 |
 |
| Korean J Ophthalmol > Volume 24(3); 2010 > Article |
To the Editor
Dear Editor,
I write to you with regard to the article by Kim and Park, titled 'Comparison between intravitreal bevacizumab and triamcinolone for macular edema secondary to branch retinal vein occlusion' [1]. Their study compared the effects of standard doses of bevacizumab (1.25 mg) and triamcinolone (4 mg) intravitreally for the treatment of macular edema (ME) secondary to branch retinal vein occlusion (BRVO). The results in terms of improvements in visual acuity and central macular thickness were similar between those treated with intravitreal bevacizumab (IVB) and those treated with intravitreal triamcinolone (IVT). Despite the seemingly promising results, there are two concerns we would like to address.
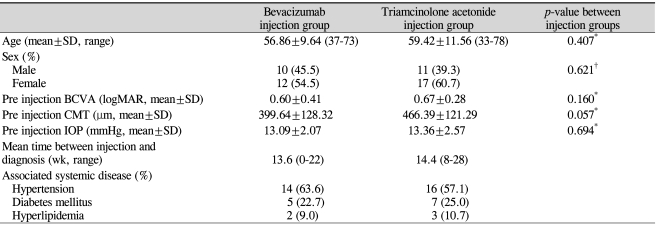
First, subjects were given treatment without being given an observation period to allow for spontaneous resolution. The natural history of BRVO can be variable and can resolve without treatment, especially for cases in which perfusion is re-established after the initial attack. In the classic Branch Vein Occlusion Study (BVOS) [2], subjects were observed for spontaneous resolution for at least 12 weeks, and, in the cases in which resolution was unlikely, treatment was offered. In the current study, both IVB and IVT were given without an observation period in whichspontaneous resolution may occur. Although the mean time from diagnosis to injection was more than 12 weeks in both groups, some patients received injection treatment as early as 0 weeks after diagnosis of BRVO (Table 1) [1]. This may only add potential risks to eyes in which spontaneous resolution can occur. Furthermore, this precluded comparison with the BVOS, since the treatment time frames were different.
Next, the only well-established, evidence-based treatment of choice for macular edema secondary to BRVO is grid laser treatment, according to the BVOS [2] and the recent Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study [3]. In the multi-center randomized trial SCORE study, IVT (either 1 mg or 4 mg) failed to produce a superior effect, when compared to that of subjects who received grid laser treatment, and risk of adverse events was highest in the 4 mg-IVT treatment arm. Hence, to date, grid laser treatment remains the benchmark for other new treatment options in comparing effects in eyes with vision loss due to ME from BRVO [3]. That being said, if the authors intend to demonstrate the effectiveness of IVB, comparison with subjects that had grid laser treatment, rather than IVT, is required.
REFERENCES
1. Kim JY, Park SP. Comparison between intravitreal bevacizumab and triamcinolone for macular edema secondary to branch retinal vein occlusion. Korean J Ophthalmol 2009;23:259-265.



2. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984;98:271-282.


3. Scott IU, Ip MS, Van Veldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol 2009;127:1115-1128.



First, the natural course of branch retinal vein occlusion (BRVO) with macular edema (ME) is now known to be very diverse, resolving without treatment in many cases [1]. Thus, I think that it is right to control the initial treatment period, In this regard, I agree with the comment of Wong I. However, in our study, the mean times and ranges between diagnosis and injection were 14.4 weeks (8 to 28 weeks) in the intravitreal triamcinolone (IVT) group and 13.6 weeks (0 to 22 weeks) in the IVB group. According to the distribution, in most cases, the time frames were more than eight weeks, with only a small number of patients in each group having 0 to 4 weeks between diagnosis and treatment. The distribution tended to be slightly negatively skewed. In addition, there were no differences in the results, even if we excluded these cases with the time frames of 0 to 4 weeks. In conclusion, even if we controlledthe interval between diagnosis and initial treatment, the results suggest that there is no significant difference. However, additional research, including more control subjects, may be warranted.
Secondly, the recent results of the Standard Care vs Corticosteroid for Retinal Vein Occlusion study have shown that, just as we suspected, grid laser treatment is effective and safe treatment [2]. Based on these results, grid laser treatment became the mainstay in the treatment of BRVO with ME [2] and is expected to play an important role in the treatment of other disease entities. Unfortunately, just as Wong I commented, we do not compare our treatment with efficacy and safety of grid laser treatment. However, when with intravitreal bevacizumab (IVB) treatment was introduced and performing off-label uses in many cases, we intend to study the differences in effectiveness and adverse events between IVT and IVB from the viewpoint of "injection" [3-5]. Among the recent studies, Cheng et al. [5] reported similar results to those of our study. Their study is more meaningful with-respect to the "Asian race". Consequently, our study shows that IVB may be a useful treatment option, as compared with IVT, as it results in fewer adverse events. Also, we performed a single injection in each group and showed that the single injection-course of BRVO with ME has special significance.
REFERENCES
1. Kim JY, Park SP. Comparison between intravitreal bevacizumab and triamcinolone for macular edema secondary to branch retinal vein occlusion. Korean J Ophthalmol 2009;23:259-265.

2. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984;98:271-282.


3. Scott IU, Ip MS, Van Veldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol 2009;127:1115-1128.


- TOOLS
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 1,531 View
- 4 Download
- Related articles



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



