A pontine metastatic mass that destroys the abducens nucleus can theoretically cause gaze palsy. However, to the best of our knowledge, there has never been a report of unilateral gaze palsy associated with pontine metastasis, although a few cases of one-and-a-half syndrome and bilateral horizontal gaze paralysis caused by pontine metastases have been reported [1-3]. The authors report a recently observed case of unilateral gaze palsy presumably related to pontine metastasis of breast cancer.
Case Report
A 51-year-old woman with breast cancer presented with progressive diplopia. She had previously been diagnosed with infiltrating ductal carcinoma in her right breast and had known metastases to the liver and bone. She had undergone a palliative right mastectomy and chemotherapy.
When she first complained of horizontal diplopia, headache, and nausea, brain magnetic resonance imaging (MRI) and cerebrospinal fluid analysis revealed no abnormal findings. Her visual acuity was 20/20 in both eyes, and no abnormal findings were detected on slit lamp examination. The light reflex was normal without a relative afferent pupillary defect in either eye. The Hardy-Rand-Rittler test was also normal in both eyes. The alternate prism cover test revealed 10 prism diopters of esotropia in the primary position. On attempted right gaze, both eyes showed a moderate limitation. Both eyes showed no limitation in left gaze.
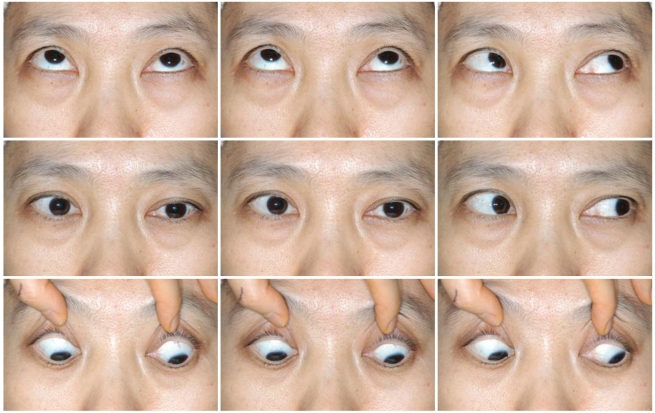
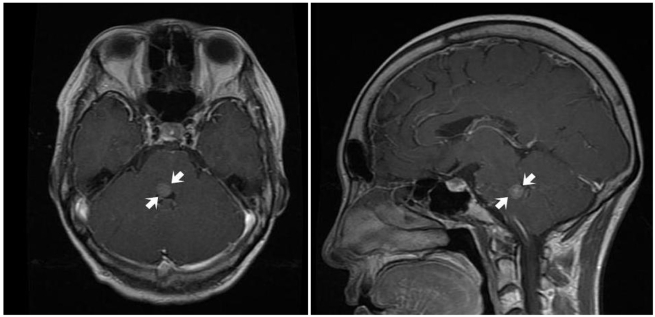
Her diplopia subsequently worsened. Two months later, both eyes were fixed in the midline on attempted right gaze. In contrast, left gaze was preserved in both eyes and vertical eye movements were normal (Fig. 1). She also demonstrated right peripheral facial nerve palsy. Follow-up brain MRI revealed an enhancing round nodular mass at the right facial colliculus of the lower pons, suggesting involvement of either the right abducens nucleus or the paramedian pontine reticular formation (PPRF) along with the facial nucleus or nerve tract (Fig. 2). On neurologic consultation, a solitary metastatic tumor was highly suspected. She was referred to the radiation oncology service for whole brain radiation therapy.
Discussion
The findings in our patient suggested impairment of the right abducens nucleus, which contains both motoneurons that control right eye abduction and internuclear neurons that control left eye adduction [3]. Involvement of the right PPRF could also be inferred given a complete loss of right saccade movements of the right eye [3]. Moreover, the accompanying ipsilateral facial palsy supported the possibility of damage to the right facial nucleus or nerve tract in the vicinity of the abducens nucleus. On MRI, a small tumor was found exactly at the facial colliculus of the lower pons (Fig. 2), where the abducens nucleus and facial nerve tract are located [3,4]. The preservation of adduction of the right eye on left gaze implied that the median longitudinal fasciculus (MLF) was intact.
Pathologic confirmation could not be obtained because we did not think the benefit of biopsy outweighed the risk of pontine injury. However, based on the MRI findings and the slow progression of the neurologic deficits, a pontine tumor was favored. Other potential diagnoses, including pontine hemorrhage, infarction, aneurysm, or demyelination, were excluded. The absence of hypertension and diabetes mellitus as well as an age younger than 55 years also supported the diagnosis.
The possibility of a primary tumor could not be completely ruled out. However, the patient's history of liver and bone metastases along with a previous report indicating that brain metastasis was detectable in up to 30% of patients with breast cancer strongly supported the possibility of a metastatic lesion [5]. In addition, metastatic brain tumors have been reported to be at least four times as common as primary brain tumors, and breast cancer is known to be the second most common cause of brain metastasis [6,7]. Yen et al. [8] reported that the incidence of brainstem involvement in patients with breast cancer metastasis to the brain was as high as 12.4%, higher than that in patients with any other type of cancer. Lee et al. [9] reported that 28% of cases of brain metastasis in breast cancer showed a single metastatic lesion, supporting the idea that a single brain lesion does not necessarily suggest a primary tumor. Moreover, brainstem gliomas, the most common primary tumor of the brainstem, are usually slow-growing and progressive over several years; the rapid growth in only three months also supported the diagnosis of metastatic cancer [10].
Neoplasm is known to be one of the causes of abducens nerve palsy and internuclear ophthalmoplegia [2]. However, to the best of our knowledge, this is the first report of unilateral conjugate gaze palsy due to a pontine metastatic mass. While gaze palsy caused by herpes zoster infection or pontine hemorrhage has been reported, this is the first report of unilateral horizontal gaze palsy due to metastasis to the abducens nucleus [11,12].
In conclusion, a localized metastasis to the abducens nucleus that spares the MLF can cause gaze palsy in a patient with breast cancer.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






