Macular Edema after Gabapentin
Article information
Dear Editor,
Gabapentin is an anticonvulsant and has been used to manage neuropathic pain. It was originally developed as an antiepileptic agent; however, it is now recommended as a drug of choice for the treatment of neuropathic pain. There is strong evidence that gabapentin is also effective in diabetic neuropathy and postherpetic neuralgia [1].
To the best of our knowledge, macular edema after use of gabapentin has not been reported to date. Therefore, we report a case of macular edema after gabapentin.
A 71-year-old man presented with a 1 day history of visual disturbance and metamorphosis in both eyes. The patient had taken oral gabapentin (Neurontin; Pfizer, New York, NY, USA) and oral methylprednisolone (Methylon; Alvogen, Seoul, Korea) for 8 days for treatment of postherpetic neuralgia. He had no other significant medical history, except hypertension controlled by oral medication. Best-corrected visual acuity (Snellen) was 0.4 (right eye) and 0.2 (left eye), and the intraocular pressure was 9 mmHg (right eye), 11 mmHg (left eye), as determined by non-contact tonometry. Both eyes had moderate cataract. Ophthalmic examination of the anterior segments revealed no other abnormal findings. Dilated fundus examination and spectral domain optical coherence tomography revealed macular edema and serous retinal detachment of macula in both eyes (Fig. 1A-1D). Fluorescence angiography revealed fluorescein dye pooling on the macula and multiple leakages in both eyes (Fig. 1E and 1F). The patient was advised to discontinue gabapentin, and the use of the drug was stopped.
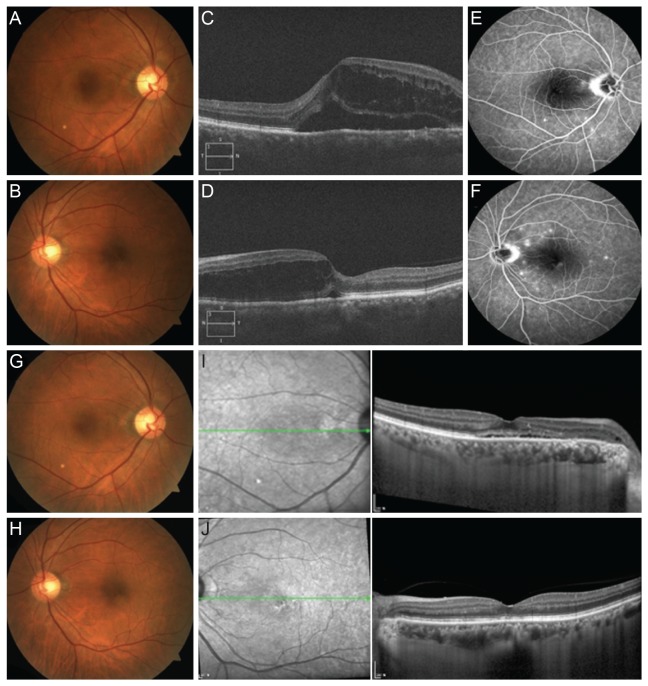
At the initial visit, macular edema and serous detachment on both eyes were observed by fundus photo (A, right eye [OD]; B, left eye [OS]) and spectral domain optical coherence tomography (C, OD; D, OS). On fluorescence angiography, fluorescein dye pooling on the macula and multiple leakages were observed in both eyes (E, OD; F, OS). At 4 weeks after the initial visit, macular edema and serous detachment were much improved on fundus photo (G, OD; H, OS) and spectral domain optical coherence tomography (I, OD; J, OS).
Four weeks after the initial visit, best corrected visual acuity improved to 0.9 (both eye). Fundus exam and spectral domain optical coherence tomography revealed markedly improved macular edema and serous detachment in both eyes (Fig. 1G-1J).
Gabapentin is an amino acid initially designed as a cyclic gamma-aminobutyric acid analogue with action as a gamma-aminobutyric acid agonist [2]. It also acts on different brain receptors by an as-yet unknown mechanism.
Common adverse effects of gabapentin include dizziness, fatigue, drowsiness, sexual dysfunction, weight gain, and peripheral edema [3]. Uncommonly, gabapentin causes blurred vision and diplopia [4]. Steinhoff et al. [5] reported that this drug has been linked with abnormal color perception and reduced contrast sensitivity due to an unknown mechanism. Gabapentin could also cause abnormal finding of visual evoked potentials and pattern electroretinogram [2]. It was suggested that toxic effects on the neuro-transmitter function of the optic nerve might be responsible.
Macular edema on optical coherence tomography after gabapentin has not hitherto been described. Using fluorescence angiography, the present patient was observed to suffer multiple chorioretinitis. Thus, it is possible that the macular edema was due to chorioretinitis. Herpetic infection can also induce chorioretinitis. However, the macular edema in the presented case was spontaneously improved after cessation of gabapentin and steroid, suggesting that chorioretinitis is not a sufficient explanation. Because the precise action mechanism of gabapentin is not known, it is difficult to deduce the mechanism of macular edema after the use of gabapentin. Further studies about the mechanism and frequency of macular edema after gabapentin are required.
In summary, we report macular edema occurring in a male patient receiving gabapentin therapy for postherpetic neuralgia treatment. The macular edema improved after discontinuing the use of the drug. If vision loss after the use of gabapentin occurs, it is prudent to identify macular edema. Gabapentin should be considered one of the potential causes of macular edema.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.