The Comparison of Central and Mean True-Net Power (Pentacam) in Calculating IOL-Power After Refractive Surgery
Article information
Abstract
Purpose
To compare the accuracy of central true net corneal power (cTNP) and mean true net corneal power (mTNP) of the Pentacam system to give a keratometry (K) reading for calculating IOL (intraocular lens) power in eyes following refractive surgery.
Methods
Refraction, an automated K-reading (Km), cTNP and mTNP were measured for 15 eyes that required cataract surgery and had previously undergone refractive surgery. The difference between postoperative manifest refraction values and target refraction values calculated with the SRK/T formula using cTNP were compared with the one using mTNP.
Results
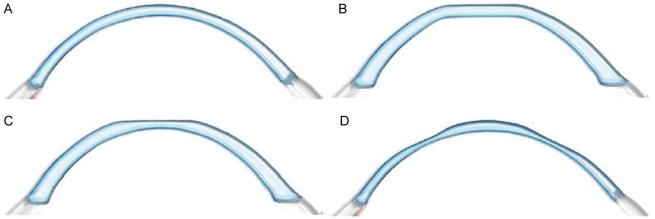
The mean deviation from the desired post-cataract refractive outcome was 0.60 diopter (D) ±0.47 (standard deviation) using cTNP; 0.75±0.54 using mTNP (p=0.386). The actual refraction was within ±0.50D of the intended refraction for 60% (cTNP) and 33.3% (mTNP) of eyes, and within ±1.00D for 93% (cTNP) and 66.7% (mTNP) of eyes.
Conclusions
Although not statistically significant, the cTNP showed better accuracy than mTNP to give a keratometry (K) reading for post-refractive surgery eyes requiring cataract surgery.
As patients who have previously undergone refractive surgery age, the incidence of cataracts increases. In some cases, refractive surprise has been observed after cataract surgery.1 A residual hyperopia was found in patients who had undergone previous myopic refractive surgery, but the reason for this error is not clear. It has been suggested that formulas for intraocular lens (IOL) power calculation may not be appropriate in these patients2-4 and/or that the corneal power may be incorrectly measured.5-12
Several solutions for reducing this postoperative refractive error have been proposed, and they can be categorized into two groups. The first group involves acquiring accurate corneal power, while the second group involves a special formula for the IOL calculation.
Myopic refractive surgery deliberately modifies the shape of the anterior surface of the cornea and its thickness to correct a refractive defect, and the normal prolate anterior surface is converted to an oblate surface. Therefore, it may not be appropriate to apply conventional variables developed for normal corneas to surgically modified corneas. Consequently, for these cases, measuring the true corneal power is critical for IOL power calculations.
The methods for acquiring accurate corneal power can also be divided into two groups based on whether or not pre-refractive surgery data are required. Methods requiring pre-refractive surgery include the clinical history method,13 the Feiz-Mannis method,14 and the cornea bypass method;15 methods that do not require preoperative data include the contact lens method and direct measurement using Orbscan topography16 or the Pentacam system. The most common drawback to the methods requiring pre-refractive surgery data lies in a loss of data owing to the long intervals between the corneal refractive procedure and cataract surgery. Contact lens over-refraction methods could also be inaccurate due to the presence of the cataract itself and the meniscus between the back surface of the contact lens and the anterior surface of the cornea, which can eventually induce a myopic shift in refraction.17
The Haigis-L formula has recently been developed for IOL calculations for post-refractive surgery patients. The formula is undergoing verification, but it needs special equipment such as an IOL Master. Therefore, direct corneal power measurement methods that do not require pre-refractive surgery data are usually more convenient and easily available for cataract surgery after refractive surgery.
The ability to measure the accurate true corneal power after refractive surgery without collecting preoperative data would provide new opportunities for the management of patients who need cataract after refractive surgery. The Pentacam (Oculus, Wetzler, Germany) anterior segment imaging system that uses a rotating Scheimpflug camera can be used to measure both the anterior and posterior corneal curvatures. This device ascertains corneal power from both anterior and posterior corneal surface measurements, whereas the Orbscan system has problems capturing images and computing the back curvature of the cornea.16,18,19 A "true net power map" that shows the refractive power of the cornea at any given point (The instrument calculates the refractive power of both surfaces and adds them together).
In the present study, we compared the accuracy of the central K-value calculated from the true net power map (cTNP) with the mean K-value (mTNP) of the Pentacam system to give a keratometry (K) reading for calculating IOL (intraocular lens) power in post-refractive surgery eyes.
Materials and Methods
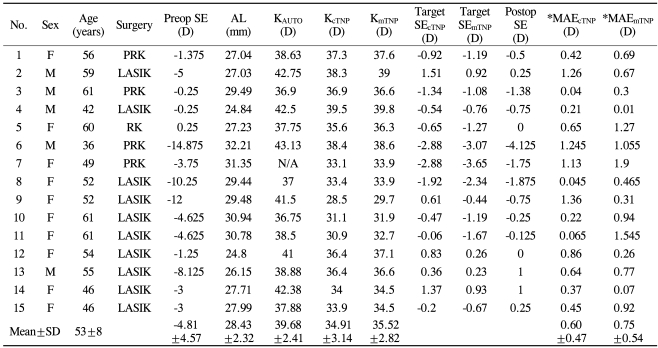
Data were collected from 15 eyes of 12 patients (6 women and 6 men) who had had refractive surgery for the treatment of myopia. Eyes were excluded that had previously undergone other corneal or intraocular surgery or which had severe dryness, which affected the quality of the Pentacam. Keratometric data for IOL calculations for cataract surgery were obtained using the Pentacam true net power assessment. The exact central value and mean of nine keratometric values within a 3-mm zone in the true net power map of the Pentacam were selected as the K-value and compared (Fig. 1). The axial length of the eye was measured using a Sonomed 5500 Digital A/B Scan (Latham and Phillips Ophthalmic Products Inc., OH, USA).
Screen-map shot of the true net power map of the Pentacam system. The exact central K-value in the true net power map was used in this study.
The power of the IOL to be implanted during cataract surgery was calculated using the SRK/T formula, and the IOL power was finally determined by a surgeon. Six weeks after cataract surgery, postoperative manifest refraction was obtained. The mean absolute differences between the achieved postoperative refraction and the target refraction using cTNP and mTNP were analyzed with a statistical software program, SPSS V 12.0 (SPSS Inc, Chicago, IL, USA).
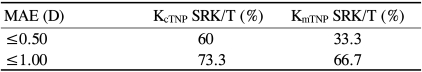
Preoperative and postoperative data from 15 eyes (12 patients) were evaluated. Mean patient age was 53.0±8.0 years. A total of 10 eyes had undergone myopic laser-assisted in situ keratomileusis (LASIK), four eyes had had myopic PRK (photorefractive keratectomy) and one eye had had an RK (radial keratotomy). The mean preoperative refraction was -4.81±4.57 diopters (D), and the mean axial length was 28.43±2.32 mm. The mean corneal power measured using the true net power of Pentacam was 34.91±3.14D (cTNP); 35.52±2.82D (mTNP) and the mean auto-keratometry corneal power was 39.68±2.41D (Table 1). There was a statistically significant difference between the corneal power measured with Pentacam and that measured with auto-keratometry (mean difference 4.63±3.30D, Mann Whitney U test, p<0.01 (cTNP); 4.05±2.97D, p<0.01 (mTNP). The mean deviation from the desired post-cataract refractive outcome (mean absolute error; MAE) was 0.60±0.47D (cTNP); 0.75±0.54D (mTNP) and statistically there was no difference between intended target refractive error and postoperative refractive error (the Mann Whitney U test, p=0.386). The proportion of eyes within <0.5D refractive errors compared with the intended postoperative refraction was 60% (cTNP); 33.3% (mTNP), and the proportion of eyes within <1.0D was reached to 93% (cTNP); 66.7% (mTNP) (Table 2).
There is a no statistically significant difference between the cMAE and the mMAE (p=0.386); however, the cTNP might be a better tool than the mTNP to give a keratometry (K) reading for post-refractive surgery eyes requiring cataract surgery.
Discussion
Patients who have previously undergone refractive surgery have high expectations about visual outcomes after cataract surgery. Unfortunately, postoperative refractive errors are less predictable in these patients than in those that have not had prior surgery, despite the assistance of various compensatory methods. Unpredicted consequences of cataract surgery are most likely due to inaccurate measurements of the corneal power of eyes after refractive surgery.5,11,20,21
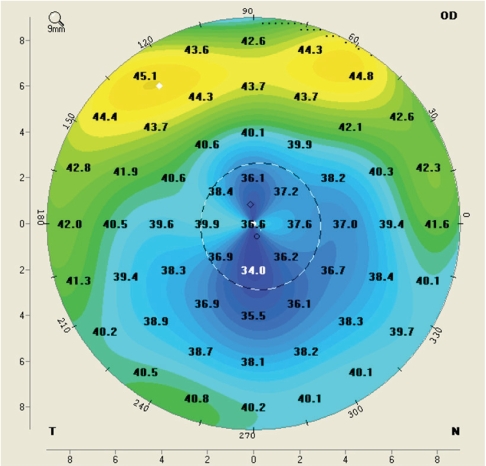
An alteration in the geometric relationship between anterior and posterior corneal curvatures makes traditional keratometry, which requires almost parallel anterior and posterior corneal surfaces, unreliable. The assumption that the distance between the anterior and posterior curvatures is a constant cannot be applied to post-refractive corneas. Figure 2 shows the schematic conceptual relationship between the anterior and posterior corneal curvatures in the unoperated eye and also in eyes that have been subjected to keratorefractive surgery.22 Figure 2B simulates the change after radial keratotomy; note that both the anterior and posterior surfaces have been flattened by the surgery, a result which is distinctly different from the effects of excimer laser photoablation. As a result, IOL power calculation formulas after radial keratotomy (RK) differ from those used after laser ablation; the former are not considered in the current investigation because the mechanisms of IOL power inaccuracy vary between RK and laser ablative refractive surgery. As noted in Figure 2C, the effect of excimer laser ablation for the correction of myopia induces a flattening of the anterior corneal surface. As a result, the posterior and anterior corneal surfaces are no longer parallel, and the back surface power value relative to the anterior corneal curvature increases. Keratometers and topographers usually misread the postexcimer-ablated cornea because they read only the anterior corneal surface and assume an approximately preset-6.0D power for the back corneal surface. Additionally, it has been reported that posterior corneal curvature may increase (because of variable limited ectasia) after myopic laser photoablation.23 Although this phenomenon may also affect the accuracy of corneal power determination with standard devices, there remains no consensus on this subject because the method for reading postoperative posterior corneal curvature with the Orbscan (Bausch & Lomb) has not been validated.24 In contrast to the effect of myopic photoablation (and as shown in Fig. 2D) after hyperopic excimer laser treatment, the anterior corneal power is increased independently of the posterior surface. This can also result in a misinterpretation of corneal power by standard instruments because the back surface will represent a lower value than -6.0D.
(A) Schematic conceptual relationship between the anterior and posterior corneal curvature in the unaffected eye. Note that the two curves are approximately parallel. (B) Schematic conceptual corneal shape change after RK. Note that the two surfaces are near parallel, but they are significantly flatter than the unoperated cornea in A. (C) Schematic conceptualized drawing of corneal shape after excimer photoablation for myopia. Note that the anterior surface is considerably flatter than the posterior surface. (D) Schematic conceptualized drawing of the corneal shape after hyperopic excimer photoablation. Note that the anterior surface is steeper than the posterior surface.
Most topography relies on Placido disc technology and calculates corneal curvatures based on derived slope data. These methods calculate the total power of the cornea by measuring the radius of the corneal anterior surface curvature from a central area with a diameter of approximately 3 mm. Conversion of millimeters of radius to diopters (D) is performed using a theoretical effective (keratometric) refractive index of 1.3375.25 However, the cornea no longer has a normal shape and the paracentral measurements no longer reflect the central power of the eye of a patient who has previously undergone a refractive corneal procedure.
Topography based on direct measurements of corneal elevation points more accurately maps the cornea than Placido-based topography. The Pentacam, an elevation-based diagnostic imaging system, can measure the corneal surface with great accuracy. The Pentacam system uses more measuring points in the central cornea than other systems. The Pentacam's Scheimpflug camera rotates around the center of the cornea, and the reproducibility of the Pentacam's data is ensured by a short measurement time and overlapped images. The precision and reproducibility of this system allow us to appropriately select a K-value (true net corneal power).
Our previous study using the Pentacam system showed a more accurate measurement of the corneal thickness in a post-PRK patient compared with the Orbscan system. This result suggests that the Pentacam system is likely to give a more accurate morphological assessment of the cornea.
In this study, all patients had myopic correction. For universal use of this method for comparing the accuracy of the true corneal power between cTNP and mTNP after a refractive procedure, further study is needed on its application for eyes with hyperopic refractive correction with an accurate IOL calculation formula.26 We compared the predictability of postoperative target refraction between the central and mean of nine keratometric values within a 3-mm zone in the true net power map of the Pentacam. Although there was no significant statistical difference between each methods, the K-value using cTNP might be a better tool than the one that uses mTNP.
We expect this measurement method (using cTNP and mTNP) will be a useful tool for net corneal power estimation and IOL power calculation in patients who have previously undergone refractive surgery but for whom there are no records of preoperative treatment data.
Notes
All of the authors have no financial interest of any materials and methods in this paper.