Scleral ischemia and melting can occur in severe cases of chemical or thermal burns, and after ocular surgeries such as a bare sclera pterygium excision with mitomycin C (MMC) application [1]. We describe a patient who developed scleromalacia after undergoing a regional conjunctivectomy using the bare sclera technique, followed by the application of postoperative MMC.
Case Report
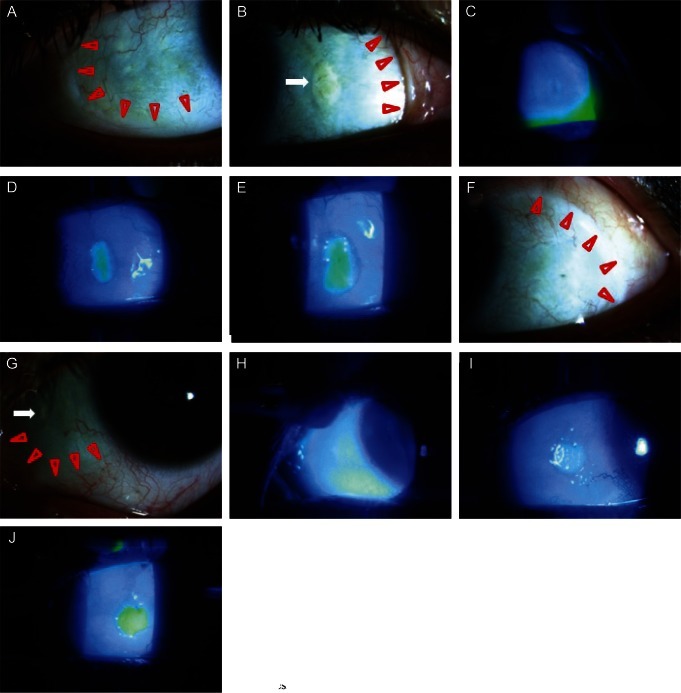
A healthy 40-year-old woman visited our clinic with complaints of ocular discomfort in both eyes. There was no documented history suggestive of connective tissue disease or any systemic disease. Six months prior to this presentation, she had undergone a bilateral regional conjunctivectomy to treat a chronic hyperemic conjunctiva. Following this procedure, she was started on a regimen of 0.2 mg/mL (0.02%) MMC eye drops four times daily for 5 days. The patient's best-corrected visual acuity was 20 / 25 in both eyes. Based on the results from the slit-lamp examination, the conjunctiva and Tenon's capsule on the nasal and lateral bulbar area were excised. Slit-lamp examination also revealed marked scleral thinning and a bluish hue due to seeing the underlying choroid layer which measured 8 ├Ś 4 mm in the temporal portion of her right eye and 8 ├Ś 3 mm in the temporal portion of her left eye (Fig. 1A and 1F). There were a 3 ├Ś 1.7 mm sized yellowish-white calcified plaque on the nasal bulbar conjunctiva of her right eye and a 1.5 ├Ś 0.5 mm sized yellowish-white calcified plaque on the nasal bulbar conjunctiva of her left eye (Fig. 1B and 1G). In addition, we found that the bare sclera was covered with a thin abnormal membranous tissue. There were no fluorescence stained lesions overlying the membranous tissue in either of her eyes (Fig. 1C and 1H). She began conservative treatment with antibiotics and artificial eye drops. The condition of the calcified plaque seemed to stabilize over the course of the next several weeks, and the area of scleral melting did not show any further deterioration. However, there was a newly developed fluorescence stained lesion on the calcified plaques (Fig. 1D and 1I). Fifteen months later, the thinned scleral area and fluorescence stained lesions showed no significant interval change (Fig. 1E and 1J). Because the scleral melting did not show any further deterioration during the following fifteen months, and aggressive surgical intervention might not have been helpful for improving her lesions, we decided to continue regular follow-ups and non-surgical treatment.
Discussion
Chronic hyperemic conjunctiva may cause cosmetic problems. A few surgeons in Seoul, Korea have performed conjunctival excision surgery only for the purpose of cosmesis. These procedures were performed using a bare sclera technique followed by the application of postoperative 0.02% MMC. The 'regional conjunctivectomy' involves the complete removal of the episcleral tissue, including the episcleral vasculature, leaving the scleral bed in an avascular state. We believe that excessive cauterization of the sclera, which is the procedure that is performed to remove engorged episcleral vessels and to stop bleeding during surgery, might promote this avascular state. When the choroid is exposed, operative therapy for the scleral defect area is required because the risk of a secondary infection is high and the ocular contents may become prolapsed with minor trauma. Disruption of the normal conjunctiva and episcleral vasculature may lead to difficulties in other ocular surgeries such as squint, encirclage and glaucoma surgery.
In addition to pterygium surgery, MMC has been successfully applied during various ocular surgeries as an anti-proliferative agent, including surgeries for glaucoma [2] and ocular surface neoplasia [3]. Although the complication rate associated with MMC application is low, these complications can include corneal melting, scleral melting, endophthalmitis, necrotizing scleritis with or without inflammation, and corneoscleral perforation [1,4-6]. Wan Norliza et al. [4] reported a case of scleral melting that presented 16 years after a pterygium excision procedure with postoperative adjuvant topical MMC. Till date, there is no consensus on the optimal operative technique or dose of MMC for patients with chronic hyperemic conjunctiva. As we reported, the complication of regional conjunctivectomy with adjuvant topical MMC can occur in healthy young women. Therefore, we recommend that surgeons should be exceedingly judicious when using MMC for the treatment of various conjunctival surgeries.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






