Spontaneous Resolution of Macular Hole with Retinal Detachment in a Highly Myopic Eye
Article information
Dear Editor,
Macular hole (MH) with retinal detachment (RD) predominantly occurs in highly myopic eyes, and is a major vision-threatening complication in pathologic myopia [1]. Treatment of MH with RD results in lower anatomic success rates and poorer functional outcomes than MH without RD. Spontaneous resolution of MH with RD is extremely rare; spontaneous resolution of MH without RD is reported more frequently, especially in cases of traumatic MH. However, we encountered a case of spontaneous resolution of MH with RD in a patient with high myopia(Fig. 1A, 1B), which is described herein with a review of the relevant literature.
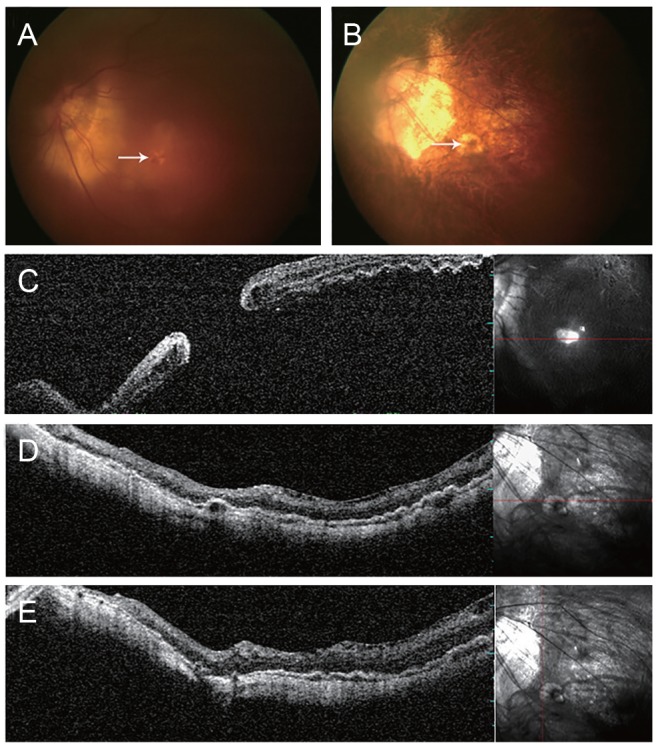
Fundus photographs and optical coherence tomography. (A) Fundus photograph of macular hole (arrow) with retinal detachment. (B) After 2 years, spontaneous resolution of macular hole (arrow) and associated retinal detachment were observed. Atrophic scar change in the fovea was seen on fundus photographs. (C) Macular hole with retinal detachment. (D,E) After 2 years, complete retinal reattachment was observed, without any retinoschisis or macular hole on horizontal- and vertical-view optical coherence tomography.
A 73-year-old female visited our clinic complaining of a decrease in vision in the left eye. Best-corrected visual acuity was 0.8 in the right eye (OD) and 0.04 in the left eye (OS) as measured by a Snellen chart. Optical coherence tomography (OCT; Spectral OCT/SLO, OTI, Toronto, ON, Canada) of the OS confirmed the presence of MH-related RD (Fig. 1C). The patient refused surgical treatment.
The clinical history of the patient included Bechet's disease (5 years before) and bilateral cataract surgery (4 years before). At the time of the surgery, the axial length of the eyes was 27.14 mm (OD) and 28.63 mm (OS). Two years after cataract surgery, Nd-YAG (neodymium-doped yttrium aluminum garnet) capsulotomy was performed in both eyes for after-cataract treatment (posterior capsular opacity after cataract surgery).
The patient visited the clinic for a check-up 2 years after MH with RD was diagnosed. Best-corrected visual acuity was 0.8 (OD) and 0.02 (OS) on the Snellen chart. OCT revealed complete retinal attachment as well as spontaneous closure of the MH in the OS (Fig. 1D, 1E).
Several cases of spontaneous closure of MH with RD have been reported. Min [2] and Tam et al. [3] reported two cases of spontaneous reattachment of RD with MH; however, these cases were reported before the advent of OCT, a useful tool for the diagnosis of MH. Li et al. [4] described a case of spontaneous closure of MH associated with RD in an eye with high myopia, in which macular detachment was observed until the last follow-up visit; they suggested that a decrease in vitreoretinal traction force may induce spontaneous closure of MH. Furthermore, spontaneous closure of MH with retinal reattachment in an eye with high myopia and staphyloma was also reported by Yu et al. [5]. They observed a very small MH (66 µm in diameter), the size of which may have influenced spontaneous closure. Furthermore, the development of macular retinoschisis accompanied by complete retinal reattachment was observed, which was believed to reduce the traction force.
The present case varies from previously reported cases because of the presence of a large MH with complete retinal reattachment and no macular schisis. Although several factors that could have negatively affected prognosis, such as a large MH and the absence of macular schisis, were present in this case, complete retinal reattachment as well as MH closure occurred spontaneously. The underlying mechanism of spontaneous MH closure in this case despite the presence of these negative factors is not fully understood, but spontaneous release of vitreoretinal traction is believed to play a role.
In conclusion, we reported a case of spontaneous resolution of MH with RD in a highly myopic eye, which is unique because of the large size of the MH, complete retinal reattachment, and the absence of macular schisis.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.