 |
 |
| Korean J Ophthalmol > Volume 23(3); 2009 > Article |
Abstract
We report three cases of neovascular glaucoma secondary to central retinal artery occlusion (CRAO) which were effectively managed with intravitreal bevacizumab (IVB) followed by panretinal photocoagulation (PRP). Neovascular glaucoma without peripheral anterior synechiae developed between one and five weeks following CRAO onset. All patients received 0.75 mg (0.03 ml) IVB. In all patients, complete regression of the iris and anterior chamber angle neovascularization was confirmed within one week. PRP was applied two weeks after the injection. The follow-up period was four to seven months (average, five months). Intraocular pressure was controlled in all patients using topical antiglaucoma medications alone. However, one patient experienced a recurrence of neovascularization three months after the initial combination treatment. This patient received another IVB injection and additional PRP, and the recurrent neovascularization resolved. There were no local or systemic adverse events in any patients. Therefore, intravitreal bevacizumab may be an effective adjunct in the treatment of neovascular glaucoma associated with CRAO.
Ischemic retinopathies can cause new vessel growth on the iris and anterior chamber angle that can lead to neovascular glaucoma (NVG). Central retinal artery occlusion (CRAO) can also cause neovascularization of the iris (NVI) and NVG as a result of ocular ischemia, with an incidence of 1 to 20%.1-3 The disease management usually attempts to control the ocular ischemia using panretinal photocoagulation (PRP).4 However, PRP often takes several weeks to induce neovascular regression. During this period, progressive angle closure and optic nerve damage may occur as a result of the elevated intra-ocular pressure (IOP).5
Recently, the pathogenesis of NVG has been linked to a locally produced angiogenic growth factor: vascular endothelial growth factor (VEGF).6 Intravitreal administration of bevacizumab (Avastin, Genentech, Inc., San Francisco, CA, USA), a recombinant anti-VEGF, has been reported to be beneficial in the treatment of NVG. In a review of the literature, we noted that bevacizumab causes early-onset neovascular regression in less than one week, and that regression of the NVI may persist for four to ten weeks because of its short duration lasting for four weeks.7-11 Given the chronic nature of the ischemic drive in NVG and the rapid decline of the effects of bevacizumab, a combination therapy of intravitreal bevacizumab (IVB) with early onset neovascular regression and PRP with a long duration of action might be useful in managing NVG.5,12 Therefore, we used a combination of IVB and PRP for the treatment of new-onset NVG associated with CRAO.
Thus far, there has been no report in the Korean literature addressing the use of combination IVB/PRP in the treatment of NVG. There has only been one case report describing the utility of bevacizumab in one PRP-treated eye with a history of proliferative diabetic retinopathy.11 We describe three cases of NVG following CRAO treated with combination IVB/PRP.
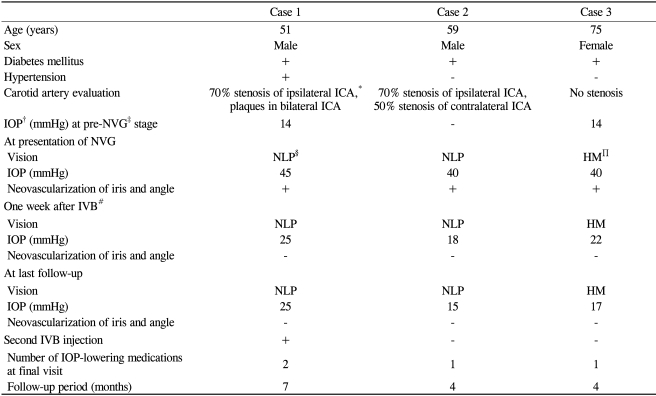
A 51-year-old man with known mild, bilateral nonproliferative diabetic retinopathy was referred for evaluation of CRAO that had developed in his left eye 72 hours prior to presentation. His past medical history included systemic arterial hypertension and diabetes mellitus for the past 15 years.
On examination, his best-corrected visual acuity was 0.6 in the right eye and hand motion in the left eye. Intraocular pressure (IOP) was 14 mmHg bilaterally by Goldmann applanation tonometry. Anterior segment evaluation showed no NVI in the left eye, and both eyes had open angles. Fundus examination showed midperipheral retinal hemorrhages in both eyes. In the left eye, the retina was pale with attenuated arteries and a cherry red spot at the posterior pole. An intravenous fluorescein angiogram showed a delayed arm-to-retina time of 25 seconds and incomplete retinal venous filling throughout the test (>6 minutes). Choroidal perfusion was normal. Noninvasive carotid examination delineated 70% stenosis in the left proximal internal carotid artery and plaques in both internal carotid arteries.
Five weeks later, on routine follow-up examination, he returned complaining of ocular pain in his left eye for the previous three days. The visual acuity in the left eye had decreased to no light perception, and the IOP was 45 mmHg. Neovascularization of the iris and angle was noted in the left eye. The retinal whitening and cherry red spot were still present.
Despite maximal tolerable medical therapy to control intraocular pressure, the patient experienced marked discomfort. Treatment options were explained in detail, and after the patient gave consent, an intravitreal injection of 0.75 mg (0.03 ml) of bevacizumab was performed in a sterile fashion without anterior chamber paracentesis. One week later, there was a complete regression of the NVI, and the IOP had decreased to 25 mmHg with two topical antiglaucoma medications (dorzolamide/timolol fixed combination and brimonidine). PRP consisting of a total of 1200 burns was administered in three sessions starting two weeks after the injection. Over the next three months, recurrent NVI developed, and the patient received another IVB injection and additional PRP. Over the course of treatment, the patient received 2000 burns in all. Two months after the additional combination therapy, there was no recurrence of NVI, and the IOP was 21 mmHg with the same medications.
A 59-year-old man with a ten-year history of diabetes mellitus was referred for evaluation of decreased vision in the previous two weeks and ocular pain for three days. He was normally followed for mild diabetic retinopathy in both eyes for the past two years.
On examination, his best-corrected visual acuity was no light perception in the right eye and 0.8 in the left eye. IOPs were 40 mmHg in the right eye and 18 mmHg in the left eye by Goldmann applanation tonometry. Anterior segment evaluation revealed neovascularization of the iris and angle in the right eye. Fundus examination showed CRAO characterized by retinal whitening with attenuated arteries and a cherry red spot at the posterior pole in the right eye. Both eyes had midperipheral retinal hemorrhages. Fluorescein angiography showed normal choroidal filling. Retinal arterial filling began at 30 seconds after injection, and the retinal vein was not completely filled even late in the angiogram. A noninvasive carotid examination revealed 70% stenosis of the right internal carotid artery and 50% stenosis of the left internal carotid artery.
After obtaining informed consent, bevacizumab (0.75 mg/0.03 ml) was injected. One week after the injection, the NVI had regressed, and the IOP was 18 mmHg/AT with two topical antiglaucoma medications (dorzolamide/timolol fixed combination and brimonidine). PRP was started two weeks after the injection. The patient received 1800 burns overfour sessions. Four months later, there was no recurrent neovascularization, and the IOP was 15 mmHg with one topical antiglaucoma medication (dorzolamide/timolol fixed combination).
A 75-year-old woman presented with a ten-day history of decreased visual acuity in her right eye. Her past medical history included diabetes mellitus for the last five years.
Her visual acuity was hand motion in the right eye and 0.9 in the left eye. IOPs were 14 mmHg in the right eye and 12 mmHg in the left eye by Goldmann applanation tonometry. There was no anterior chamber reaction or NVI in the right eye. The right fundus showed a CRAO characterized by retinal opacification of the posterior pole with a cherry red spot. No clinical evidence of diabetic retinopathy was present in either eye. Fluorescein angiography showed sluggish retinal arterial flow and delayed retinal venous filling. Noninvasive carotid examination showed no evidence of obstruction.
Two weeks later, the patient returned for a follow-up examination. Her visual acuity in the right eye remained hand motion. However, the right eye now exhibited NVI and had an IOP of 40 mmHg. The retinal opacification was still present. After obtaining informed consent, bevacizumab (0.75 mg/0.03 ml) was injected. One week after the injection, the NVI had regressed, and the IOP had decreased to 22 mmHg with two topical antiglaucoma medications (dorzolamide/timolol fixed combination and brimonidine). PRP was performed in the right eye two weeks after the injection. The patient received 1600 burns over four sessions. Four months after combination therapy, the visual acuity remained hand motion with no recurrent neovascularization. The IOP was 17 mmHg with one topical antiglaucoma medication (dorzolamide/timolol fixed combination).
NVI and the subsequent development of NVG are serious complications seen in patients with ischemic retinal disorders such as proliferative diabetic retinopathy, central retinal vein occlusion and central retinal artery occlusion.4 The incidence of NVI or NVG secondary to CRAO has been reported to be in the range of 1 to 20%.1-3 We reviewed 36 CRAO patients seen over a four-year period from January 2004 to August 2008. Based on our data, the incidence of NVI or NVG after CRAO was 19.4% (7 of 36). This figure may actually be less than the true incidence because all 36 patients were not followed-up completely; some of them might have developed NVI or NVG after discontinuing follow-up. There were seven patients who had NVI or NVG after CRAO, and this report describes three patients with NVG treated with combination IVB/PRP therapy.
The evidence implicating CRAO as the cause of NVG is strong. No ocular neovascularization was present in any of the three cases at the time of CRAO. NVI appeared de novo as early as two to five weeks after the initial presentation of CRAO. At the time of the initial CRAO, Cases 1 and 2 had only mild, nonproliferative diabetic retinopathy, and Case 3 had no diabetic retinopathy upon clinical examination or fluorescein angiography. Ocular ischemic syndrome was ruled out completely in Case 3, who showed no evidence of carotid artery stenosis. Cases1 and 2 both had some degree of carotid artery stenosis, but the obstruction did not approach the 90% or greater blockage that is necessary to induce ocular ischemic syndrome.13 More importantly, there was no delayed choroidal filling on fluorescein angiography in any of the three cases.
NVI and NVG are highly correlated with retinal ischemia, which stimulates the production of vascular endothelial growth factor (VEGF), a key molecule in ocular neovascularization.6,14 Tripathi et al.6 reported that the level of VEGF in the aqueous humor is significantly increased in patients with NVI and NVG, and that inhibition of endogenous VEGF is effective in suppressing retinal ischemia-induced NVI. Currently, PRP is the gold standard for initial treatment.4,15,16 VEGF levels are indirectly reduced after PRP in patients with ischemic retinal disorders.6 However, PRP alone is not completely successful in halting NVI in every patient, especially those with severe and rapid neovascular progression.4 Duker and Brown15 reported regression in 65% of patients after PRP for treatment of NVI secondary to CRAO. Therefore, direct targeting of VEGF with anti-VEGF pharmacotherapy may be another possible therapeutic strategy in the treatment of ocular neovascularization.17
Bevacizumab is a full-length humanized monoclonal antibody that binds with all isoforms of VEGF.18 Some studies have reported on the short-term efficacy and safety of off-label IVB in the treatment for NVI and NVG.9-11 A marked regression of NVI has been shown to occur within one to two weeks after the injection. IOP was controlled for the short follow-up period in most patients, even those with early-stage NVG. However, the effect of bevacizumab on the regression of NVI may be transient due to the drug's short duration of action.7,8
Several recent studies have addressed combination IVB/PRP therapy for the treatment of NVG.5,12,19 A combination of IVB and PRP can theoretically offer the advantage of early onset neovascular regression from the bevacizumab and a long duration of action from the PRP.5 In a study comparing same-day combination IVB (1.25 mg/0.05 ml)/PRP with PRP alone for the treatment of new onset NVG, Ehlers et al.5 reported that the combination treatment group showed a significantly higher frequency and rate of neovascular regression and a significantly reduced IOP compared to the PRP-alone group. Gheith et al.12 reported six cases of NVG treated with IVB (1.25 mg/0.05 ml) that were then followed by PRP approximately one week later. In all cases, NVI completely regressed after initial combination therapy. However, two cases had a recurrence of NVI after three months and five months, respectively. These patients initially had inadequate PRP, and the neovascularization recurred when the effect of the bevacizumab wore off.
Based on these observations, we chose to administer combination IVB/PRP therapy. Although the optimum IVB dose remains to be established, previous studies have described using up to 2.5 mg without serious adverse systemic or ocular events.20,21 Recent reports have suggested that even smaller doses may be sufficient to inhibit intravitreal VEGF and neovascular proliferation.7,22 Therefore, we performed an injection of 0.75 mg of bevacizumab, representing 0.03 ml of a 25 mg/ml concentration, in all patients as an initial treatment for NVG. All injections were done without anterior chamber paracentesis to avoid its related complications after maximal tolerable medical therapy, including mannitolization for elevated IOP. Considering the short duration of action associated with small amounts of bevacizumab, PRP was routinely started approximately two weeks after IVB injection to achieve long-lasting neovascular regression. In all of our cases, NVI had completely resolved within one week after the initial injection of IVB. NVI regression persisted four months later in two of our cases (Cases 2 and 3) who received a single injection of IVB followed by PRP. However, Case 1 showed an NVI recurrence after three months. This patient received another IVB injection with additional PRP, which resulted in the resolution of the recurrent NVI. It is possible that, in this patient, subsequent PRP was scheduled but was not completed. Because NVI as the main indicator for adequate PRP disappears after the initial IVB, the amount of subsequent PRP required may have been underestimated.
Recently, Wakabayashi et al.23 reported a large case study in which the patients were followed-up for six to 22 months. In the NVI-only group, recurrent NVI was resolved by repeat IVB and additional PRP without the development of NVG. In the open-angle NVG group, 41% of the patients eventually required surgical intervention to stabilize their elevated IOPs, despite repeat IVB and PRP and in the closed-angle NVG group, 93% of the patients underwent surgery. These findings indicate that IVB may be effective as the first treatment of choice for eyes with NVI and early-stage NVG, but it may be insufficient for treating eyes in a pathologically-advanced stage of NVG. Our three cases had open-angle NVG associated with CRAO. In all of these cases, IOP was controlled with topical antiglaucoma medications alone without surgical intervention.
In conclusion, we recommend that all CRAO patients be followed closely for several months after obstruction, with specific attention directed toward the development of NVI and NVG. If NVI or NVG is present, combination IVB/PRP therapy should be considered. Our report suggests that IVB may be valuable in the treatment of NVG because it speeds up the resolution of NVI. Furthermore, IVB appears to provide long-term control when used in combination with PRP. This report emphasizes the need for further prospective, long-term, randomized studies examining PRP-only, IVB-only, and IVB/PRP combination therapy for the treatment of NVG.
Notes
The contents in this paper were presented in the 100th Annual Meeting of the Korean Ophthalmological Society, October 2008, Ilsan, Korea.
REFERENCES
1. Gartner S, Henkind P. Neovascularization of the iris (rubeosis iridis). Surv Ophthalmol 1978;22:291-312.


2. Duker JS, Brown GC. Neovascularization of the optic nerve associated with obstruction of the central retinal artery. Ophthalmology 1989;96:87-91.


3. Hayreh SS, Podhajsky P. Ocular neovascularization with retinal vascular occlusion. II. Occurrence in central and branch retinal artery occlusion. Arch Ophthalmol 1982;100:1585-1596.


4. Sivak-Callcott JA, O'Day DM, Gass JD, Tsai JC. Evidence-based recommendations for the diagnosis and treatment of neovascular glaucoma. Ophthalmology 2001;108:1767-1776.


5. Ehlers JP, Spirn MJ, Lam A, et al. Comparison intravitreal bevacizumab/panretinal photocoagulation versus panretinal photocoagulation alone in the treatment of neovascular glaucoma. Retina 2008;28:696-702.


6. Tripathi RC, Li J, Tripathi BJ, et al. Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma. Ophthalmology 1998;105:232-237.


7. Beer PM, Wong SJ, Hammad AM, et al. Vitreous levels of unbound bevacizumab and unbound vascular endothelial growth factor in two patients. Retina 2006;26:871-876.


8. Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 2007;114:855-859.


9. Iliev ME, Domig D, Wolf-Schnurrbursch U, et al. Intravitreal bevacizumab (Avastin) in the treatment of neovascular glaucoma. Am J Ophthalmol 2006;142:1054-1056.


10. Chilov MN, Grigg JR, Playfair TJ. Bevacizumab (Avastin) for the treatment of neovascular glaucoma. Clin Experiment Ophthalmol 2007;35:494-496.


11. Maeng H, Kim J, Kee C. Intravitreal bevacizumab (Avastin) injection for the treatment of early-stage neovascular glaucoma. J Korean Ophthalmol Soc 2008;49:696-700.

12. Gheith ME, Siam GA, Barros MD, et al. Role of intravitreal bevacizumab in neovascular glaucoma. J Ocul Pharmacol Ther 2007;23:487-491.


13. Brown GC, Magargal LE, Simeone FA, et al. Arterial obstruction and ocular neovascularization. Ophthalmology 1982;89:139-146.


14. Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 1994;331:1480-1487.


15. Duker JS, Brown GC. The efficacy of panretinal photocoagulation for neovascularization of the iris after central retinal artery obstruction. Ophthalmology 1989;96:92-95.


16. Laatikainen L. A prospective follow-up study of panretinal photocoagulation in preventing neovascular glaucoma following ischaemic central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 1983;220:236-239.


17. Ferrara N. Role of vascular endothelial growth factor in physiologic and pathologic angiogenesis: therapeutic implications. Semin Oncol 2002;29(suppl):10-14.

18. Ferrara N, Hillan KJ, Gerber HP, Novotny W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov 2004;3:391-400.


19. Vatavuk Z, Mandic BZ. Intravitreal bevacizumab for neovascular glaucoma following central retinal artery occlusion. Eur J Ophthalmol 2007;17:269-271.


20. Lynch SS, Cheng CM. Bevacizumab for neovascular ocular diseases. Ann Pharmacother 2007;41:614-625.


21. Fung AE, Rosenfeld PJ, Reichel E. The international intravitreal bevacizumab safety survey: using the internet to assess drug safety worldwide. Br J Ophthalmol 2006;90:1344-1349.



- TOOLS
-
METRICS

- Related articles
-
Neovascular Glaucoma Associated with Chronic Rhegmatogenous Retinal Detachment2023 June;37(3)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



