneous mass on the right upper eyelid near the medial canthus (Fig. 1A). He had undergone two previous excisional procedures, with this being the third recurrence at the same site.
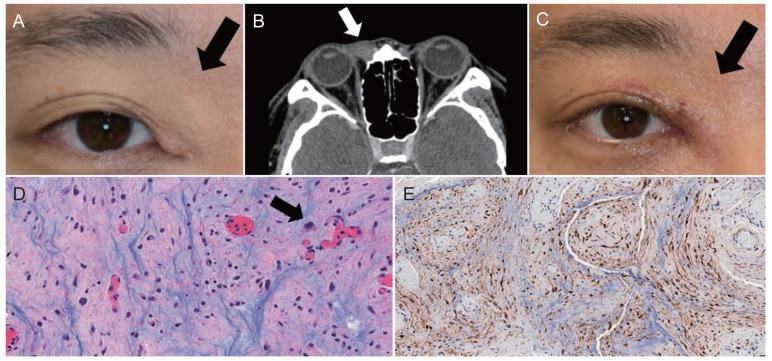
(A) Photograph of the patient's eye at the time of his first visit. A mass (black arrow) at the medial canthus with drooped eyelid skin is observed. (B) Orbit computed tomography image shows an ill-defined enhancing soft tissue lesion (white arrow) at the medial canthal area of the right orbit. (C) Photograph of the patient's eye after complete excision of nerve sheath myxoma. The mass at the medial canthus and drooped eyelid skin had disappeared (black arrow). (D) Histopathologic analysis revealed epithelioid and stellate neoplastic Schwann cells (black arrow) with an abundant myxoid matrix (H&E, ×400). (E) Immunohistochemical staining for S-100 showed a strong positivity (S-100, ×200). Written informed consent from the patient was obtained.
The right medial canthal mass in question first appeared 15 years ago. The initially round, about 5-mm-sized, painless, non-erythematous mass had increased in size over time. He had visited another tertiary center 14 years ago and underwent excision and biopsy. The pathologic diagnosis was “mucocele.” Six years later, an eyelid mass with similar characteristics recurred at the same site and the patient visited another hospital. The orbit computed tomography showed focal, nonspecific increased soft tissue opacity in the medial preseptal area of the right orbit. Two masses sized 1 cm × 0.5 cm × 0.5 cm at the muscle layer were excised; however, the details of the surgical procedure and whether the mass was completely excised or not were not described. The histopathologic diagnosis here was also “mucocele.”
Six months after the excision, a mass reappeared. The patient came to our institute seven and a half years later, during which the mass remained stationary in size. The preoperative orbit computed tomography showed a 1-cm-sized, ill-defined enhancing soft tissue lesion at the right medial canthal area. There were no definite cystic lesions indicating mucocele (Fig. 1B). We excised the right medial canthal mass completely, by dissecting a few lobulated masses from the medial canthal tendon (Fig. 1C). The histopathologic examination revealed that stellate and spindle cells were within a bluish myxoid matrix by fibrous bands. The cells presented a strong positive signal for S-100 immunohistochemical staining, consistent with nerve sheath myxoma (Fig. 1D, 1E).
Nerve sheath myxoma is a myxoid peripheral nerve sheath tumor with a propensity for onset in the extremities and a high local recurrence rate, particularly among patients in their third and fourth decades of life [4]. Nerve sheath myxoma is often misdiagnosed as one of other benign slow-growing eyelid lesions including neurofibroma, chalazion [2], or mucocele as a result of its painless and soft features. Since there are no distinctive clinical symptoms of nerve sheath myxoma, pathological findings are essential in properly diagnosing this condition. Also, it is important that nerve sheath myxoma be distinguished from neurothekeoma. Traditionally, nerve sheath myxoma has been regarded as a myxoid subgroup of neurothekeoma. However, recent studies have shown that nerve sheath myxoma and neurothekeoma are two separate disease entities [5]. Immunohistochemical staining of S-100 is most important for the differential diagnosis of nerve sheath myxoma and neurothekeoma, in that it shows positivity for nerve sheath myxoma and negativity for neurothekeoma [5]. Because nerve sheath myxoma is likely to recur at the same site, complete surgical excision with clear margins is the treatment of choice.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.