The Correlation between Angle Kappa and Ocular Biometry in Koreans
Article information
Abstract
Purpose
To investigate normative angle kappa data and to examine whether correlations exist between angle kappa and ocular biometric measurements (e.g., refractive error, axial length) and demographic features in Koreans.
Methods
Data from 436 eyes (213 males and 223 females) were analyzed in this study. The angle kappa was measured using Orbscan II. We used ocular biometric measurements, including refractive spherical equivalent, interpupillary distance and axial length, to investigate the correlations between angle kappa and ocular biometry. The IOL Master ver. 5.02 was used to obtain axial length.
Results
The mean patient age was 57.5 ± 12.0 years in males and 59.4 ± 12.4 years in females (p = 0.11). Angle kappa averaged 4.70 ± 2.70 degrees in men and 4.89 ± 2.14 degrees in women (p = 0.48). Axial length and spherical equivalent were correlated with angle kappa (r = -0.342 and r = 0.197, respectively). The correlation between axial length and spherical equivalent had a negative correlation (r = -0.540, p < 0.001).
Conclusions
Angle kappa increased with spherical equivalent and age. Thus, careful manipulation should be considered in older and hyperopic patients when planning refractive or strabismus surgery.
The angle kappa is defined as the angle between the visual line and the pupillary axis. In terms of refractive surgery, a large angle kappa can lead to a decentered ablation, which may produce complications, including decreased safety and an increased likelihood of postoperative irregular astigmatism [1]. Sensory exotropia or esotropia are performed during strabismus surgery to make the eyes appear straight, not to align the visual axes [2]. Thus, the presence of a large angle kappa is of great significance when planning strabismus surgery and should be considered [3].
Slit lamp, synoptophore or Orbscan II topography can be used to measure the angle kappa. It can be influenced by age, sex, refractive error, or strabismus [4,5]. However, there is a difference of opinion on the relationship between angle kappa and factors. Basmak et al. [4] reported that the angle kappa decreased as the refractive error became more negative. Therefore, it is smaller in myopes and larger in hyperopes. However, Hashemi et al. [1] showed that the largest angle kappa values were observed in individuals with emmetropia. These differences might be due to ethnic variations in ocular anatomy [6]. A statistically larger interpupillary distance, which may influence the angle kappa [7], has been observed in black patients compared to white ones. Refractive errors are also statistically different among races. Au Eong et al. [8] estimated that the prevalence of myopia in Singaporean participants (n = 110,236) was 48.5% in Chinese, 34.7% in Eurasians, 30.4% in Indians, and 24.5% in Malays.
Thus, the purpose of the current study was to investigate normative data of angle kappa using Orbscan II measurements and also to estimate the correlation between angle kappa and ocular biometrics (e.g., refractive error, axial length) and demographic features in Koreans.
Materials and Methods
Data from 584 eyes examined between January and June of 2011 were obtained from the Kim's Eye Hospital database, and medical records were reviewed retrospectively. We excluded 148 eyes with a history or signs of previous ocular trauma, anterior segment inflammation, glaucoma, previous ocular surgery, or manifest strabismus. Data from 436 eyes (213 males and 223 females) were included in the study's analyses. This research study was reviewed and approved by the institutional review board of Kim's Eye Hospital, and all procedures conformed to the guidelines of the Declaration of Helsinki. Full ophthalmologic examinations, including best-corrected visual acuity, slit-lamp examination and manifest refraction, were performed.
Angle kappa was obtained with Orbscan II topography (Bausch & Lomb/Orbtek, Rochester, NY, USA). The Orbscan II is a three-dimensional scanning slit topographic device that measures the angle kappa automatically with special software by calculating the distance between the center of the pupil and the center of the Placido ring reflection on the cornea. The latter center represents the axis of sight [4]. We used the spherical equivalent, interpupillary distance (IPD) and axial length to investigate whether correlations existed between the angle kappa and ocular biometric measures. IPD was measured using a millimeter rule and common procedure [9]. The IOL Master ver. 5.02 (Carl Zeiss, Jena, Germany) was used to measure axial length.
Data were analyzed using the SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). Results from quantitative variables were expressed as mean ± standard deviation, and comparisons between males and females were conducted using Student t-tests. The comparison between age and angle kappa were analyzed using one-way ANOVA. Correlations between the angle kappa and ocular biometries were statistically examined using the Pearson correlation test. Statistical significance was defined as a p-value of <0.05.
Results
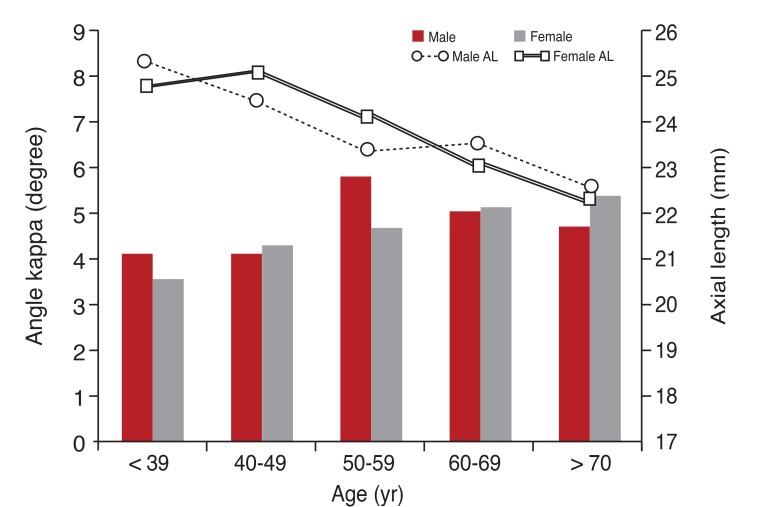
The average patient age was 59.2 ± 12.6 years (57.5 ± 12.0 years in males and 59.4 ± 12.4 years in female participants, p = 0.11). Angle kappa averaged 4.70 ± 2.70 and 4.89 ± 2.14 degrees in male and female patients, respectively (p = 0.48). Normative data of the angle kappa are shown in Fig. 1. Angle kappa was highest in male patients in 50 years of age and in female patients over 70 years of age. After post-hoc analysis, there was a statistically significant difference between men in their 40s and men in their 50s (p = 0.04) and between women less than 40 years old and women more than 70 years old (p = 0.04).
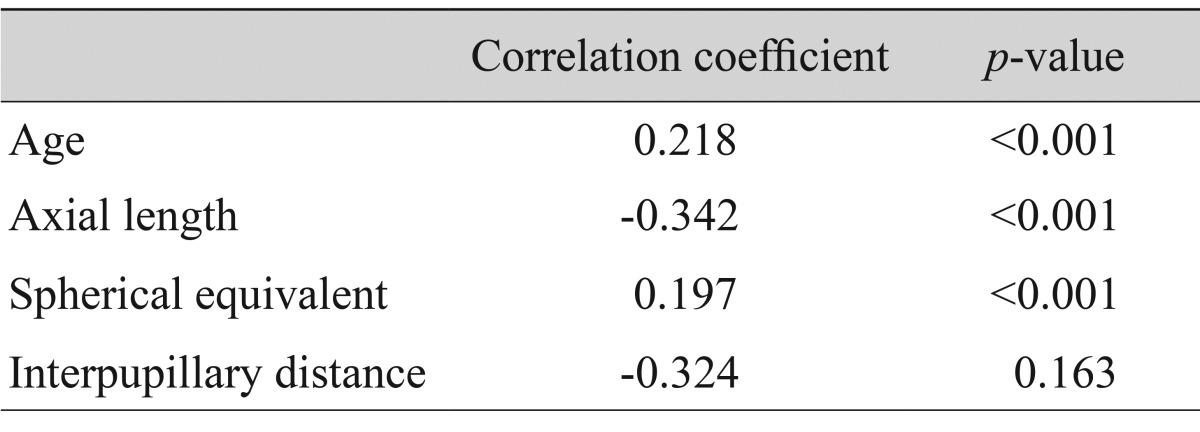
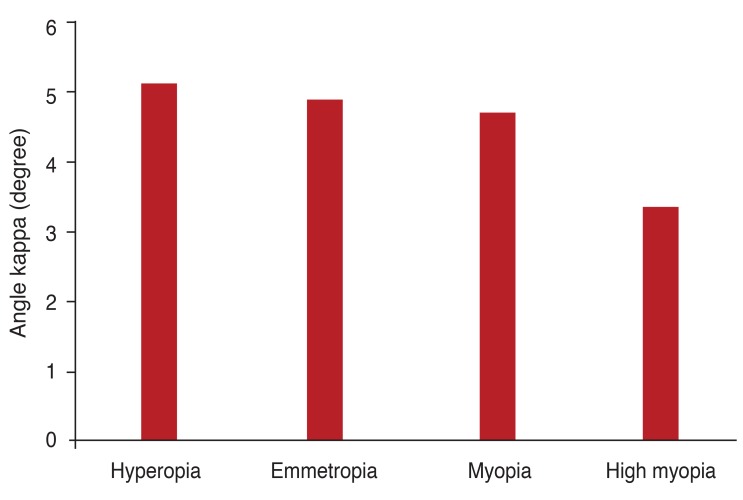
Axial length was correlated with angle kappa (r = -0.342, p < 0.001). Similarly, the spherical equivalent was positively correlated with angle kappa (r = 0.197, p < 0.001) (Table 1). In addition, the correlation between axial length and spherical equivalent had a negative correlation (r = -0.540, p < 0.001). Angle kappa tended to be lowest in high myopes, but there was no statistically significant difference in angle kappa between refractive error groups (ANOVA, p = 0.33) (Fig. 2).
Discussion
This study showed that the angle kappa decreased with axial length and increased with age and spherical equivalent. The angle kappa averaged 4.70 ± 2.70 degrees in men and 4.89 ± 2.14 degrees in women. This finding was somewhat smaller than the values observed in citizens of Tehran, where it was measured as 5.41 ± 1.32 degrees in men and 5.49 ± 1.34 degrees in women [1]. This difference could be due to racial differences in ocular biometric measures. Also, higher rates of myopia have been noted in Far East Asia (including Korea) [8]. This trend could explain why a smaller angle kappa, which decreases with the spherical equivalent, was observed in our study.
The angle kappa was not significantly different among age groups, but significant differences between certain decades were noted. As shown in figure 1, the angle kappa generally increased with age in women, while the largest angle kappa was observed in men in their 50s. The cause of the difference is not certain. However, Fig. 1 illustrates the slight decline of axial length in the 50s in males, and these minimal differences might have influenced the angle kappa value.
A positive correlation between angle kappa and age was noted. Our results differed from those obtained previously by Hashemi et al. [1], who found that the angle kappa decreased with age and that inter-gender differences were not significant. Still, Kahn and Shaw [10] have reported inter-gender differences in biometric measures, and the inferior orbital rim significantly receded laterally in our female population, while male subjects generally had a recession of the entire inferior orbital rim. As a result, the eyeball could shift laterally with age from recession of the inferior orbital rim.
The present results documented that the angle kappa was correlated with the spherical equivalent positively and the axial length negatively. Giovanni et al. [11] suggested that emmetropes and hypermetropes tend to have a larger angle kappa than myopes. Hashemi et al. [1] also presented that angle kappa values were larger in the hypermetropic population compared to the myopic population. Basmak et al. [4] reported that normative values of angle kappa ranged from 4.51 ± 0.11 degrees (right eye of myopic patients) to 5.73 ± 0.10 degrees (left eye of hyperopic participants), according to the refractive status, and the authors speculated that the corneal intercepts of the axes were located closer to the optical axis in myopic eyes and farther away in hyperopic eyes. Interestingly, the present study showed a negative correlation between angle kappa and axial length. It is well known that spherical equivalent is highly correlated with axial length [12], and the present results also had positive correlations. Thus, the current study suggested that myopic changes of the eyeball may induce a decrease of the angle kappa. Lastly, the angle kappa was not significantly correlated with interpupillary distance, despite the relatively correlation coefficient (r = -0.324, p = 0.16).
In conclusion, the mean angle kappa was 4.70 ± 2.70 degrees in men and 4.89 ± 2.14 degrees in women. The angle kappa increased with spherical equivalent and age. Thus, careful manipulation should be considered both in older patients and in hyperopic patients when planning refractive or strabismus surgery.
Notes
No potential conflict of interest relevant to this article was reported.