Castleman's Disease Presenting with Uveal Effusion Syndrome
Article information
Abstract
We report a rare case of multicentric Castleman's disease that presented with ophthalmic involvement, along with a review of the literature. A 63-year-old male presented with decreased visual acuity in both eyes. Both eyes had serous elevations of the retinas with shifting subretinal fluid and annular choroidal detachment. No retinal breaks were found. Laboratory tests revealed pancytopenia, hypergammaglobulinemia, and an increased erythrocyte sedimentation rate. Chest and abdominal computed tomographies showed multiple lymphadenopathies in the mediastinum, abdomen, and in both inguinal areas. Histological examination of the inguinal lymph node biopsy was consistent with Castleman's disease. After combination chemotherapy, the serous elevations of both retinas and the annular choroidal detachments of both eyes disappeared. Ophthalmic involvement in Castleman's disease is very rare, and to the authors' knowledge, this is the first report of ophthalmic involvement of Castlemans's disease in Korea.
Castleman's disease is a rare, atypical lymphoproliferative disorder. It was first described by Benjamin Castleman in 1956 as a 'localized mediastinal lymph node hyperplasia resembling a thymoma' [1]. Pathologically, the disease is classified into two types, hyaline-vascular disease and plasma cell disease [2]. Clinically, Castleman's disease can be divided into two different categories, unicentric and multicentric. Unicentric, or localized disease, presents with a solitary mass, most commonly found in the mediastinum. Multicentric, or systemic disease, presents with generalized lymphadenopathy and may involve the liver, spleen, or other organs and tissues [3]. However, the exact cause of this disease remains unknown.
Ocular involvement in Castleman's disease is very rare, and we were only able to uncover four such cases in the literature [4-7]. The current report documents the first case of multicentric Castleman's disease with intraocular involvement in a Korean patient.
Case Report
A 63-year-old man with a 20-year history of diabetes mellitus was referred for surgical treatment of rhegmatogenous retinal detachments in both eyes. His chief complaint was the deterioration of visual acuity in both eyes that had begun four days prior to his presentation. His visual acuity allowed only the visualization of hand motions at 20 cm in the right eye and was 20/200 in the left eye, while his intraocular pressures were 17 mmHg and 14 mmHg in the right and left eyes, respectively
Slit-lamp examinations of the anterior segment and anterior vitreous showed no specific findings in either eye. On dilated fundoscopic examination, both eyes were found to have serous elevations of the retina, with shifting of the subretinal fluid, and multiple retinal hemorrhages. Furthermore, the left eye had an annular choroidal detachment; however, no retinal breaks were found (Fig. 1). Fluorescein angiography demonstrated hypofluorescence in the early phase and hyperfluorescence in the late phase resulting from leakage of fluorescein dye into the subretinal space, in addition to multiple microaneurysms resulting from his preexisting diabetic retinopathy (Fig. 2). Optical coherence tomography images through the foveas of both eyes revealed severe cystic changes in the foveal areas and elevations of the retinal pigment epithelium (Fig. 3). Magnetic resonance imaging showed elevations of the eyeball contour due to the choroidal detachment (Fig. 4).

A fundus photograph of the left eye. Peripheral annular choroidal detachment, shallow detachment of the retina and multiple retinal hemorrhages and exudates due to the underlying diabetic retinopathy are shown.
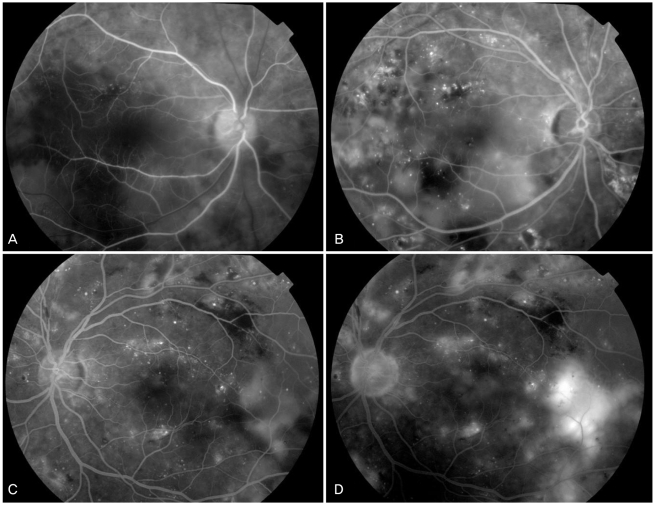
Fluorescein angiography (FAG) of both eyes revealed numerous fluorescent blotches in the subretinal space. FAG demonstrated hypofluorescence in the early phase and hyperfluorescence in the late phase resulting from leakage of fluorescein dye into the subretinal space, in addition to multiple microaneurysms resulting from diabetic retinopathy. (A) Early phase (right eye). (B) Late phase (right eye). (C) Early phase (left eye). (D) Late phase (left eye).
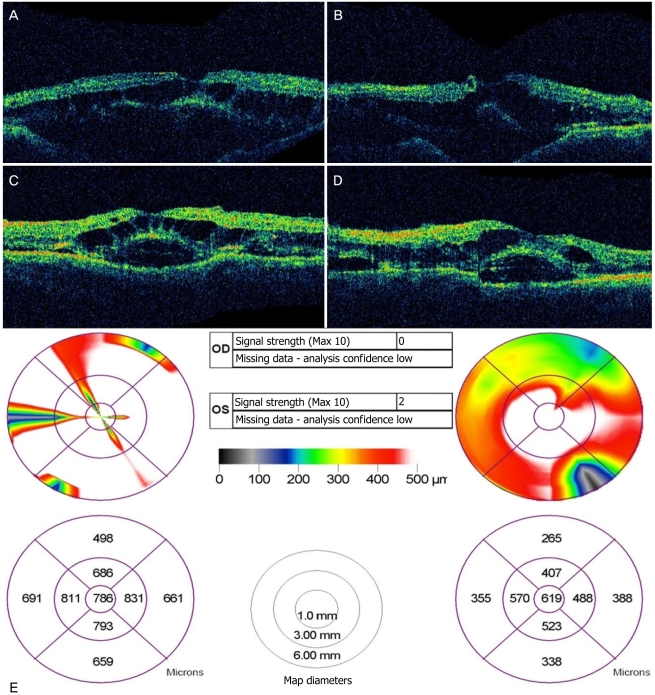
Optical coherence tomography images through the foveas of both eyes revealed severe cystic changes in the foveal area and a high elevation of the neurosensory retina and the retinal pigment epithelium. (A,B) Retinal map of the right eye. (C,D) Retinal map of the left eye. (E) Retinal thickness map of both eyes. OD=oculus dexter; OS=oculus sinister.
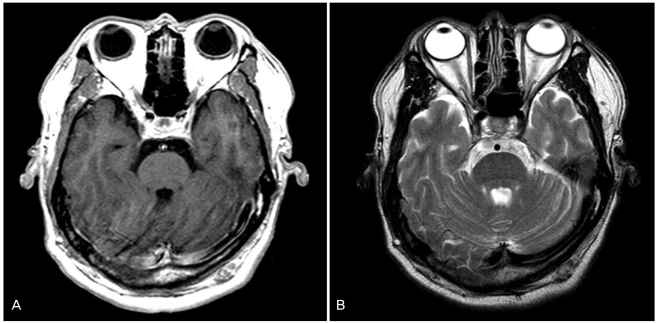
Magnetic resonance imaging. The eyeball size and scleral thickness are normal in both eyes. (A) T1-weighted image, choroidal detachment shown in the left eye. (B) T2-weighted image.
Laboratory abnormalities included pancytopenia, hypergammaglobulinemia, increased erythrocyte sedimentation rate and cerebrospinal fluid pressure (24 cmH2O), and a positive perinuclear antineutrophil cytoplasmatic antibody test. The chest and abdominal computed tomographies showed multiple lymphadenopathies in the mediastinum, abdomen, and in both inguinal areas. An inguinal lymph node biopsy was performed, and Castleman's disease was diagnosed based on the histopathologic findings. Combination chemotherapy was initiated using cyclophosphamide, doxorubicin, vincristine, and prednisolone. Following the combination chemotherapy, the serous elevation of the retina and the annular choroidal detachment of both eyes disappeared. The patient's visual acuity improved to 20/50 in the right eye and to 20/63 in the left eye.
Discussion
Castleman's disease is a rare disorder characterized by cancerous growths within lymph node tissues throughout the body. Commonly, the mediastinal lymph node is affected [8]. Castleman's disease is divided into two main types, including the hyaline-vascular type and the plasma cell type [2]. The hyaline-vascular type comprises approximately 90% of unicentric cases, in which patients present with a solitary mass, and the disease typically follows a benign course [9]. Most patients with unicentric Castleman's disease can be treated with complete surgical ablation [10]. In contrast, the plasma cell type develops in a multicentric fashion, and patients suffer systemic symptoms including fever, weight loss, anemia, and hypergammaglobulinemia [8]. The multicentric form is associated with polyneuropathy, organomegaly, endoclinopathy, monoclonal proteinemia, skin changes, Hodgkin's disease, Kaposi's sarcoma, and acquired immunodeficiency syndrome [11]. Lymphoma and Kaposi's sarcoma have been reported to arise in as many as 32% of patients with multicentric Castleman's disease [2,9,10]. Multicentric Castleman's disease with systemic manifestations is more difficult to treat than is the unicentric disease. Radiotherapy or steroid therapy is often used as a treatment, and combination chemotherapy is used in patients who do not respond to steroid therapy [12].
To our knowledge, ophthalmic involvement in Castleman's disease is very rare. Four cases of ophthalmic involvement have been reported in the literature [4-7]. Three cases reported orbital masses diagnosed as Castleman's disease [5-7], while the final case reported a serous retinal detachment along with choroidal thickening [4]. In our case, after combination chemotherapy for multicentric Castleman's disease, the serous elevation of the retina and the annular choroidal detachments of both eyes disappeared. Although Castleman's disease is very rare and its exact mechanism of serous retinal detachment and choroidal detachment is unknown, it should be considered in the differential diagnosis of choroidal detachment.
Notes
No potential conflict of interest relevant to this article was reported.