Abducens Nerve Palsy Complicated by Inferior Petrosal Sinus Septic Thrombosis Due to Mastoiditis
Article information
Abstract
We present a very rare case of a 29-month-old boy with acute onset right abducens nerve palsy complicated by inferior petrosal sinus septic thrombosis due to mastoiditis without petrous apicitis. Four months after mastoidectomy, the patient fully recovered from an esotropia of 30 prism diopters and an abduction limitation (-4) in his right eye.
In many reports, abducens nerve palsy complicated by otitis media is accompanied by involvement of the abducens nerve pathway due to petrous apicitis [1]. In contrast, abducens nerve palsy complicated by septic thrombosis of the inferior petrosal sinus due to mastoiditis and otitis media without petrous apicitis is very rare. Here we report our findings in such a patient.
Case Report
A 29-month-old boy presented with acute onset of esodeviation and limitation of ocular movement in his right eye. Six weeks earlier, he had right otitis media, but no improvement was achieved. Five days before onset of esodeviation, he had a high fever (over 39℃), otorrhea, and cough. Otolaryngological examination showed that the right eardrum and tonsils were congestive. Laboratory evaluation revealed a white blood cell (WBC) of 30,127/uL and C-reactive protein (CRP) of 51.60 mg/L. A blood culture was positive for Streptococcus pneumoniae, suggesting a septic condition. On his second day in the hospital, the patient had a recurrent high fever due to mastoiditis complicated by otitis media. On his fourth day in the hospital, his fever was controlled but he complained of mastoid tenderness, otalgia, rhinorrhea, nasal stuffness, and postnasal drip, and his right eardrum was yellowish brown. Laboratory evaluation revealed a WBC of 15,000/uL, CRP of 19.68 mg/L, erythrocyte sedimentation rate of 115 mm/hr, and D-dimer of 739 ng/mL, suggesting a septic condition. On his fifth day in the hospital, he underwent myringotomy and insertion of a ventilation tube into the right ear. A serous discharge was drained from the myringotomy site. On the first day after surgery, an esotropia of 30 prism diopters (PD) and an abduction limitation (-4) occurred in his right eye, and facial turn to the right appeared (Fig. 1). Six days after surgery, he underwent magnetic resonance imaging (MRI) to assess other defects in intracranial or optic nerve pathways. The MRI showed right mastoiditis, and stasis of the transverse sinus and internal jugular vein. The thrombus, however, was not significant (Fig. 2). Temporal bone computed tomography showed erosive changes in the right mastoid adjacent to the sigmoid sinus, but petrous apicitis was not observed (Fig. 3). Seven days after surgery, the patient underwent a mastoidectomy. One week after mastoidectomy, he had mostly recovered from the septic condition caused by the mastoiditis, but the esotropia of 30 PD, the abduction limitation (-4) in the right eye, and the facial turn to the right were sustained. Three weeks after mastoidectomy, we observed improvements in the esotropia (25 PD), abduction limitation (-2) and alternate fixation. Four months after surgery, he had fully recovered from the esotropia, limitation of ocular movement, and anomalous head posture (Fig. 4).
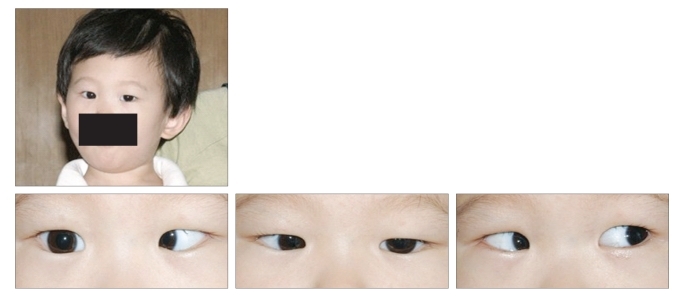
Photographs show an anomalous head posture of right-turning facial position, an abduction defect (-4), and an esodeviation of 30 prism diopters in his right eye. Informed consent was received from parents of the patient.
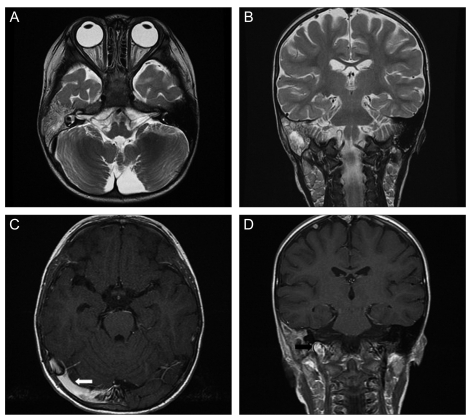
(A) Preoperative axial enhanced T2-weighted magnetic resonance (MR) image shows right otomastoiditis. (B) Preoperative coronal enhanced T2-weighted MR image shows right otomastoiditis. (C) Axial enhanced T1-weighted MR image shows slow flow velocity of the right transverse sinus (white arrow). (D) Coronal enhanced T1-weighted MR image shows slow-flow velocity of the right internal jugular vein (black arrow).
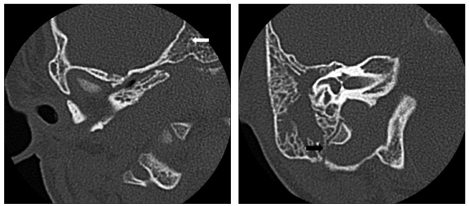
Computed tomography of the right temporal bone shows no inflammation of the petrous bone (white arrow) and an erosive mastoid septa (black arrow).
Discussion
Acute mastoiditis and intracranial complications resulting from otitis media were very common prior to the introduction of antibiotics [1,2]. Although the incidence of these complications dropped dramatically after antibiotics were developed, intracranial complications caused by mastoiditis remain serious complications, especially in infants, with an incidence of about 10% to 15% [3]. Abducens nerve palsy is a rare complication resulting from direct damage to abducens nerve pathways caused by Gradenigo's syndrome, petrous apicitis, cavernous sinus thrombosis or lateral sinus thrombosis [4,5].
The abducens nerve is the cranial nerve most frequently involved in acquired cranial ocular motor palsy. The causes of this condition can be microangiopathy, cerebral trauma, tumor, and inflammation, or it may be idiopathic. The causes of abducens nerve palsy are similar in children and adults, although vascular diseases and viral infections are less common in children, whereas trauma and neoplasia occur more frequently. Spontaneous recovery within 6 months is common, although the rate of recovery varies according to the cause [5-7].
Abducens nerve palsy complicated by otitis media without petrous apicitis is very rare. In our patient, the most likely cause of abducens nerve palsy was inflammatory invasion of the periosteum of the petrous apex from the middle ear caused by pachymeningitis, extradural abscess or thrombophlebitis from the lateral or inferior petrosal sinus [5,7]. The inferior petrosal sinus runs postero-inferiorly from the cavernous sinus in a groove between the petrous and basilar occipital bone. Shortly after leaving the cavernous sinus, the inferior petrosal sinus runs parallel to the sixth nerve as the nerve pierces the dura [3,6].
In our patient, abducens nerve palsy was accompanied by mastoiditis and sepsis complicated by otitis media, but there was no evidence of petrosal apicitis, cavernous thrombosis or thrombophlebitis from the lateral sinus responsible for ipsilateral abducens nerve palsy. Venous stasis of the lateral sinus and a case report of thrombosis caused by perisinus fibrin deposition and phlebitis of the lateral sinus reinforce the hypothesis that abducens nerve palsy is secondary to inferior petrosal sinus thrombosis [3]. This hypothesis is further reinforced by the absence of trigeminal nerve involvement [3,7]. Due to its small size, however, the inferior petrosal sinus is very difficult to visualize in radiologic diagnostic images [8]. Any disorder that causes an abduction deficit should be included in the differential diagnosis of patients with abducens nerve palsy. A syndrome involving constant otorrhea, headache, and diplopia, thought to be due to inflammation of the petrous apex, is called Gradenigo's syndrome. In the present patient, however, this syndrome was excluded on the basis of the absence of apicitis, retrobulbar pain, and trigeminal nerve palsy.
We describe here a 29-month-old infant with a very rare case of abducens nerve palsy complicated by septic thrombosis of the inferior petrosal sinus due to mastoiditis without petrous apicitis.
Notes
No potential conflict of interest relevant to this article was reported.
