 |
 |
| Korean J Ophthalmol > Volume 24(2); 2010 > Article |
Abstract
Purpose
The purpose of this study was to compare and differentiate the clinical characteristics of intermittent exotropia (X(T)) in children and adults.
Methods
This study included 398 patients with X(T): 360 children ranging in age from 1 to 14 years and 38 adults over 15 years of age. Patients with neurological abnormalities or developmental delays were excluded. Clinical characteristics of interest included sex, age on first visit, age of onset, type of onset, duration to surgery, family history, chief complaints, type of fixation, refractive errors, sensory tests, angle of deviation, fundus examination, oblique muscle dysfunction, and other associated ocular disorders.
Results
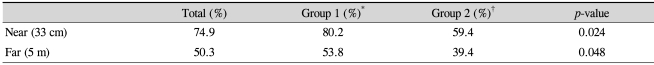
In both groups, an insidious onset was more common than a sudden onset (p=0.033). Outward deviation was the most common chief complaint in both groups, followed by photophobia in the childhood group, and diplopia in the adult group. The most common subtype of X(T) was the basic type. The mean near deviation was 23.6±7.9 prism diopters (PD) in the childhood group and 30.7±12.2 PD in the adult group (p=0.01). The mean distance deviation was 23.4±6.1 PD and 28.3±11.2 PD in the childhood and adult groups, respectively (p=0.028). The rate of fusion, measured with the Worth 4-dot test at near and distance was higher in the childhood group, as compared to the adult group (p=0.024 and p=0.048, respectively).
It has been reported that intermittent exotropia (X(T)) occurs more prevalently in Asian than in Caucasian populations. In Korea, it is one of the most common types of strabismus [1]. Intermittent exotropia manifests various clinical symptoms and mostly occurs at 2 to 4 years of age. It is known that, as children grow, the incidence of exodeviation increases or is maintained [2,3]. With regard to the changes in the angle of deviation associated with exotropia, Burian and Spivey [4] reported that exuberant convergence in childhood can mask an exotropia and that convergence weakens with age, producing an increasingly divergent position of the eye. In children, X(T) is usually identified by their parents chiefly because one eye appears turned out or because these children have a habit of closing one eye in bright sunlight. However, in adult patients, most visit the hospital because of discomfort associated with studies and work or cosmetic concerns [5]. In addition, the symptoms of X(T) vary, including headache, blurred vision, diplopia, and eye fatigue. To date, few articles have been published that compare the clinical characteristics of adult and pediatric X(T) cases [5].
The purpose of this study was, therefore, to compare and differentiate these characteristics among children and adults.
A retrospective study was conducted using the medical records of patients that visited the department of ophthalmology's outpatient clinic during the period ranging from January 2004 to December 2007. The study included 360 pediatric patients (group1) ranging in age from 1 to 14 years and 38 adults (group 2) over 15 years of age, all of whom were diagnosed with X(T) and in need of surgical treatment. Cycloplegic refraction was performed at least 30 minutes after the patient received one drop in each eye of 1% cyclopentolate and 0.5% tropicamide 3 times at 5-minute intervals. The presence of amblyopia was defined as a difference of two or more lines in the Snellen visual acuity charts between the best corrected visual acuity of each eye, or as a best corrected visual acuity lower than 20/30.
Anisometropia was classified as hyperopic anisometropia (>1 diopters [D]), myopic anisometropia (>2 D) and astigmatic anisometropia (>1.5 D). Employing the alternative prism cover test, measurements of the angle of deviation were obtained in all patients at distant (5 m) and near (33 cm) primary positions with fixation on accommodative targets.
Basic type was defined as when distance deviation was approximately equal to near deviation (within 10 prism diopters, PD). Divergence excess was defined as when exodeviation at distance fixation was greater than at near fixation by at least 10 PD. Convergence insufficiency was defined as when near deviation was at least 10 PD greater than distance deviation. Pseudodivergence excess was defined as when exodeviation at distance fixation is significantly larger than at near fixation, although an occlusion test is required to reveal the deviation at near fixation, which then often equaled or even exceeded that at distance fixation.
Sensory function was evaluated using the Titmus and the Worth 4-dot test (W4D). On the W4D (Flashlight type; Mag instrument, Ontario, CA, USA), the degree of fusion was measured at near and distance. For the stereoacuity test, we used a circle of Titmus (Stereo Optical Co. Inc., Chicago, IL, USA), and patients were recommended to wear Polaroid glasses at a distance of 40 cm. The disparity of circle of Titmus was 800, 400, 200, 140, 100, 80, 60, 50, and 40 seconds of arc (seconds). The distance stereoacuity was measured at a distance of 5 meters using a Mentor B-VAT II-SG videoacuity tester (Mentor O&O Inc., Norwell, MA, USA). Distance stereoacuity was evaluated using a B-VAT II BVS contour circle (BVC). The disparity of BVC consisted of 240, 180, 120, 60, 30 and 15 seconds. A fundus examination was performed following pupil dilation, for which the head was rightly fixated using a fundus camera (Visupac, Zeiss, Germany). Patients were instructed to view a camera indicator with the contralateral eye.
Statistical analysis was performed using Windows SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA), for which a Chi-square test and T-test were employed. A p-value less than 0.05 was regarded as statistically significant.
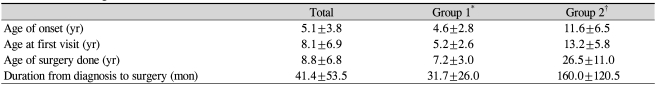
The mean age for surgery was 8.8±6.8 years. Two hundred and six males (51.8%) and 192 females (48.2%) patients were evaluated. The number of males was 188 (52.2%) in the childhood group and 20 (52.6%) in the adult group (p=0.673). The mean age at onset of exodeviation, mean age at which patients first visited the hospital, and mean duration from diagnosis to surgery are shown in Table 1. Thirty-seven (9.3%) of the patients had a family history of strabismus. Thirty-two patients (8.9%) in the childhood group and five (13.2%) in the adult group had a family history of strabismus.
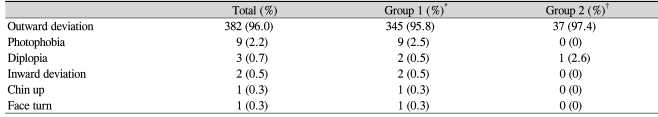
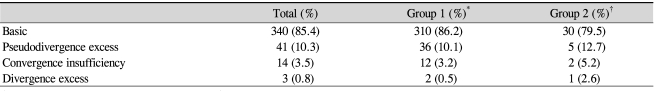
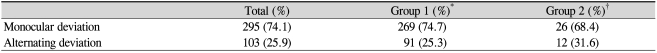
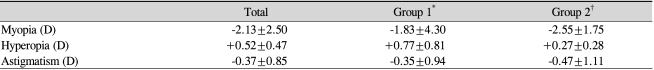
In regard to the pattern of onset, gradual onset was seen in 99.7% of the childhood group and 97.4% of the adult group. These proportions were significantly higher than those for sudden onset (p=0.033). The objective and subjective symptoms in both groups are shown in Table 2. In regard to the incidence based on the subtype of X(T), basic was the most prevalent type of X(T), followed by pseudodivergence excess, convergence insufficiency, and divergence excess (Table 3). In regard to type of fixation, there were 269 cases (74.7%) of monocular deviation and 91 cases (25.3%) of alternating deviation in the childhood group. In the adult group, there were 26 cases (68.4%) of monocular deviation and 12 cases (31.6%) of alternating deviation (p=0.166) (Table 4). Mean refractive errors are shown in Table 5.
The angle of deviation is shown in Table 6. Near and distance angles of exodeviation and distance hyperdeviation were all significantly greater in the adult group than in the childhood group (p=0.01, p=0.028, p=0.02) (Table 6).
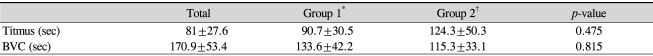
Table 7 shows the rate of fusion using W4D at near and distance. This was significantly higher in the childhood group than in the adult group (p=0.024, p=0.048). There was no significant difference in stereoacuity at near and distance between the children and adult groups (p=0.475, p=0.815) (Table 8).
In both groups, inferior oblique overaction (IOOA) was the most common type of associated ocular muscle dysfunction. IOOA was manifested by elevation on adduction, the rate of cases in which IOOA was greater than or equal to 1 was 36.9% (n=133) in the childhood group and 34.2% (n=13) in the adult group (p=0.104). Excyclotorsion with IOOA was 0.3% (n=1) in the childhood group and 0% in the adult group (p>0.05).
The most prevalent associated ocular abnormalities were astigmatism (41.0%) in the childhood group and myopia (46.8%) in the adult group. Among associated ocular abnormalities, causes of amblyopia in X(T) for both groups are shown in Table 9.
Intermittent exotropia shows variable clinical symptoms and is the most common type of strabismus in Korea [1]. It is known that most cases of X(T) originate from exophoria, then deteriorate into X(T) and constant exotropia as suppression deteriorates with age. It is therefore termed as a progressive disease [6].
The incidence of X(T) among patients shows a female predilection [7-9]. In this study, however, there was no significant difference in the incidence of X(T) between male and female patients. According to the Korean literature, Cho et al. [10] reported that the age of onset is 5 years of age or younger in 54.9% of total patients; Kwak et al. [11] reported 6 years of age or younger in 57.3% of total patients. These reports are similar to our results.
With regard to the prevalence of each X(T) subtype, Hardesty el al. [12] reported that, among patients with X(T) between 10 months and 51 years of age, 41% had basic, 48% had divergence excess, and 11% had convergence insufficiency. Burian and Spivey [4] reported that 65% of patients had basic type, 21.5% had divergence excess, and 13.5% had convergence insufficiency. Similarly, in this study, basic type was the most prevalent in both groups, followed by pseudodivergence excess, convergence insufficiency, and divergence excess. There was no significant difference between child and adult patients as compared with the previous studies.
In this study, among various chief complaints, outward deviation of the eye was observed to occur most prevalently in both groups. In the childhood group, photophobia was the second most prevalent symptom (2.7%). In the adult patient group, diplopia was the second most prevalent symptom (3%). Schlossman et al. [13] reported that diplopia was the most frequent symptom (26.5%) in adult patients with X(T). These authors also noted that diplopia frequently did not occur in childhood due to well-developed suppression mechanisms. In studying the cause of photophobia in children, Wirtschafter and von Noorden [14] reported that bright light adversely affects the amplitude of fusional convergence in patients who maintain a delicate balance between exophoria and X(T). Manley [15] reported that when a child is outdoors and looking at infinity, there are no near clues to stimulate convergence and that bright sunlight dazzles the retinas so that fusion is somehow disrupted, causing the deviation to manifest.
In regard to the changes in angle of deviation seen in patients with exotropia, Knapp [2] reported that fundamental exodeviation is present at birth, and the observed deviation increases as dynamic factors, such as accommodative convergence, change. Jampolsky [16] and von Noorden [7] reported that exophoria and X(T) have a common basis and usually arise in infancy, but that the latter may progress throughout life, both in degree and frequency of deviation. In this study, near and distance angles of deviation were significantly greater in the adult group than in the childhood group. These results indicate that as convergence weakens with age, the angle of deviation and symptoms, such as diplopia, increase.
Regarding sensory status in patients with X(T), Knapp [2] reported that the fusion mechanism is stressed most in the late teens and twenties, when the amount of close work increases, and in the forties, when accommodation is no longer adequate for close work. Also in this current study, a W4D showed that the rate of fusion was higher in the childhood group at both near and distance. These results may indicate that the accommodative or tonic convergence of children was more active than that of adults.
With respect to abnormalities of ocular muscle function in X(T), Wilson and Parks [17] conducted a 5-year-follow-up study in 148 patients with X(T). These authors reported that IOOA and dissociated vertical deviation could be observed at an incidence of 32% and 3%, respectively. They reported that the incidence of IOOA was not related to age of onset of strabismus, time from onset of strabismus to surgery, age at first surgery, or decompensation of ocular alignment.
When concurrent amblyopia is present in cases of X(T), Moore et al. [8] reported that anisometropic amblyopia, rather than strabismus amblyopia, accounted for the majority of cases of amblyopia. These authors also noted that only a small number of patients with X(T) had concurrent amblyopia. Similarly, in the current study, all three cases of amblyopia in the pediatric group were anisometropic amblyopia. Of two adult patients with amblyopia, one had anisometropic amblyopia and the other had strabismic amblyopia.
A limitation of the current study is that the number of adult patients with X(T) was smaller than that of pediatric patients. Nevertheless, no problems were encountered with the analyses of the statistical differences between the two groups. Moreover, in a comparison of stereopsis between the two groups, there was no significant difference between the pediatric and adult patient groups. These results point toward a lower compliance rate in the pediatric patient group, as compared to that of the adult patient group, which deserves further study.
In summary, there are various clinical characteristics in adult and childhood patients with X(T). Subjective symptoms, angle of deviation, and sensory tests were different between the two groups. Therefore, these are important factors to consider when assessing adults and children with X(T).
Notes
This article was presented in part at the 100th Autumn Meeting of Korean Ophthalmological Society, October 2008, Goyang, Korea
REFERENCES
1. Rah SH, Jun HS, Kim SH. An epidemiologic survey of strabismus among school-children in Korea. J Korean Ophthalmol Soc 1997;38:2195-2199.
3. In: Wright KW, Spiegel PH, Pediatric ophthalmology and strabismus. 2003. 2nd ed. New York: Springer; p. 224-228.
5. Lee SY, Oh JS, Kim SJ. The clinical characteristics and surgical results in the intermittent exotropia more than 15 years of age. J Korean Ophthalmol Soc 1997;38:1056-1063.
7. Von Noorden GK, Campos EC. Binocular vision and ocular motility. 2002. 6th ed. St. Louis: Mosby; p. 346-376.
9. Costenbader FD. In: Allen JH, The physiology and management of divergent strabismus. Strabisumus ophthalmic symposium I. 1950. St. Louis: Mosby; p. 349-354.
10. Cho YA, Shin HS, Joo HS, Jung HR. Surgical treatment of intermittent exotropia. J Korean Ophthalmol Soc 1987;28:1315-1322.
11. Kwak MS, Kwon JY, Kim SY. A clinical study on exodeviation. J Korean Ophthalmol Soc 1994;35:95-102.
12. Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Opthalmol 1978;96:268-274.

13. Schlossman A, Muchnick RS, Stern KS. The surgical management of intermittent exotropia in adults. Ophthalmology 1983;90:1166-1171.


14. Wirtschafter JD, Von Noorden GK. The effect of increasing luminance on exodeviations. Invest Ophthalmol 1964;3:549.
15. Manley DR. In: Manley DR, Classification of the exodeviations. Symposium on horizontal ocular deviation. 1971. St. Louis: Mosby; p. 128.
- TOOLS
-
METRICS

- Related articles
-
Comparison of Retinal Layer Thicknesses of Highly Myopic Eyes and Normal Eyes2020 December;34(6)





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



