 |
 |
| Korean J Ophthalmol > Volume 27(4); 2013 > Article |
Abstract
Purpose
To evaluate the clinical usefulness of binocular multifocal electroretinography (mfERG) by comparing results with conventional monocular mfERG in patients with monocular macular disease.
Methods
mfERG testing was conducted on 32 patients with monocular macular disease and 30 normal subjects. An initial mfERG was simultaneously recorded from both eyes with two recording electrodes under binocular stimulation. A second mfERG was subsequently recorded with conventional monocular stimulation. Amplitudes and implicit times of each ring response of the binocular and monocular recordings were compared. Ring ratios of the binocular and monocular recording were also compared.
Results
In the macular disease group, there were no statistical differences in amplitude or implicit time for each of the five concentric rings between the monocular and binocular recordings. However, with binocular simulation, the ring ratios (ring 1 / ring 4, ring 1 / ring 5) were significantly reduced in the affected eye. In the normal control group, there were no statistical differences in any parameters between the monocular and binocular recordings.
Conclusions
Binocular mfERG could be a good alternative to the conventional monocular test. In addition, given that the test needs stable fixation of the affected eye during the binocular test, the reliability of the test results could be improved, especially for patients with monocular macular disease.
The multifocal electroretinogram (mfERG) was developed by Sutter and Tran [1] in 1992. mfERG is useful for the evaluation of localized retinal dysfunction in the posterior pole and has been reported to show sensitivity to several types of macular disease [2-6]. mfERG is a valuable tool not only for the detection of macular dysfunction, but also for following disease progression and evaluation of the effectiveness of treatment modalities used in macular diseases, such as age-related macular degeneration (AMD) [7].
However, as with most electrophysiological techniques, mfERG can be influenced by recording conditions. Minute eye movements can cause noise and significantly influence the results of the recordings. Thus, an mfERG recording is reliant on patient cooperation. In particular, visual fixation during the test, both central and steady, is a major parameter of the reliability of the acquired data [8,9]. In practice, it is difficult for patients, particularly those with poor central visual acuity (VA) due to macular disease, to maintain monocular fixation of the affected eye when the good eye is occluded. In addition, mfERG is primarily useful in evaluation of the functionality of the central retina. Erroneous information can be provided by misinterpretation of recordings due to the possibility of eccentric fixation in patients with macular disease.
The authors hypothesized that, if binocular mfERG can be performed in patients affected by macular disease with poor VA, there will be a gaze change by the affected eye toward the fixation point of the fellow eye. This may lead to a more accurate and steady visual fixation compared with monocular viewing. In this study, we evaluated the clinical usefulness of binocular mfERG by comparing results with conventional monocular mfERG in patients with unilateral macular disease.
This prospective study included 32 patients with a primary diagnosis of wet AMD in one eye and who had previously undergone mfERG in our institution. A standard eye examination was performed prior to the mfERG recording, and none of the subjects had any ocular comorbidity, other than visually insignificant cataract. No history of strabismus was known prior to VA loss due to AMD. Subjects were excluded if they showed heterophoria equal to or greater than 10 prism diopters by the Krimsky test or an alternative cover-uncover test. Both tests were performed for both near and distant vision. In addition, a group of 30 normal individuals served as control subjects. All had a corrected VA of 1.0 logarithm of minimum angle resolution with less than 3 diopters of correction. A standard eye examination was performed to exclude the presence of any ocular abnormalities including anisometropia and heterophoria. The study was performed in full accordance with the standards in the Declaration of Helsinki. The institutional review board approved the research, and informed consent was obtained.
The UTAS E3000 system (LKC Technologies, Gaithersburg, MD, USA) was used for the recording of mfERGs. The stimulus matrix consisted of 61 hexagons displayed on a 17' cathode ray tube (CRT) monitor driven at a 75-Hz frame rate. Prior to testing, pupils of both eyes were dilated fully with 0.1% tropicamide and 2.5% phenylephrine. A ground electrode was attached to the earlobe, and bipolar ERG-jet contact lens electrodes were used for recording. Subjects were placed at a viewing distance of 27 cm, and the height of the chinrest was adjusted so that the subjects' eyes were approximately level with the fixation point at the center of the screen. The hexagons were scaled in an area in order to produce approximately equivalent mfERG amplitudes as a function of eccentricity, and they alternated between black and white according to a binary m-sequence. Unfortunately, in our laboratory, a manual adjustment of the viewing optics for the mfERG instrument is impossible. However, there is some evidence that mfERGs are unaffected by moderate blurring of the retinal image in healthy individuals, if within ±3 diopters [10]. The size of the fixation target was adjusted so that the patient could see the target. This was performed instead of correcting for the near vision refractive error.
There were two separate trials during the recording phase. An initial mfERG was recorded simultaneously from both eyes with two recording electrodes. Subjects were instructed to stare using both eyes at the fixation target on the center of the monitor. The mfERG system was equipped with a video camera, located on the chin rest assembly below and in front of the CRT monitor. The image captured by the camera was displayed on the examiner's computer and allowed real-time visual fixation stability monitoring during the recording. Each recording session consisted of 16 segments of approximately 13.5 seconds each. If the subjects were able to cooperate and maintain good visual fixation, the total recording time was approximately 4 minutes per session. In reality, it took a much longer time for patients with macular disease to complete one session since any recording segments contaminated with an artifact or excessive noise due to poor cooperation or unsteady fixation were discarded and the test repeated. The total time for one session of mfERG recording was measured for each subject. Thirty minutes after the first recording with binocular fixation, a second mfERG test was conducted under conventional monocular viewing conditions. A second trial was performed on the affected eye while the fellow eye was occluded.
In this study, the first-order mfERG kernel was analyzed. Averaged response densities of mfERG from each subject were analyzed by grouping the 61 responses into five concentric rings. Amplitudes and implicit times of each ring response were measured between the first negative trough (N1) and the first positive peak (P1). The results of the binocular and monocular recordings were compared.
Macular diseases, such as AMD, predominantly affect the central or paracentral regions of the visual field. Comparing the electric response of the central part to that of the peripheral regions could enhance disease specific features of the mfERG. Ring ratios were computed as the ratio of the central ring amplitude (R1) to that of the peripheral rings (R1/R2, R1/R3, etc.) [11]. The results of the binocular and monocular recordings were compared.
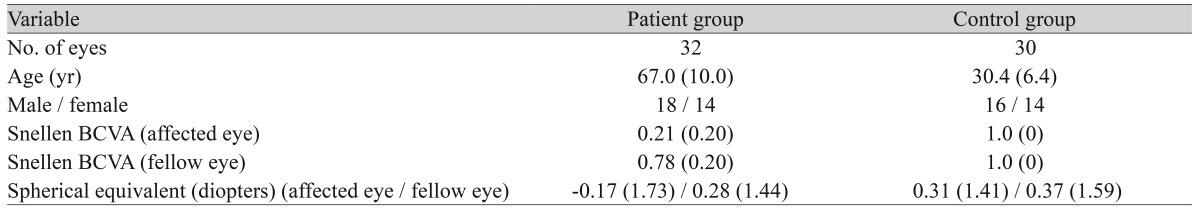
Eighteen women and 14 men were enrolled in the macular disease group. They ranged in age from 51 to 88 years (mean age, 67.0 ± 10.0 years). The mean best-corrected visual acuity (BCVA) was 0.21 ± 0.20 in the affected eye, as measured by the Snellen letter chart, and 0.78 ± 0.20 in the contralateral eye. The spherical equivalent was -0.17 ± 1.73 diopters in the affected eye and 0.28 ± 1.44 diopters in the contralateral eye. The mean age of the control group was 30.4 ± 6.4 years, and all subjects had a BCVA of 1.0 in both eyes. The spherical equivalent in the control group was 0.31 ± 1.41 diopters in the one eye and 0.37 ± 1.59 diopters in the contralateral eye (Table 1).
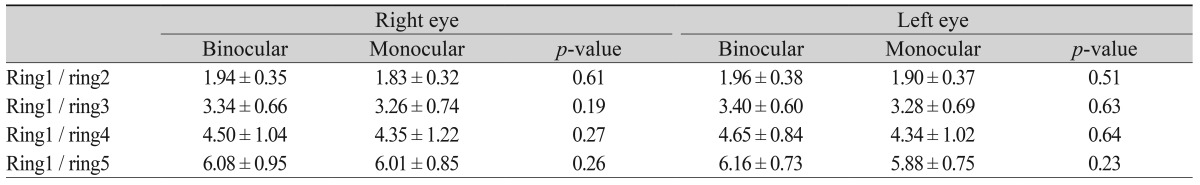
In the normal control group, there were no statistically significant differences in the N1 or P1 amplitudes/implicit times for each of the five concentric rings or in any of the ring ratios (R1 / R2, R1 / R3, R1 / R4, R1 / R5) between the monocular and binocular recordings in both eyes (Tables 2-4).
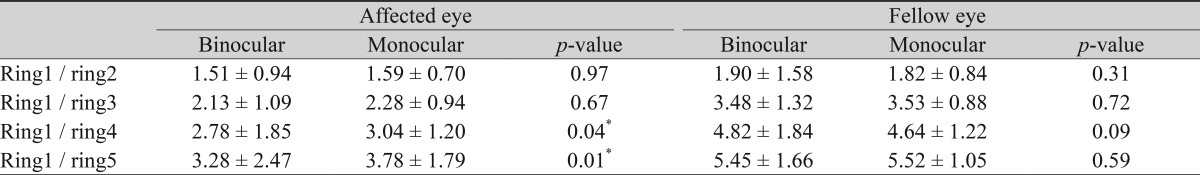
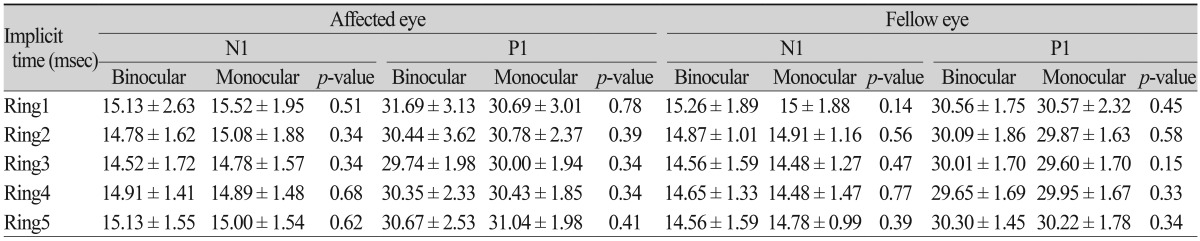
Similarly, in the sound eye for the maculopathy group, there were no significant differences in N1 or P1 amplitudes/implicit times or any of the ring ratios between monocular and binocular viewing. In the affected eye, there were also no statistical differences in N1 or P1 amplitudes/implicit times of each of the five concentric rings. However, with binocular fixation, the ratios of R1 to the most peripheral two rings (R1 / R4 and R1 / R5) were significantly reduced compared with monocular fixation (p = 0.04, p = 0.01) (Tables 5-7).
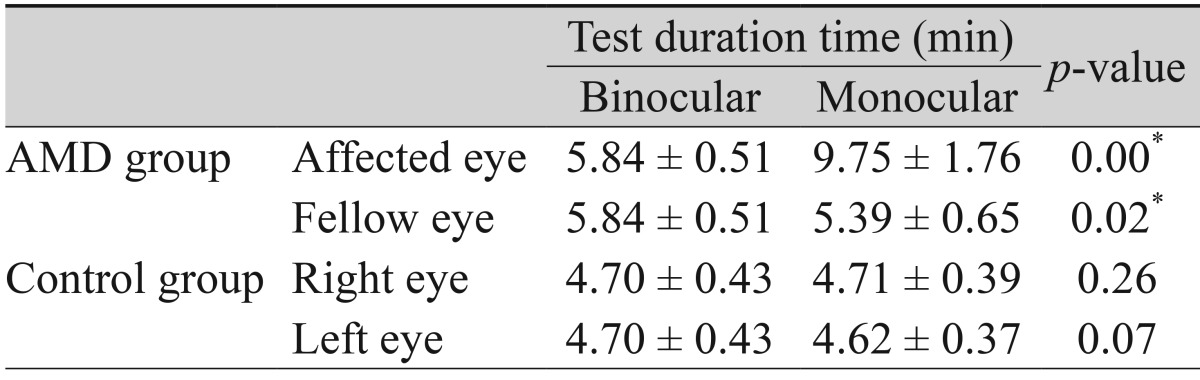
Fixation quality was compared between binocular and monocular viewing. During mfERG testing, none of the subjects showed gross off-fixation under either viewing condition. However, when the affected eyes of subjects with AMD were tested under conventional monocular fixation with occlusion of the sound eye, the noise and/or artifact production was higher than with binocular fixation. Consequently, a significantly longer time was needed to complete one session. The mean test duration for monocular and binocular recording was 9.75 ± 1.76 min and 5.84 ± 0.51 min, respectively (p < 0.01) (Table 8).
mfERG has been used for the assessment of retinal function in various ocular diseases. In particular, it is widely used in clinical practice for the diagnosis of abnormalities in parts of the macula and the paramacular area [2-6]. Furthermore, mfERG can also be useful for the assessment of treatment outcome [7,12,13].
Patient cooperation is essential for mfERG. It is particularly important that patients retain the ability to see the fixation target [14]. However, in patients with macular disease who have difficulty retaining central visual fixation, the anatomical lesion may not correspond to the abnormal area in the mfERG. It is known that, in cases of macular disease, patients may view the fixation target using another retinal area instead of the fovea [15]. This area is called the preferred retinal locus (PRL). In such cases, the results will be based on an eccentric fixation point, and the VA or function of the macula may appear as if it has improved when it actually has not [16].
mfERG with binocular fixation was studied based on the hypothesis that performance of the test with binocular fixation, instead of the conventional monocular fixation, could result in more reliable data due improved central fixation by the patient and better patient cooperation. A binocular test can be more helpful than a monocular test especially in the event of gazing using the PRL in patients with macular disease. Kabanarou et al. [17] observed a difference in the gazing direction for each eye between monocular and binocular tests in patients with AMD. They also found that, when using binocular fixation, the eye with poor VA follows the gazing direction of the eye with good VA.
Results of this study showed that there was no significant difference between binocular and monocular tests in the mean of amplitude or implicit time of each ring. There was also no difference in the ring ratio in either eye of the normal control group and in the non-affected eyes of the macular disease group. The binocular test did not differ significantly from the monocular test in the analysis of current general indicators. Furthermore, better patient cooperation with binocular testing can reduce testing time. Therefore, binocular testing can be a good option for patients who cannot maintain steady monocular fixation due to macular disease.
Contrary to the authors' expectation, there was no significant difference between binocular and monocular tests in regard to the amplitude or peak latency for each ring in the affected eye in the macular disease group. This could be due to increased artifacts resulting from poor fixation. Up to 30% variation in the amplitudes obtained from mfERG of normal eyes has been reported due to the effect of artifacts [18]. Standardization by grouping the amplitudes of each of the 61 hexagons into five rings can reduce this effect. As ring1 consisted of only one hexagon located at the fixation center, variation in this ring was likely to be high. In addition, this could be due to the fact that locations of the lesions varied by patient and ranged from ring1 to ring3.
Another possible cause was that parafoveal fixation was used. In a recent study of patients with macular disease who had decreased VA, Crossland et al. [15] reported that most of the patients developed a PRL within six months. The location of the PRL varied across patients and was difficult to predict. In addition, while the fixation target was being projected, it was observed that the fixation point on the retina showed minute movements following several PRLs. Thus, even among patients with eccentric fixation in this study, the summation and averaging analyses of amplitude and implicit time of each ring did not differ significantly between the binocular and monocular tests. This is possibly because the location of the so-called pseudofovea varied across patients, and minute movement was possible while observing the fixation target.
Analysis of the ring ratios showed a slightly different pattern. Ring ratios were defined as the ratios of the central ring's electric response to the electric response of each of the peripheral rings [11]. Very few studies have used this index in the analysis of mfERG results even though analysis of the ring ratios on mfERG has several benefits [11,19,20]. The amplitude, the response density of each ring generally used in the analysis, decreases with age, while the ring ratios are generally constant and are not significantly influenced by age [11,21]. In addition, ring ratios are less influenced by the condition of the stimuli [22], the location of the reference electrode [23], and the condition of the anterior segment of the eye, such as a cataract [24]. All these reasons make the ring ratio a useful indicator of reduced variation in the test results.
In this study, analysis of the ring ratios showed that there was no significant difference between either eye of the normal control group in the binocular and monocular tests. R1 / R2 and R1 / R3 of the affected eyes also did not differ significantly between the binocular and monocular tests. This could be because the averages of R1 / R2 and R1 / R3 did not reflect an actual difference due to the variable lesion locations by patient, ranging from ring 1 to ring 3. The R1 / R4 and R1 / R5 in the affected eyes were significantly decreased in the binocular test compared to the monocular test (p = 0.04 and p = 0.01) (Table 6). This finding indicates that the binocular test more specifically showed the decreased response of the central retina than of the pericentral areas via analysis of the ring ratios compared with the conventional monocular test. This is most likely due to improved patient cooperation and good maintenance of gazing at the fixation center.
In terms of the reduction in test time, the usefulness of the binocular test can be considered. The benefit of reduction in testing time for the binocular test is not merely arithmetic. Since better patient cooperation and stable fixation were possible with the binocular test, the resulting reduction in artifacts allowed for a shorter time required to completely test the 16 segments than in the monocular test. The actual time required to complete the binocular test was more than two times shorter than that for the monocular test. The binocular test would make it easier to assure patient cooperation and to reduce the burden of repetitive tests for both physicians and patients.
One important thing to consider when using binocular recordings is that the patient's eyes should be aligned. It is difficult to apply the binocular test when a patient has heterophoria or heterotropia. The ocular alignment for both near and distance fixation should be checked by a cover test before performing the mfERG. In addition, when both eyes are tested simultaneously, care must be taken to ensure that the distance between the recording electrodes for both eyes is sufficient in order to minimize electric interference.
This study showed that the binocular test of mfERG did not differ significantly from the monocular test in analysis of current general indicators. Therefore, binocular mfERG could be a good alternative to the conventional monocular test. In addition, especially for patients who have monocular macular disease, given that the fixation point of the affected eyes moves toward the fixation point of the non-affected eyes during the binocular test, the reliability of the test results could be improved.
REFERENCES
1. Sutter EE, Tran D. The field topography of ERG components in man. I. The photopic luminance response. Vision Res 1992;32:433-446.


2. Ahn YS, Park TK, Ohn YH, Gwak HW. Multifocal electroretinogram abnormalities of central serous chorioretinopathy. J Korean Ophthalmol Soc 2003;44:2265-2277.
3. Kang JH, Choi ES, Yoon JM, Yoon HS. Multifocal electroretinogram before and after epiretinal membrane surgery. J Korean Ophthalmol Soc 2008;49:104-110.

4. Kim DK, Park TK, Ohn YH. Changes of multifocal electroretinograms after macular hole surgery. J Korean Ophthalmol Soc 2005;46:1351-1360.
5. Lee KH, Chang MH, Ahn JH. Correlation between multifocal electroretinography and visual acuity after resolution of diabetic macular edema. J Korean Ophthalmol Soc 2010;51:29-34.

6. Sung MS, Park TK, Lee JH, Ohn YH. A correlation with retinal thickness using retinal thickness analyzer and the responses of multifocal electroretinogram in patients with diabetic macular edema. J Korean Ophthalmol Soc 2006;47:1401-1409.
7. Karanjia R, Eng KT, Gale J, et al. Electrophysiological effects of intravitreal Avastin (bevacizumab) in the treatment of exudative age-related macular degeneration. Br J Ophthalmol 2008;92:1248-1252.


8. Chisholm JA, Keating D, Parks S, Evans AL. The impact of fixation on the multifocal electroretinogram. Doc Ophthalmol 2001;102:131-139.


9. Winn BJ, Shin E, Odel JG, et al. Interpreting the multifocal visual evoked potential: the effects of refractive errors, cataracts, and fixation errors. Br J Ophthalmol 2005;89:340-344.



10. Hood DC, Bach M, Brigell M, et al. ISCEV standard for clinical multifocal electroretinography (mfERG) (2011 edition). Doc Ophthalmol 2012;124:1-13.

11. Lyons JS, Severns ML. Detection of early hydroxychloroquine retinal toxicity enhanced by ring ratio analysis of multifocal electroretinography. Am J Ophthalmol 2007;143:801-809.


12. Maturi RK, Bleau LA, Wilson DL. Electrophysiologic findings after intravitreal bevacizumab (Avastin) treatment. Retina 2006;26:270-274.


13. Palmowski AM, Allgayer R, Heinemann-Vernaleken B, Ruprecht KW. Influence of photodynamic therapy in choroidal neovascularization on focal retinal function assessed with the multifocal electroretinogram and perimetry. Ophthalmology 2002;109:1788-1792.


14. Chu PH, Chan HH, Leat SJ. Effects of unsteady fixation on multifocal electroretinogram (mfERG). Graefes Arch Clin Exp Ophthalmol 2006;244:1273-1282.


15. Crossland MD, Culham LE, Kabanarou SA, Rubin GS. Preferred retinal locus development in patients with macular disease. Ophthalmology 2005;112:1579-1585.


16. Ishiko S, van de Velde F, Yoshida A. Paradoxical improvement of visual acuity in macular disease. Curr Eye Res 2010;35:651-656.


17. Kabanarou SA, Crossland MD, Bellmann C, et al. Gaze changes with binocular versus monocular viewing in age-related macular degeneration. Ophthalmology 2006;113:2251-2258.


18. Gundogan FC, Sobaci G, Bayraktar MZ. Intra-sessional and inter-sessional variability of multifocal electroretinogram. Doc Ophthalmol 2008;117:175-183.


19. Tuzson R, Varsanyi B, Vince Nagy B, et al. Role of multifocal electroretinography in the diagnosis of idiopathic macular hole. Invest Ophthalmol Vis Sci 2010;51:1666-1670.


20. Lyons JS, Severns ML. Using multifocal ERG ring ratios to detect and follow Plaquenil retinal toxicity: a review. Review of mfERG ring ratios in Plaquenil toxicity. Doc Ophthalmol 2009;118:29-36.


21. Friedman DS, O'Colmain BJ, Munoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 2004;122:564-572.


22. Raz D, Seeliger MW, Geva AB, et al. The effect of contrast and luminance on mfERG responses in a monkey model of glaucoma. Invest Ophthalmol Vis Sci 2002;43:2027-2035.

Table 2
Mean amplitude of N1 and P1 according to the five concentric rings in the normal control group
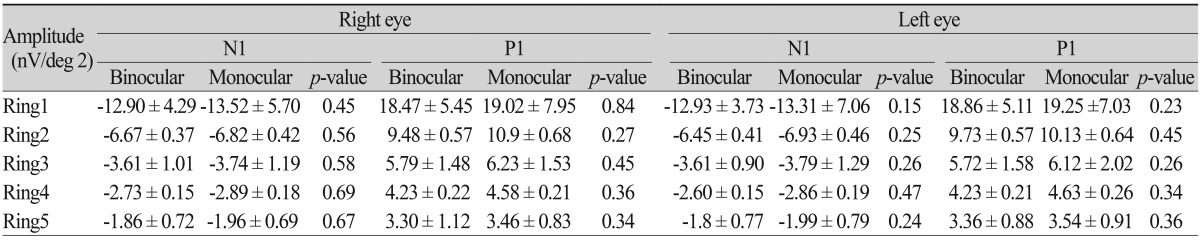
Table 4
Mean implicit time of N1 and P1 according to the five concentric rings in the normal control group
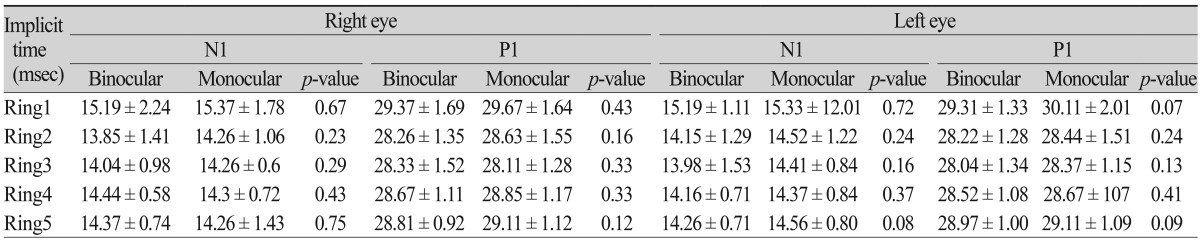
Table 5
Comparison of N1 and P1 amplitude between the monocular and the binocular recordings of the affected eye and fellow eye in patients with unilateral age-related macular degeneration
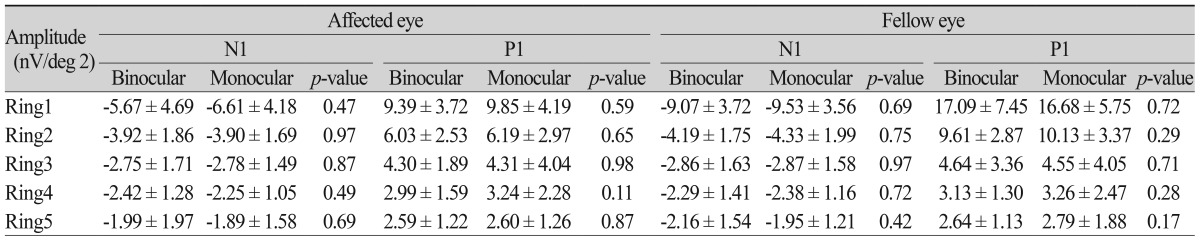
Table 6
Comparison of ring ratios between the monocular and the binocular recordings of the affected eye and the fellow eye in patients with unilateral age-related macular degeneration
- TOOLS



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




