Evaluation of Plasma Vitamin A and E Levels and Tear Film Changes in Patients with Psoriasis Vulgaris
Article information
Abstract
Purpose
To evaluate whether alterations in plasma vitamin A and E levels in patients with psoriasis have an effect on tear film changes.
Methods
Sixty-two eyes of 31 patients with psoriasis vulgaris (Group A) and 74 eyes of 37 age- and gender-matched control subjects (Group B) were included in the study. Ocular and medical histories and dietary habits were obtained from each patient. The tear film break-up time (TBUT), the Schirmer 1 test results and plasma vitamin A and E levels were evaluated.
Results
The mean Schirmer 1 test score was 14.76 ± 6.12 mm/5 min in Group A and 15.69 ± 3.10 mm/5 min in Group B. The mean plasma levels of vitamins A and E in Groups A and B were 1.86 ± 0.62 µmol/L and 1.88 ± 0.65 µmol/L vs. 26.21 ± 5.13 µmol/L and 27.19 ± 8.89 µmol/L, respectively. The Schirmer 1 test results and plasma vitamin A and E levels were not found to be significantly different between the groups (p > 0.05). The mean TBUT was 9.94 ± 6.18 seconds in Group A and 14.47 ± 5.65 seconds in Group B, a significant difference (p < 0.05). No correlation existed between plasma vitamin A and E levels, TBUT or the severity and duration of the disease (p > 0.05).
Conclusions
Plasma vitamin A and E levels do not seem to be related to tear film changes in patients with psoriasis vulgaris.
Psoriasis is a hyperproliferative chronic inflammatory skin disease of unknown etiology. Erythematous plaques resulting from increased keratinocyte proliferation and abnormal differentiation are the characteristic findings. Ocular manifestations, such as uveitis, blepharitis, conjunctivitis, keratitis, cataracts, orbital myositis and keratoconjunctivitis sicca are observed in about 10% of patients with psoriasis [1].
Vitamins A and E, essential fat-soluble vitamins, have an important role in ocular health. The former is required for normal differentiation and maintenance of mucosal epithelium. In vitamin A deficiency, loss of conjunctival goblet cells causes a reduction in the mucin layer of the tear film, and the mucosal epithelium undergoes metaplasia to form keratinized squamous epithelium [2]. Vitamin A is also a component of tears and performs a vital role in ocular surface health [3,4]. Systemic vitamin A level affects its concentration in tears [4,5]. Mucin is secreted by conjunctival goblet cells, and systemic deficiency of vitamin A is the most common cause of mucin deficiency.
In addition to its antioxidant effect, vitamin E is important in membrane stabilization and has been shown to prevent changes in the ocular surface due to vitamin A deficiency [2]. Although some studies have proposed that decreased plasma levels of vitamin A (retinol) or its precursors (beta carotene) and vitamin E (α-tocopherol) have an important role in the development of psoriasis, controversy persists regarding the contribution of vitamins A and E to the pathophysiology of psoriasis [6-9].
Patients with psoriasis may develop dry-eye secondary to conjunctivitis or decreased aqueous layer production as a result of lacrimal gland involvement [10]. The tests most commonly used to evaluate tear film changes in clinical practice are tear break-up time, Schirmer 1 test, and corneal and conjunctival staining with fluorescein and Rose Bengal dye [11-13]. The Schirmer1 test is used to measure tear production, and tear film stability is determined by tear film break-up time (TBUT) [14]. Abnormal mucin and lipid components may cause dry-eye even if the quantity of aqueous tear production is normal [15]. As a result, most clinicians perform both tests to evaluate different components of tears. Tear film and conjunctival changes in this group of patients have also been studied. TBUT has been shown to be decreased, and squamous metaplasia of the conjunctival epithelial cells has been observed [1,11].
Because altered tear mucin content and squamous metaplasia of the conjunctival epithelia as a result of vitamin A deficiency can be influential factors in the development of the changes mentioned above, we have evaluated the tear film changes and plasma levels of vitamin A and vitamin E as they are important circulating factors that maintain normal epithelial differentiation in patients with psoriasis.
Materials and Methods
Sixty-two eyes of 31 patients with psoriasis vulgaris (Group A) and 74 eyes of 37 age- and gender-matched control subjects (Group B) were included in the study. The inclusion criteria required biopsy-proven diagnosis of the chronic plaque-form of psoriasis vulgaris. The Psoriasis Area and Severity Index (PASI) score and duration of the disease were also recorded. Ocular and medical histories and dietary habits were obtained from each patient. Exclusion criteria included any condition or disease that could affect the tear film, meibomian gland function and/or vitamin A metabolism. These conditions encompass blepharitis, the use of contact lenses, malabsorptive and liver diseases, chronic alcoholism, bizarre eating habits, and the use of retinoids, oral contraceptives, immunosupressive agents, ultraviolet phototherapy, or psoralen plus UV A within 3 months of participation in the study. The study was conducted according to the guidelines of the Declaration of Helsinki, and the patients gave written informed consent after the nature and purpose of the study had been fully explained.
The TBUT and Schirmer 1 tests were evaluated an hour after a full ophthalmologic examination. All examinations were evaluated by the same one examiner (HDD). The TBUT was measured after a fluorescein strip was moistened with sterile saline and applied to the tarsal conjunctiva. Subjects were instructed to blink, and the tear film was examined using the cobalt blue filter of a slit-lamp biomicroscope. The time interval in seconds between the instillation of fluorescein and the appearance of the first randomly distributed dry spot was recorded as the TBUT. This procedure was repeated three times for each eye, and the average of the results was recorded as the mean TBUT.
The Schirmer 1 test was performed without anesthesia by placing a standardized strip of filter paper in the lateral cantus away from the cornea. Data were expressed in millimeters after 5 minutes of wetting. In the morning after an overnight fasting, a 2-mL venous blood sample was collected in tubes coated with EDTA, which were then centrifuged to obtain plasma (9.000 g/10 min at 4℃). Fifty microliters of supernatant were used for high pressure liquid chromatographic examination (Agilent 1100 series analyzer; Agilent Technologies, Waldbronn, Germany), and simultaneous analysis of vitamins A (retinol) and E (α-tocopherol) was performed (Chromosystems Instruments & Chemicals GmbH, Munchen, Germany) at different wavelengths.
The parameters were compared using a t-test for independent samples. The Mann-Whitney U-test was used when data were not normally distributed. A Pearson correlation coefficient was applied to the variables. Statistical significance was defined as p < 0.05.
Results
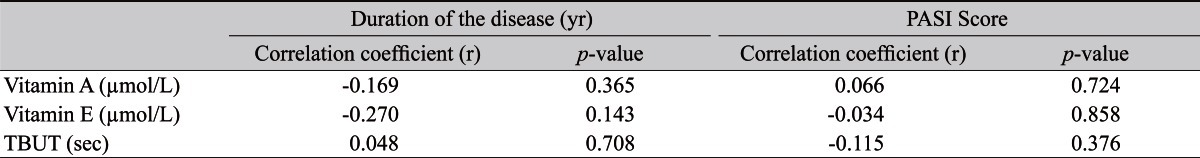
There was no statistical difference for age or gender between Groups A and B (p > 0.05) (Table 1). PASI scores and the duration of the disease are summarized in Table 1. The Schirmer 1 test results were not statistically significant between the two groups (p > 0.05), but significant differences were detected in the TBUT estimates (p < 0.05) (Table 2). No significant intergroup differences were demonstrated in plasma vitamin A and E levels (p > 0.05) (Table 1). Additionally, no correlation was found among plasma vitamin A and E levels, TBUT and the severity and duration of the disease (p > 0.05) (Table 3).
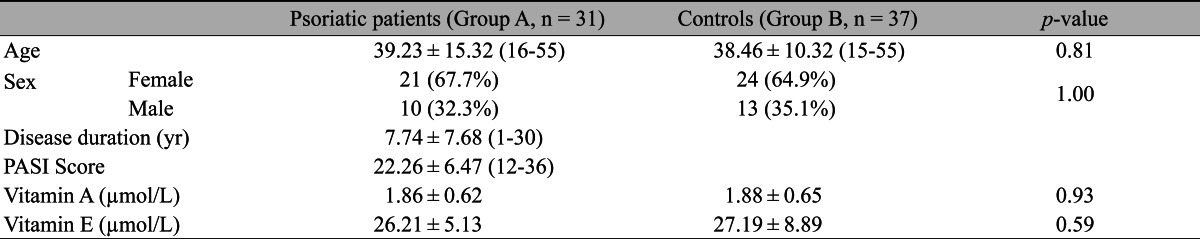
Comparative evaluation of demographic data, disease activity, duration of the disease, and mean plasma vitamin A and E levels of the study participants
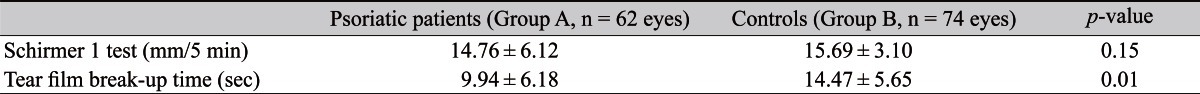
The mean tear film break-up time and Schirmer 1 test results in patients with psoriasis and controls
Discussion
Psoriasis vulgaris is characterized by epidermal hyperproliferation and abnormal differentiation [6]. Although it may affect eyes during its course, none of the patients in our study had any ocular manifestations such as uveitis or keratitis. Tears play a vital role in ocular surface health and contain growth factors and vitamin A. The roles of growth factors and vitamin A in proliferation, differentiation, and maturation of the ocular surface epithelium have become well-understood during the past decade [3]. In previous studies, no significant difference had been observed regarding Schirmer 1 test values of patients with psoriasis, but the TBUT was found to be decreased [1,11]. The repeatability of different diagnostic tests for dry-eye evaluation has been studied, and the Schirmer test has been found to give variable results, low sensitivity and poor reproducibility compared to TBUT [12,13-15]. The irritative nature of the test, the positioning of the Schirmer paper, and the effects of evaporation and environmental factors (such as temperature and humidity) have been noted among the causes of poor sensitivity [15]. TBUT is reported to be more sensitive and repeatable and the most common test preferred for dry eye evaluation [12-15].
A shorter TBUT is the hallmark of mucin deficiency [10]. It is also involved in meibomian gland dysfunction. In their study, Zengin et al. [11] mentioned the obstructive type of meibomian gland dysfunction as the cause of an abnormal TBUT. Karabulut et al. [1] studied tear film changes and conjunctival impression cytology in patients with psoriasis and found a decreased break-up time, squamous metaplasia and goblet cells with poorly periodic acid-schiff positive-stained content. As impaired tear mucin can also cause a decrease in TBUT, we studied plasma vitamin A, a factor affecting the mucin-secreting goblet cells. In an animal study, Fujikawa et al. [2] showed that vitamin E prevented corneal and conjunctival changes due to vitamin A deficiency, so we studied vitamin E as well.
There is still some controversy regarding the pathogenic role of plasma vitamin A and vitamin E levels in patients with psoriasis [16,17]. In a study by Majewski et al. [6], plasma level of vitamin A was found to be decreased in psoriatic patients as compared with the values in an age- and gender-matched group. Safavi [7] observed no evidence of decreased plasma vitamin A level in patients with psoriasis, but found a decrease in plasma vitamin A level that was related to age and gender. Kokcam and Nazıroglu [8] did not find a significant difference in plasma vitamin E levels in patients with psoriasis, but plasma beta carotene level, a precursor of vitamin A, was decreased. Marrakchi et al. [9] reported decreased levels of vitamin A and vitamin E in the same group of patients with a history of alcohol consumption, especially in the active period of erythrodermic or pustular psoriasis. In that study, the blood levels of these two vitamins were not found to be reduced in the other study groups (i.e., patients with psoriasis vulgaris with or without a history of chronic or heavy alcohol consumption) [9].
The mean plasma levels of vitamin A and E levels in subjects with psoriasis were not different from the control subjects in our study. Our results are in agreement with the results of Safavi [7] and Marrakchi et al. [9]. We also did not find any correlation among plasma vitamin A and E levels, TBUT and the severity and duration of the disease. These results suggest that plasma vitamin A and E levels do not differ between patients with psoriasis and healthy controls. Abnormalities in cellular metabolism of vitamin A and regulation of retinol binding protein genes have been reported in psoriasis, and the disease has responded favorably to exogenous vitamin A derivatives [16-19]. The results of the current study show that the tear film changes in psoriasis are not related to a deficiency of vitamin A or E. We may speculate that psoriasis-related ocular surface and tear film changes may be due to impaired uptake or processing of these vitamins by the conjunctival epithelial cells, rather than the lack of circulating vitamins A and E. To the best of our knowledge, this is the first study correlating serum vitamin A and E levels with TBUT estimates.
Although the etiology of psoriasis is unknown, further controlled prospective studies with a larger number of participants and ultrastructural evaluation should be conducted to better understand the exact nature of the tear film and ocular surface changes and their relationship to vitamins A and E in patients with psoriasis.
Acknowledgements
The authors would like to thank İlker Etikan and Ünal Erkorkmaz PhD for their assistance with the statistical analysis and Fikret Özuğurlu PhD for his assistance with the biochemical analysis performed in this study.
Notes
No potential conflict of interest relevant to this article was reported.