 |
 |
| Korean J Ophthalmol > Volume 25(5); 2011 > Article |
Abstract
Purpose
To compare the outcomes of unilateral lateral rectus recession between the first operation and second operation for exotropia.
Methods
Thirty-two patients who underwent unilateral lateral rectus recession for exotropia of 15 to 20 prism diopters (PD) were investigated. The follow-up period was at least 6 months. We classified 17 patients without a surgical history for exotropia (first operation group) and 15 patients with a previous procedure (second operation group). Surgical success was defined as an exodeviation or esodeviation of less than 10 PD at the primary position. Postoperative deviation angles and success rates were compared between the two groups.
Results
There were no significant differences in the age, gender, visual acuity (logarithm of the minimal angle of resolution), preoperative deviation, and amount of recession between the two groups. Postoperative deviations were -1.7 ┬▒ 5.5:1.3 ┬▒ 5.1 PD at one day, 4.3 ┬▒ 3.8:5.6 ┬▒ 5.1 PD at 1 month, 4.3 ┬▒ 4.3:3.0 ┬▒ 8.1 PD at 3 months, and 5.0 ┬▒ 4.3:4.5 ┬▒ 7.2 PD at 6 months post-operation, and there was no statistically significant difference between the two study groups. Surgical success rate were 95.2:100% at one day, 95.2:92.9% at 1 month, 90.5:85.7% at 3 months, and 90.0:92.9% a 6 months post-operation.
Conclusions
In patients with exotropia of 15 to 20 PD, no significant difference was found in terms of the postoperative deviation angle and the surgical success rate between the first operation and the second operation groups. Unilateral lateral rectus recession can lead to similar results in 15 to 20 PD exotropia for the first operation or recurrent exotropia.
The classical operation methods for basic type exotropia are bilateral lateral rectus recession or unilateral recession of the lateral rectus and resection of the medial rectus (R & R) [1]. The use of unilateral lateral rectus recession (ULR) for small- to moderate-angle exotropia has become increasingly popular, although the surgical results have yielded varied outcomes [2-12].
Operating on one muscle instead of two muscles has the advantages of shortening the anesthesia and operating time, diminishing the risk associated with muscle surgery, such as scleral perforation, retinal detachment, or endophthalmitis, and performing a second operation more easily if exotropia recurs [2]. In addition, it also has the advantage of reducing amblyopia associated with overcorrection and deterioration of stereopsis due to amblyopia [3]. However, undercorrection can appear after long-term follow-up [3], and it has been reported that a limitation of abduction could develop due to a large amount of recession in one muscle [4].
Deutsch et al. [5] performed ULR surgeries in 30 patients with moderate-angle exotropia. All 30 patients had orthophoria or deviations of 10 prism diopters (PD) or less after 21 months follow-up. In contrast to this study, Kim and Chang [6] reported a poor prognosis for ULR patients in cases of recurrent exotropia. Among 40 patients with recurrent exotropia who underwent ULR, the rate of success, defined as stability in 10 PD, was 55.6% at 12 to 14 months post-operation. We speculate that the reason for the difference of these results may lie in their demographic characteristics, including the surgical history for exotropia. The surgical success rate of reoperation for exotropia was different from that of the first operation for exotropia due to a lesser change in postoperative divergence at reoperation than with the first operation [13]. However, a comparison of surgical results after ULR between the first operation and the second operation for exotropia has not yet been evaluated. So, we decided to perform this study and compare the surgical results of ULR between the first operation group for exotropia and the second operation group for recurring exotropia.
We retrospectively reviewed the medical records of patients who underwent ULR for basic type exotropia and recurred exotropia of 15 to 20 PD between March 2003 and January 2009. All patients had a minimum of 6 months of follow-up after surgery. The exclusion criteria were as follows: 1) amblyopia at surgery, 2) type A or type V exotropia, 3) paralytic strabismus, 4) concurrent oblique or horizontal muscle surgery, 5) abnormal version and duction preoperatively, and 6) presence of systemic abnormalities such as Down syndrome or cerebral palsy.
Fifteen patients that underwent ULR for recurred exotropia (15 to 20 PD) were included in second operation group. The mean age at the time of the second surgery was 10.2 ┬▒ 2.6 years (range, 5.5 to 16.0 years), and the average duration of postoperative follow-up was 22.9 ┬▒ 15.0 months (range, 7 to 53 months). Seventeen patients who underwent ULR for exotropia (15 to 20 PD) between 2005 and 2007 were assigned to first operation group based on consideration of preoperative bias (age of patients and duration of postoperative follow-up) for operative results. The mean age at the time of surgery was 9.2 ┬▒ 1.2 years (range, 8.1 to 12.4 years), and the duration of postoperative follow-up was 19.3 ┬▒ 7.8 months (range, 7 to 39 months).
The following parameters were reviewed and analyzed: gender, age at each operation, methods of first and second operations, preoperative best corrected visual acuity (BCVA), and history of amblyopia treatment. All examinations were performed under BCVA. The deviation angles were measured in the primary position at distance and near fixation, and the secondary position at distance fixation using an alternate prism cover test. Stereopsis was measured using the Titmus stereo test (Stereo Optical Cl Inc., Chicago, IL, USA) at both preoperative and final follow-up examinations. All surgeries were performed by one surgeon. The surgery was performed on the basis of the largest angle of deviation during follow-up, according to the Wright table [14], and the operation was performed on the virgin muscle in both groups. The amount of recession was 7 to 9 mm according to their deviation angle.
Surgical success was defined as having a deviation angle less than 10 PD at each follow-up examination after the operation. We defined a recurrence as a 10 PD or more exotropia. The deviated angle and the success rate of surgery were compared at one day, one week, 1 month, 3 months, and 6 months post-operation, and at a final follow-up visit after surgery.
Statistical analysis was carried out using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA), and a p-value of less than 0.05 was considered statistically significant.
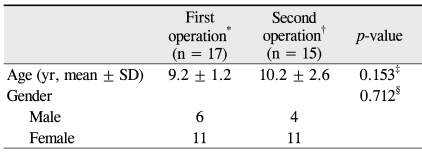
The mean age was 9.2 ┬▒ 1.2 years (range, 8.1 to 12.4 years) at the time of surgery in first operation group and 10.2 ┬▒ 2.6 years (range, 5.5 to 16 years) at the time of the second surgery in second operation group, and there was no significant difference between the two groups (Mann-Whitney U-test, p = 0.153). There was also no difference in gender between the two groups (Fisher's exact test, p = 0.712) (Table 1). The mean age at the time of the first surgery was 5.8 ┬▒ 1.7 years (range, 4.0 to 8.4 years) in the 15 patients of second operation group. In the first surgery of the patients in second operation group, 7 patients (46.7%) underwent ULR, while the remaining patients (53.5%) underwent R & R. The second surgery was performed at 53.8 ┬▒ 31.5 months (range, 18 to 111 months) after the first surgery.
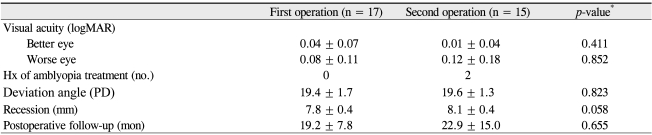
There was no difference in the preoperative visual acuity of the better and worse eyes between the two groups (Mann-Whitney U-test, p = 0.411, p = 0.852), and the preoperative deviation was 19.4 ┬▒ 1.7 PD in first operation group and 19.6 ┬▒ 1.3 PD in second operation group (Mann-Whitney U-test, p = 0.823). The average amount of ULR recession was 7.8 ┬▒ 0.4 mm in first operation group and 8.1 ┬▒ 0.4 mm in second operation group, and there was no significant difference between the two groups (Mann-Whitney U-test, p = 0.058). The average duration of follow-up after surgery was 19.3 ┬▒ 7.8 months (range, 7 to 39 months) in first operation group and 22.9 ┬▒ 14.8 months (range, 7 to 53 months) in second operation group. The duration was 3 months longer in second operation group, although there was no statistically significant difference (Mann-Whitney U-test, p = 0.852) (Table 2).
The mean deviation angles were -2.1 ┬▒ 5.7 PD and 1.6 ┬▒ 5.1 PD in first and second operation groups, respectively, at one day post-operation, and there was no statistical difference between the two groups (Mann-Whitney U-test, p = 0.076). The mean deviation angles for first and second operation groups were 2.4 ┬▒ 3.6 PD and 3.6 ┬▒ 5.4 PD at one week (p = 0.295), 4.4 ┬▒ 3.7 PD and 5.7 ┬▒ 4.9 PD at 1 month (p = 0.455), 4.4 ┬▒ 4.4 PD and 3.5 ┬▒ 8.0 PD at 3 months (p = 0.941), and 5.1 ┬▒ 4.6 PD and 4.9 ┬▒ 7.1 PD at 6 months post-operation (p = 0.852), and 8.6 ┬▒ 4.7 PD and 8.2 ┬▒ 8.9 PD at the final follow-up visit (p = 0.970), respectively. During follow-up, there was no difference in the deviation angles between the two groups, and exodrift had developed in both groups (Fig. 1).
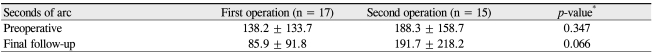
The success rates of surgery were 94.1% in first operation group and 100% in second operation group at one day (Fisher's exact test, p = 1.000), 100% for both groups at one week, 94.1% and 92.9% (p = 1.000) at 1 month, 88.2% and 85.7% at 3 months (p = 1.000), and 88.2% and 92.9% at 6 months post-operation (p = 1.000), respectively. There was no difference in the success rate between the two groups during follow-up. At the final follow-up visit, the success rate decreased to 64.7% and 60.0% (p = 1.000), respectively, for first and second operation groups, because of exodrift (Fig. 2). There was no difference in stereopsis between the two groups at the preoperative and final follow-up examinations (Mann-Whitney U-test, p = 0.347, p = 0.066) (Table 3).
At the final follow-up visit, one patient in second operation group needed Fresnel prism glasses due to diplopia from 10 PD esotropia from 4 months to 13 months after surgery. Exotropia was reccurred in one patient of first operation group at one year post-operation, and in 6 patients of second operation group at 19.5 ┬▒ 13.8 months post-operation (range, 1 to 42 months). In these cases among second operation group patients, the methods used in the first surgery were ULR in 3 patients and R & R in the other 3 patients.
In this study, the surgical results of ULR were compared between exotropia patients without a surgical history and patients who had previously undergone surgery for exotropia. Our data showed that the success rate between the two groups was similar, and the success rate decreased during follow-up in both groups.
ULR has been performed as a method of surgery for small-to moderate-angle intermittent or constant exotropia, and the surgical results of ULR were reported variously according to the author [2-12]. In study of Reynolds and Hiles [7], 36 patients with deviation angles of 10 to 20 PD received ULR of 4 to 6.5 mm. Of the 18 patients who were followed postoperatively for 9 months or longer, 88% of them had orthophoria or small-angle exophoria. Therefore, they advocated ULR as an effective treatment for exotropia of 10 to 20 PD. Sul and Park [10] described ULR of 8 to 9 mm as being an effective treatment in cases of moderate-angle exotropia (18 to 35 PD). After 14 weeks follow-up, the success rate was 90%. However, some authors reported that ULR was ineffective or yielded inconsistent results [8,9]. Lee and O'Brien [8] described inconsistent results of ULR in 15 patients with varying degrees of exotropia. Dunlap and Gaffiney [9] also reported that ULR as a treatment was inadequate, except in cases of small-angle exotropia (10 to 15 PD). In the study of Lee et al. [11], 30 patients with exotropia of 23 to 28 PD were underwent ULR of 9.0 mm. After 6 months of follow-up, 76.7% of patients had an alignment within 8 PD and there were no limitations of abduction and overcorrection. Lee et al. [12] conducted a retrospective study of 62 patients with intermittent exotropia of less than 25 PD. They underwent ULR and had a minimum of 6 months follow-up. At the one one-year follow-up examination, the success rate, defined as having an alignment within 10 PD, was 85.7%. The varying results of the previously mentioned studies were caused by several factors. We speculate that the reasons for the variation in ULR outcomes may include the patient's age, different deviation angles, amount of recession, the history of strabismus surgery, and postoperative follow-up periods in each study. Therefore, our study focused specifically on the homogenous baseline characteristics of the subjects. There was no statistical significance for the age at surgery, preoperative angle of deviation, or postoperative follow-up duration between the two groups. Furthermore, any patients with a history of strabismus operation were excluded in several studies [2-5,10-12,15]. Kim and Chang [6] reported on the results of ULR in recurrent exotropia after R & R. They included the patients with a variable amount of deviation (15 to 30 PD) and the amount of ULR was 6 to 8 mm. Beyond this study, there was no other study of using ULR for a second operation for exotropia. We compared the surgical results between the first and second surgery groups in this study. To the best of our knowledge, there was no study directly comparing the results of ULR in exotropia and in recurred exotropia.
However, the success rate in cases of recurred exotropia (second operation group) was better than that in Kim and Chang's study [6]. We speculate that these differences in the surgical results may be due to different angles of preoperative deviation. In the study of Kim and Chang [6], the range of exodeviation was 15 to 30 PD. However, in our study, only exotropia patients with 15 to 20 PD were included.
In this study, 15 (88.2%) of the 17 patients in first operation group and 14 (92.9%) of the 15 patients of second operation group showed alignment within 10 PD at 6 months post-operation, and 11 (64.7%) of the 17 patients in first operation group and 9 (60.0%) of the 15 patients in second operation group showed alignment within 10 PD at their final follow-up examination. The success rates showed no significant difference between the two groups, and these results were consistent with those of the earlier studies of ULR for exotropia [7,10-12]. Therefore, these results suggest that the prognosis of ULR in recurred exotropia may be similar with those in exotropia without a previous surgical history, and ULR may have the merits of limiting surgery to only one muscle in recurred exotropia.
In conclusion, ULR had a similar effect in the correction of exotropia of 15 to 20 PD between the first surgery group and the second surgery group during the follow-up period of 19 to 22 months. Therefore, we propose that ULR may achieve the same or similar results in both first and second surgical procedures for exotropia ranging from 15 to 20 PD.
Acknowledgements
This work was supported by the clinical research grant of the Chungbuk National University Hospital in 2011.
Notes
This article was presented at the Korean Ophthalmological Society 102nd annual meeting on November, 2009 in Goyang, Korea.
REFERENCES
2. Nelson LB, Bacal DA, Burke MJ. An alternative approach to the surgical management of exotropia: the unilateral lateral rectus recession. J Pediatr Ophthalmol Strabismus 1992;29:357-360.


3. Weakley DR Jr, Stager DR. Unilateral lateral rectus recessions in exotropia. Ophthalmic Surg 1993;24:458-460.


4. Lee SY. The effect of unilateral lateral rectus muscle recession over 11mm in the treatment of intermittent exotropia of 15-20PD. J Korean Ophthalmol Soc 1999;40:550-554.
5. Deutsch JA, Nelson LB, Sheppard RW, Burke MJ. Unilateral lateral rectus recession for the treatment of exotropia. Ann Ophthalmol 1992;24:111-113.

6. Kim JY, Chang BL. The effect of unilateral lateral rectus recession in recurrent exotropia. J Korean Ophthalmol Soc 1995;36:2261-2265.
7. Reynolds JD, Hiles DA. In: Reinecke RD, Single lateral rectus muscle recession for small angle exotropia. Strabismus 2. 1984. New York: Grune & Stratton; p. 247-253.
8. Lee OS, O'Brien CS. In: Allen JH, Surgical treatment of concomitant divergent strabismus. Strabismus ophthalmic symposium. 1950. St Louis: Mosby.

9. Dunlap EA, Gaffiney RB. Surgical treatment of intermittent exotropia. Am Orthopt J 1963;19:20-33.
10. Sul CY, Park C. Large recession of one lateral rectus muscle for moderate-angle exotropia. J Korean Ophthalmol Soc 1988;29:125-129.
11. Lee SH, Kim JY, Kwon JY. The effect of unilateral lateral rectus recession for the treatment of moderate-angle exotropia. J Korean Ophthalmol Soc 2005;46:2045-2049.
12. Lee SN, Shin DB, Xu YG, Min BM. Effect of unilateral lateral rectus recession for intermittent exotropia under 25 PD. J Korean Ophthalmol Soc 2002;43:1469-1473.
13. Sohn JH, Chang BL. Management for reoperation in recurrent exotropia. J Korean Ophthalmol Soc 1994;35:580-584.
14. Wright KW. Practical aspects of the adjustable suture technique for strabismus surgery. Int Ophthalmol Clin 1989;29:10-15.


15. Attarzadeh H, Zandi A, Nasrollahi K, Mortazavi AA. Two year results of unilateral lateral rectus recession on moderate intermittent exotropia. J Res Med Sci 2008;13:12-16.
Fig.┬Ā1
Comparison of deviation angle at each follow-up examination after surgery. PD = prism diopters. *Mann-Whitney U-test; ŌĆĀExotropia without previous surgery; ŌĆĪRecurred exotropia.
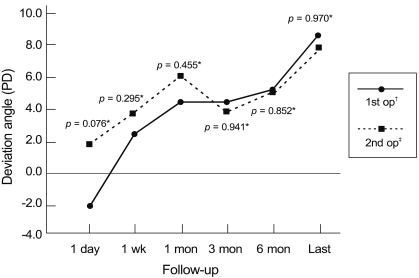
Fig.┬Ā2
Surgical success rate at each follow-up examination after surgery. *Fisher's exact; ŌĆĀExotropia without previous surgery; ŌĆĪRecurred exotropia.

- TOOLS
-
METRICS

- Related articles
-
Comparison of Retinal Nerve Fiber Layer Thickness between Stratus and Spectralis OCT2011 June;25(3)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



