Intravitreal Bevacizumab (Avastin) as an Adjuvant for the Treatment of Posterior Scleritis
Article information
Abstract
We report a case of posterior scleritis effectively managed with intravitreal bevacizumab. A 71-year-old woman was diagnosed with posterior scleritis. Although she was initially treated with systemic steroids, her clinical presentation deteriorated. She was then treated with a single intravitreal injection of bevacizumab and aqueous humor collection. The aqueous level of vascular endothelial growth factor prior to the intravitreal injection was 880.51 pg/mL, greater than that in the healthy control group (p < 0.001). One month later, the scleritis was completely resolved, and the patient remained stable during six months of follow-up. Intravitreal bevacizumab appears to be an effective adjuvant therapy for patients with posterior scleritis.
Posterior scleritis is an uncommon and under-recognized form of scleral inflammation [1]. The majority of patients with idiopathic posterior scleritis respond well to treatment with non-steroidal anti-inflammatory drugs. Here, we report a patient with posterior scleritis who had a favorable response to intravitreal bevacizumab. This patient had elevated levels of vascular endothelial growth factor (VEGF) and interlukin (IL)-8 in the aqueous humor; serum levels of these molecules were not increased.
Case Report
A 71-year-old woman presented to our clinic for evaluation of right ocular pain and loss of visual acuity for the previous week. On ophthalmic examination, visual acuity was 20 / 50 in the right eye (OD). There was an anterior chamber reaction (++) and a vitreous cell reaction (+) in the OD. Fundus examination revealed disc swelling, peripheral serous retinal detachment, and edema at the site of a macular lesion (Fig. 1A). Fluorescein angiography revealed disc edema and vascular leakage (Fig. 1B). Posterior scleral thickening, choroidal effusion, and serous retinal detachment were demonstrated on ocular ultrasonography, suggesting posterior scleritis (Fig. 1C). Other laboratory findings were normal and she had no systemic disease. The patient was treated with prednisolone (1 mg/kg orally) and topical prednisolone (1%). After three days of treatment, the serous and choroidal detachment worsened, and her visual acuity decreased to hand movement. The patient agreed to proceed with intravitreal bevacizumab treatment (1.25 mg/0.1 mL) after informed consent for the off-label use of this drug was obtained.
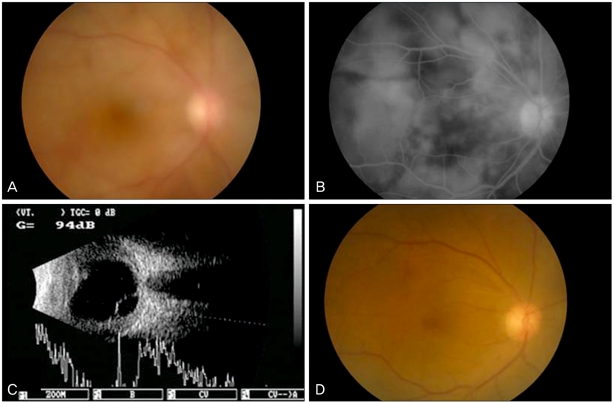
(A) Fundus photography at initial presentation demonstrates serous detachment and vitreous haziness in the right eye. (B) Mid-phase fundus fluorescein angiography demonstrates disc and vascular leakage involving the macula. (C) B-mode ultrasound scan demonstrating diffuse thickening of the posterior coatings of the eye (1.9 mm) together with fluid in the Tenon capsule and the nerve sheath. (D) Fundus photography one month post-intravitreal bevacizumab injection, demonstrating resolved posterior scleritis.
The patient was given a single intravitreal bevacizumab injection. Aqueous humor and blood samples were obtained prior to injection. One day later, the ocular pain and serous macular detachment were considerably reduced; after one month, the scleritis had completely remitted (Fig. 1D). The dose of oral prednisolone was gradually reduced over the course of one month. Further improvement was noted, and the patient remained stable during six months of follow-up with a visual acuity of 20 / 40 in the OD.
Concentrations of VEGF and IL-8 were measured using suspension bead array technology on a Luminex TM 100 IS system (Luminex Corp., Austin, TX, USA). Aqueous humor and blood samples from ten healthy controls undergoing cataract surgery were processed using an identical method. The aqueous humor and serum levels of VEGF and IL-8 from the patient were 880.51 pg/mL and 4,531.5 pg/mL, respectively, which were significantly higher than those of the healthy control group (65.1 ± 42.9 pg/mL and 132.4 ± 62.6 pg/mL, respectively; p < 0.001). The plasma levels of VEGF and IL-8 from the patient were 105.51 pg/mL and 5.91 pg/mL, respectively, which did not significantly differ from those of the healthy control group (255.7 ± 198.9 pg/mL and 17.8 ± 14.6 pg/mL; p = 0.416 and p = 0.328, respectively).
Data were compared using Student's t-test with Bonferroni's correction using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Discussion
Posterior scleritis is a common form of scleritis that should be suspected in patients who present with periocular pain, visual loss, or any of the other signs of posterior scleritis. The pathophysiology of posterior scleritis is not fully understood; however, during scleral inflammation multiple factors, including VEGF, may increase vascular permeability by altering gap formation between endothelial cells [2].
Bevacizumab is a full-length humanized recombinant antibody against VEGF. There have been numerous reports regarding its safety and efficacy in the off-label treatment of choroidal neovascularization and other ischemic-proliferative retinopathies [3]. However, no studies using intravitreal bevacizumab as an adjuvant in treating posterior scleritis have been published to date. VEGF, a powerful angiogenic substance, significantly increases vascular permeability and is associated with inflammation and immune-mediated pathology. Therefore, we hypothesized that VEGF is elevated in posterior scleritis. To test this hypothesis, we measured the aqueous humor and plasma levels of VEGF in an affected patient. IL-8, a chemokine, not only promotes angiogenesis but also displays proinflammatory activity. High levels of IL-8 have been detected in patients with uveitis [4,5].
The current case describes the benefits of using intravitreal anti-VEGF therapy in combination with systemic treatment. We observed an increased level of VEGF in the aqueous humor of an affected patient without a corresponding increase is serum level. We suggest that the increased VEGF was locally expressed and was not associated with increased systemic production. The increased levels of VEGF and IL-8 in the aqueous humor provide a rationale for the use of intravitreal anti-VEGF therapy.
Although systemic steroid therapy may have a role in disease treatment, we demonstrated that an intravitreal bevacizumab injection could bring on prompt resorption of subretinal fluid, which may be associated with rapidly improved vision. The elevated aqueous humor levels of VEGF suggest that it plays an important role in intra-ocular inflammation and increased vascular permeability in posterior scleritis. Local anti-VEGF treatment may be an effective treatment option for posterior scleritis.
Notes
No potential conflict of interest relevant to this article was reported.