Optic disc pit is a congenital optic disc anomaly first described by Wiethe in 1882, and it occurs in approximately one in 11,000 patients [1]. About 70% of the pits are on the temporal side of the disc, and about 20% are situated centrally; the remainder are found inferiorly, superiorly, and nasally [2]. The macular retinoschisis (or serous detachment) seen in association with optic disc pit maculopathy appears most commonly when the pit is located in the temporal region of the optic disc and in larger pits [2]. The prevalence of maculopathy caused by optic disc pit has been reported to vary between 25% and 75% [3,4].
There are many reports about cases of optic disc pit maculopathy, but to our knowledge, there have not been any reports about optic disc pits with peripapillary retinoschisis not extending to the macula and presenting as a localized retinal nerve fiber layer (RNFL) defect.
Case Report
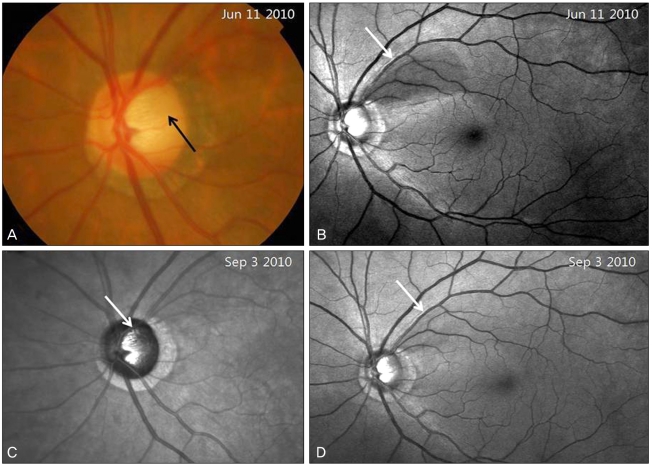
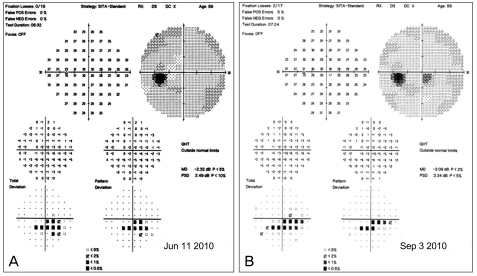
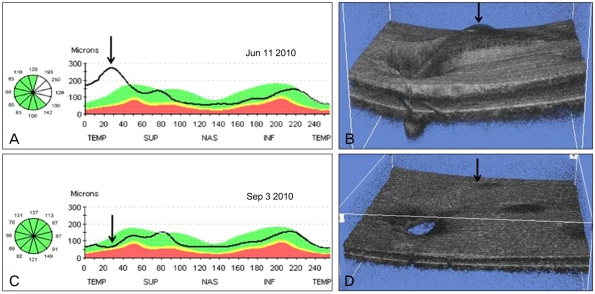
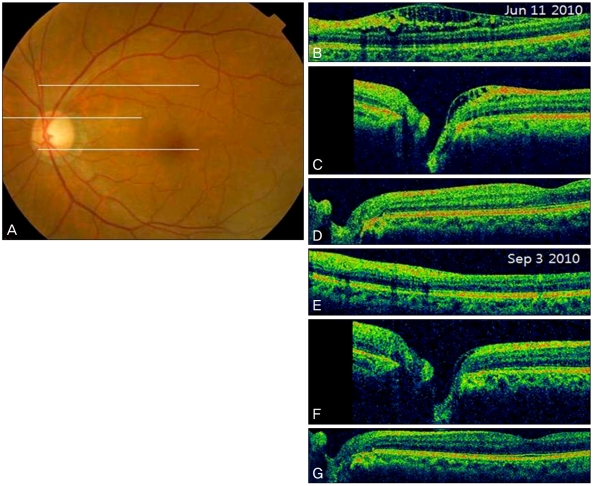
A 59-year-old woman was referred to our clinic for glaucoma evaluation. Her visual acuity was 20 / 20 and intraocular pressure was 14 mmHg in both eyes. Slit-lamp examination of the anterior segment showed no specific findings in either eye. Red-free fundsus photography and visual field testing with the central 30-2 Swedish Interactive Threshold Algorithms-Standard strategy of the Humphrey Visual Field Analyzer (HFA II, model 750; Carl Zeiss Meditec, Dublin, CA, USA) were normal in the right eye. However, in the left eye, an optic disc pit with a superotemporal wedge-shaped RNFL defect was found by disc photography and red-free fundus photography (Fig. 1A and 1B). Visual field testing revealed a corresponding inferior partial arcuate scotoma in two repeat examinations (Fig. 2A). However, optical coherence tomography (OCT) (Stratus OCT, Carl Zeiss Meditec) RNFL scan indicated RNFL thickening of the superotemporal region rather than RNFL thinning (Fig. 3A). This result did not correlate with that of red-free fundus photography. Spectral domain OCT (3D OCT-1000; Topcon Corp., Tokyo, Japan) peripapillary and macular cube scans were performed, resulting in the finding of superotemporal arcuate-shaped peripapillary retinoschisis (Figs. 3B and 4A-4D). The macula was flat and there was no retinoschisis in the papillomacular retinal region. The optic disc pit and the superotemporal peripapillary retinoschisis seemed to be connected to each other, indicating that the peripapillary retinoschisis probably resulted from the optic disc pit. A topical prostaglandin analogue was administered to the patient. After 3 months of medication, the intraocular pressure in the retinoschisis eye was lowered to 10 mmHg, and the peripapillary retinoschisis was partially resolved (Figs. 3C and 3D; 4E-4G). The RNFL defect seemed to decrease in red-free fundus photography (Fig. 1D), but the visual field testing showed no change (Fig. 2B).
Discussion
Optic disc pits are congenital excavations of the optic nerve head usually seen in association with other abnormalities of the optic nerve and peripapillary retina, including large optic nerve head size, large inferior coloboma of the optic disc, and retinal coloboma [5]. Histologically, optic disc pits are defects in the lamina cribrosa and have been reported to be associated with a variety of retinal abnormalities including aberrant nerve fibers and pigmented tissues, resemble retinal pigment epithelium, and are supported by a framework of glial tissue [1].
Visual acuity is usually unaffected unless the pit is complicated by subretinal fluid, but serous macular retinal detachment eventually complicates 25% to 75% of optic disc pits [6]. The pathophysiology of optic disc pit maculopathy remains unclear. Lincoff et al. suggested that the primary communication from the optic disc pit is to the retina temporal to the optic disc, in which fluid slips under the inner retina, lifting it and the nerve fiber layer up and away from the outer retina [7,8]. This has been corroborated by OCT and extended to show both retinal schisis and an outer retinal detachment connected by a hole in the outer retinal layer [3].
There are some reports about optic disc pits and their relationship to glaucoma. Radius et al. described incident pits of the optic disc in open-angle glaucoma, both clinically and histologically, demonstrating an association with glaucoma progression [9]. In addition, a number of authors have confirmed these findings in clinic-based case-control studies [10-12]. Also, Healey and Mitchell [13] reported that optic disc pits are associated with glaucoma and the related signs of optic disc hemorrhage and ╬▓-peripapillary atrophy.
In the present case, the initial examination seemed to be an RNFL defect whose base did not reach the horizontal fundus raphe and a corresponding visual field defect. However, an OCT scan and disc photography showed an optic disc pit with an arcuate-shaped peripapillary retinoschisis, not involving the macula. This is an unusual type of optic disc pit and is apt to be confused with a peripapillary retinoschisis with an RNFL defect. When an RNFL defect is found by red-free fundus photography, the possibility of optic disc pit with peripapillary retinoschisis should be considered. To our knowledge, this is a rare case of optic disc pit with peripapillary retinoschisis presenting as a localized RNFL defect, and the peripapillary retinoschisis was partially resolved after the administration of antiglaucoma medication.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






