 |
 |
| Korean J Ophthalmol > Volume 20(1); 2006 > Article |
Abstract
Purpose
To assess the clinical pattern, the histopathological findings, the response to treatments, the recurrence pattern and the prognosis of malignant lymphoma in the ocular adnexa.
Methods
This study was performed on 22 total eyes from 17 patients who were diagnosed with ocular adnexal malignant lymphoma. We retrospectively analyzed the medical records for patient information including the histological classification based on age, the gender of each patient, the symptoms and signs at the initial diagnosis, the presence of binocular invasion, the findings of the surgical biopsy, the clinical stage of each patient's tumor, and the treatment methods used and their effectiveness. The mean follow-up period was 24.8 months.
Results
The mean age of patients studied was 46.8 years old. Six females and 11 males were included in the study. Fifteen cases consisting of 20 total eyes represented extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT). Five of seven patients (71.4%) whose lymphoma occurred within the conjunctiva relapsed after irradiation or chemotherapy, and four of the relapsed patients were salvaged with further therapy.
Conclusions
Extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT) constituted 88.2% of all lymphomas involving the ocular adnexa. Lymphoma in the ocular adnexa responded well to conventional treatment, but the recurrence rate of lymphoma in the conjunctiva was significantly high.
Malignant lymphomas represent approximately 10% of orbital tumors.1-4 In addition, 5-8% of extranodal lymphomas involve the orbit, and 1.3-2.0% of extranodal lymphomas appear as primary orbital tumors.3,5 The incidence of primary orbital tumors has recently been on the rise due to environmental and lifestyle changes as well as to advances in the histopathological diagnostic techniques using immunohistochemical and molecular analysis.1,3-5
After numerous controversies regarding the classification of malignant lymphoma, a new WHO classification was established founded on the 1994 REAL classification that was based on a variety of objective information such as the presence of various immune markers or the analysis of gene expression within each lymphoma, along with morphological and clinical findings from each case studied.6,7
Based on the histopathological analysis of the reported studies, the extranodal marginal zone B cell lymphoma of the mucosa-associated lymphoid tissue (MALT) is reported to account for 38-64% of ocular adnexal lymphomas.5,8,9 In contrast to lymphomas of other organs, ocular adnexal lymphomas are low malignancy MALT lymphomas in most cases and have a relatively benign structure of the lymphoid follicle.10
Treatment of extranodal marginal zone B cell lymphoma by surgical resection, radiation and chemotherapy is effective when compared with the efficacy of treating lymphomas from other cell types.1,4,9,10-13 However, recurrence and metastasis have been reported in several cases and prognosis is poor in cases with systemic metastasis.11,14,15 Hence, we assessed the clinical pattern, the histopathological findings, the response to various treatments, the recurrence pattern and the prognosis of patients with malignant lymphoma in the ocular adnexa.
This study comprised 22 total eyes from 17 patients who were diagnosed with ocular adnexal malignant lymphoma and treated at the Dong-A University Hospital from October 1999 to June 2004. We retrospectively analyzed the patients' medical records including the histological classification based on patient age and gender; the symptoms and signs present at the initial diagnosis; the findings from the surgical biopsies; the presence of binocular invasion; the clinical stages based on the presence of systemic invasion; the treatment methods used and the effectiveness of those treatments. The mean duration follow-up period was 24.8 months, with a range of 12 to 53 months.
A histological diagnosis was performed in all cases. To demonstrate the presence of monoclonal characteristics within the studied tumors, the expression of ╬║ and ╬╗ immunoglobulin light chains (using monoclonal antibodies diluted to 1:300 and 1:000 respectively, Dako Corporation) was assessed by flow cytometry. The biopsy specimens were fixed in 10% formalin and embedded in paraffin. Hematoxylin-eosin staining was then performed. Immunohistochemical testing was performed using the peroxidase-antiperoxiadase (PAP) technique with antibodies against IgG, IgM, CD3 (1:50, Dako Corporation, Santa Barbara, CA, USA), CD5 (1:100), CD10 (1:100), CD20 (1:100), CD23 (1:100), and CD45RO (1:50).
Each of the studied lymphomas was histopathologically reclassified according to the WHO classification published in 1997.6-7 The clinical staging was determined according to the Ann Arbor staging system.16 In the case of invasion to both eyes, the consensus on the disease stage has not yet been reached. In this study, however, bilateral orbital involvement without any other lesions outside the orbit was classified as stage I EE according to other investigator's criteria.17-19
The treatment modalities were determined according to the Ann Arbor criteria. In cases where lesions were limited to the orbit, radiation therapy of 3,000-4,000 cGy was primarily administered after surgical resection for a complete cure. For patients with monocular blindness or with small lymphocytic lymphoma (B cells), chemotherapy using the CHOP regimen (cyclophosphamide, vincristine, doxirubicin, and prednisone) was administered. In the cases with systemic invasion, radiation therapy and chemotherapy were administered simultaneously for symptomatic purposes.
The response after treatment was evaluated based on the Response Criteria of non-Hodgkin's lymphoma as recommended by the National Cancer Institute (NCI) in 1998. All patients were evaluated with a full physical examination, a biopsy of the suspected conjunctival lesion and periodical orbital CT. In cases with an absence of tumors in the lymph nodes and at the primary site as assessed by clinical examination, biopsy and CT analyses were deemed as complete remission (CR); the reduction of tumors in the primary site by over 75% was deemed as uncompleted remission (CRu); the reduction of tumors in the primary site by over 50% was deemed as partial remission (PR); and the detection of new lesions or an increase of the tumor size was deemed as relapse or progression.20
During patient follow-up, the complications during or after treatment were assessed by questioning the patients, by taking patient physicals and by performing slit-lamp examinations.
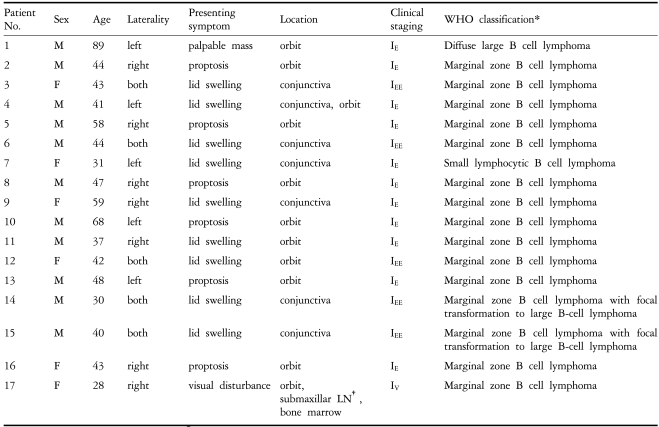
The age of patients ranged from 28 years to 89 years and the mean age was 46.8 years old. Six females and 11 males were included in the study. The major symptoms listed in the order of decreasing frequency were proptosis, lid swelling, a painless palpable mass and blurred vision (Table 1). Proptosis was detected in 8 patients with orbital tumors, and a painless palpable mass was noted in 5 of the patients. Seven patients with tumors in the conjunctiva complained of symptoms like keratoconjunctivitis. In a patient with decreased visual acuity, the tumor had invaded the vicinity of the optic nerve as visualized on the orbital CT.
The location of each lymphoma was limited to the conjunctiva in 10 eyes from 6 patients and limited to the orbit in 10 eyes from 9 patients. Lymphoma was simultaneously detected in the conjunctiva and in the orbit at the time of the diagnosis in one patient. The tumor was located in the orbit, the bone marrow and the submandibular gland in this patient. Except for one patient with the simultaneous invasion to the conjunctiva and the orbit, lymphomas were detected in both eyes in 4 of 6 patients with tumors in their conjunctiva. According to the Ann Arbor clinical stages at the time of diagnosis of 16 patients with ocular adnexa-limited lymphoma, 11 patients whose lesions were limited to the monocular adnexa displayed stage IE, and 5 patients that displayed invasion to the binocular adnexa were classified as stage IEE. One patient that displayed stage IV had metastasized to the bone marrow and the submandibular gland.
The histopathological classification was done according to the WHO classification. Twenty total eyes from 15 patients of extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT) were examined. In patients 14 and 15, who had mainly extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT), the focal transformation to large B cell lymphoma was detected. One patient (1 eye) was diagnosed with diffuse large B cell lymphoma that was positive for CD20 and CD45. Another patient (1 eye) with small lymphocytic B cell lymphoma was positive for IgM and CD20.
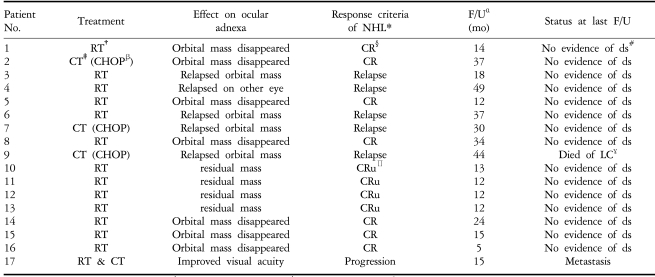
Of the 17 patients, 16 patients (totaling 21 eyes) with disease limited to the orbit were primarily treated by biopsy and partial resection followed by 20 cycles of radiation therapy (3,000-4,000 cGy) or chemotherapy (CHOP: cyclophosphamide+vincristine+doxorubicin+prednisone). According to the response criteria for non-Hodgkin's lymphoma recommended by the National Cancer Institute (NCI), 11 patients showed complete remission and 4 patients showed uncompleted remission. Although a patient with systemic metastasis was simultaneously treated by radiation and chemotherapy, he died 15 months after the treatment. In 4 patients with primary tumors in the orbit, residual tumors were detected by CT after the completion of radiation therapy. These residual tumors were reduced in size by over 75%. During the 12-13 month follow-up period, new tumors or metastasis were not detected. Thus, these cases were classified as uncompleted remissions (Table 2).
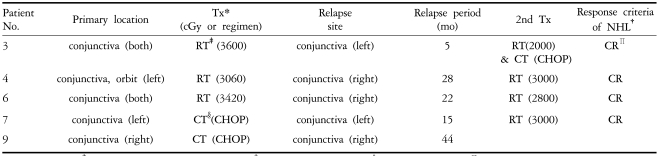
Tumors relapsed after treatment in 5 patients and the overall recurrence rate was 31.3%. The lymphomas relapsed in 2 of 3 patients who were treated with chemotherapy for their primary treatment. Relapse was detected in 2 of 5 patients with binocular invasion. Of the 7 patients with tumors in their conjunctiva, the recurrence rate was 71.4% and the tumor recurred in 5 patients during follow-up. Additional radiation therapy or chemotherapy was administered to patients with recurring tumors, except in one case where the patient died of liver cirrhosis 44 months after the relapse.
After the fifth month of radiation therapy, a tumor relapsed on left conjunctiva of patient number 3 who had tumors on both conjunctiva. It was treated completely with additional radiation (2,000 cGy) and chemotherapy (CHOP regimen). For patient number 4 who had a tumor in the monocular conjunctiva and in the orbit, the tumor relapsed in the opposite conjunctiva at the 28th month and regressed with additional radiation therapy (3,000 cGy). For patient number 6 with tumors in both conjunctiva, radiation therapy was given and the tumor recurred on the right conjunctiva at the 22nd month. It was then treated with radiation therapy (2,800 cGy) and remitted completely. Patient number 7, who had small lymphocytic lymphoma in the monocular conjunctiva, was treated with chemotherapy (CHOP regimen) as the primary treatment. The tumor relapsed at the 15th month and was treated with radiation therapy (3,000 cGy), which was followed by complete regression (Table 3).
A patient who had systemic invasion at the time of diagnosis, despite treatment with radiation therapy and chemotherapy, died 15 months after the treatment. However, the reduced exophthamos and improved visual acuity helped to improve his quality of life.
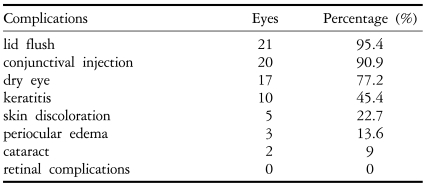
After radiation therapy, lid flushing and conjunctival injection were detected in most patients. Such complications were temporary and were relieved with the administration of steroid eye drops. Additional complications were dry eyes (77.2%), keratitis (45.4%), skin discoloration (22.7%), periocular edema (12%), and cataracts (9%), listed in the order of decreasing frequency. Retinal complications were not detected during follow-up (Table 4).
The incidence of malignant lymphoma in the ocular adnexa was previously reported as being approximately 10% of total orbital tumors.1,3,4 The incidence has recently been on the rise. In eastern Asia, the incidence of malignant lymphoma has been reported to be 18.4-28.0%.2,21,22
In regard to the ratio of males and females with the disease, the incidence of non-Hodgkin's lymphoma is known to be higher in males than in females.23,24 Similarly, lymphoma of the ocular adnexa has been shown to occur more frequently in males.11,14,19 In our study, 11 cases were in males and 6 cases in females, with a higher incidence in males.
The mean age of patients included in the study was 46.8 years, with ages ranging from 28 to 89 years. Two of 17 patients (11.7%) were under 30 years old and 5 patients were under 40 years (29.4%). Previous studies generally reported a higher age of incidence for MALT lymphoma in the range of 59-65 years.4,5,8,9,22 Although MALT lymphoma is typically a disease of the elderly, this study showed an incidence of MALT lymphoma in patients of a much younger age, which contrasts with the mean age of the patients with MALT lymphoma reported in the literature. Recent studies of Korean patients with lymphoma in the ocular adnexa have reported that the mean age of patients with MALT lymphoma was 44-48 years.25-28 Hence, in regard to MALT lymphoma of the ocular adnexa, this disease occurs at a younger age in Korea than in western countries or Japan.
The clinical characteristics of lymphoma of the ocular adnexa are diverse according to the location of tumors, and we observed multiple symptoms including conjunctival injection, lid swelling, proptosis, painless palpable mass, ptosis, foreign body sensation, and blurred vision. In 7 patients with lymphoma in the conjunctiva, lid swelling and conjunctival injection were detected. These patients were previously treated for conjunctivitis a long time prior to diagnosis. In 4 of 7 patients with lymphoma in the conjunctiva, including a patient whose lymphoma involved both the conjunctiva and orbit, lymphoma was detected in both eyes. Study guidelines required that both eyes be examined at the first examination and during the follow-up observation period. The cases misdiagnosed as having an atypical infection such as chlamydia have been reported because of continuous conjunctival injection and lid swelling.29,30 If the eye condition showed the symptoms of conjunctivitis and it did not improve in response to conventional treatments, a confirmation biopsy was considered necessary.
In the present study, extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT) constituted 88.2% of all lymphomas involving the ocular adnexa. This rate is much higher than the 50-79.5% reported in the previous studies of patients originating from Japan or western countries.3-5,9 Recently, Cho et al. and Lee et al. each reported incidences of 89.7% and 86%, respectively, of MALT-type ocular adnexal lymphoma in Koreans.27,28 These results may reveal the higher incidence of MALT lymphoma and the lower incidence of other types of lymphoma in Koreans.
The clinical staging was determined according to the Ann Arbor staging system.16 However, in the case of invasion to both eyes, the consensus on the disease stage has not yet been reached. Kim et al. and Stafford et al. classified multiple lesions in the same site of the diaphragm as stage II.11,17 However, because bilateral orbital lymphoma has subsequently been shown to be able to respond completely to treatment with only radiation therapy, thus giving it a prognosis identical to a unilateral tumor, it is classified as stage I.10,18,19 In a similar fashion, bilateral ocular adnexal lymphoma was classified as stage IEE in this study.
Lymphomas in the ocular adnexa respond well to radiation therapy or chemotherapy.10-14,18,19 According to studies reported up until presently, MALT lymphoma in the conjunctiva also responds well to radiation therapy or chemotherapy.1,11,14,19,31 During the analysis of tumor relapse in this study, lymphomas recurred during follow-up in 5 of 7 patients who had lymphoma in the conjunctiva, with a high recurrence rate of 71.4%. On the other hand, in the 9 patients with tumors limited to the orbit, relapse was not detected after treatments. Thus, the recurrence rate was significantly different from the cases in which the tumor invaded the conjunctiva. A number of environmental factors have been implicated in the occurrence of non-Hodgkin's lymphoma, including infectious agents, chemical exposure, and medical treatment.32 De Jong D et al. reported that the chronic inflammation or chronic irritation of antigens lead to a loss of the control of proliferation and differentiation in B lymphocytes.33 Chronic ocular irritations from infectious agents including viruses, environmental factors, eye drops or preservatives may induce MALT lymphoma. Byon et al. reported that lymphoma cells remained in the conjunctiva after therapy despite regular histological testing and treatment.34 These remaining cells may not have been detected due to the fact that previous reports simply reflected the clinical improvement without periodic conjunctival histopathologic examination. Conventional therapeutic modalities for malignant lymphoma occurring in the conjunctiva may need to be reconsidered. Even if specific conjunctival lesions like salmon patch are not detected, more careful observation including periodic histopathologic examination during follow-up is required.
After treatment of primary malignant lymphomas in the orbit, residual tumors were detected in 4 patients on CT. After treatment of patients with tumors in the chest from non-Hodgkin's lymphoma, residual tumors were detected in as often as 40% of patients during the follow-up CT.35 Determining complete remission in patients is a remaining problem. Surbone et al. have reported that only fibrosis was detected in 95% of cases when performing histological testing on the residual tumors after treatment for aggressive non-Hodgkin's lymphoma.35 In addition, the study of Coiffier et al. showed no difference resulted between CR and CRu groups in the recurrence rate, the disease-free survival rate, or in the total survival rate.36 Therefore, the cases without any change in the size of lesions for a proper period were reclassified as complete remission.
In this study, all of the 17 patients with ocular adnexa lymphoma responded well to conventional treatments. However, the risk of the relapse was high when it occurred in the conjunctiva or simultaneously invaded both eyes. And residual tumors may remain after treatment for the some patients with the lymphoma in the orbit. Hence, for the treatment of lymphoma, it is important to precisely diagnose the location of lesions, histopathological findings and the clinical stage. Long-term follow-up observation may also be necessary after treatment.
Notes
This study was conducted with the sponsorship of the Dong-A University Scientific Research Fund, 2004.
REFERENCES
1. Dunbar SF, Linggood RM, Doppke KP, et al. Conjunctival lymphoma: results and treatment with a single anterior election field. A lens sparing approach. Int J Radiant Oncol Biol Phys 1990;19:249-257.

2. The Hematolymphoreticular Study Group of the Korean Society of Pathologist. REAL classification of malignant lymphomas in the Republic of Korea: incidence of recently recognized entities and changes in clinicopathologic features. Cancer 1998;83:806-812.


3. Witherspoon AC, Diss TC, Pan L, et al. Primary low-grade B-cell lymphoma of the conjunctiva: a mucosa-associated lymphoid tissue type lymphoma. Histopathology 1996;28:129-134.


4. Shirai K, Okada Y, Saika S, Ohnishi Y. A case of mucosaassociated lymphoid tissue (MALT) lymphoma of presumed lacrimal gland origin. Ganka Rinsho Iho (Jpn Rev Clin Ophthalmol) 1996;90:604-606.
5. Coupland SE, Krause L, Delecuse HJ, et al. Lymphoproliferative lesions of the ocular adrexa: analysis of 112 cases. Ophthalmology 1998;105:1430-1441.


6. Harris NL, Jaffe ES, Diebold J, et al. The World Health Organization classification of neoplastic disease of the haematopoietic and lymphoid tissues: report of the Clinical Advisory Committee Meeting, Airlie house, Virginia, November 1997. Histopathology 2000;36:69-87.


7. Harris NL, Jaffe ES, Stein H, et al. A revised European-American classification of lymphoid neoplasm: a proposal from the international lymphoma study group. Blood 1994;84:1361-1392.


8. Ellis JH, Banks PM, Campbell RJ, Liesegang TJ. Lymphoid tumors of the ocular adnexa. Clinical correlation with the working formulation classification and immunoperoxidase staining of paraffin sections. Ophthalmology 1985;92:1311-1324.


9. White WL, Ferry JA, Harris NL, Grove AS Jr. Ocular adrexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology 1995;102:1994-2006.


10. Erkal HS, Serin M, Sak SD, Cakmak A. Radiation therapy for stage I primary orbital non-Hodgkin's lymphomas. Tumori 1997;83:822-825.


11. Stafford SL, Kozelsky TF, Garrity JA, et al. Orbital lymphoma: radiotherapy outcome and complications. Radiother Oncol 2001;59:139-144.


12. Pelloski CE, Wilder RB, Ha CS, et al. Clinical stage IEA-IIEA orbital lymphomas: outcomes in the era of modern staging and treatment. Radiother Oncol 2001;59:145-151.


13. Bolek TW, Moyses HM, Marcus RB Jr, et al. Radiotherapy in the management of orbital lymphoma. Int J Radiat Oncol Biol Phys 1999;44:31-36.


14. Ohtsuka K, Hashimoto M, Suzuki Y. A review of 244 orbital tumors in Japanese patients during a 21-year period: origins and locations. Jpn J Ophthalmol 2005;49:49-55.


15. Jenkins C, Rose GE, Bunce C, et al. Histological features of adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Br J Ophthalmol 2000;84:907-913.



16. Rosenberg SA, Boiron M, DeVita VT Jr, et al. Report of the Committee on Hodgkin's Disease Staging Procedure. Cancer Res 1971;31:1862-1863.

17. Kim YH, Fayos JV. Primary orbital lymphoma: a radiotherapeutic experience. Int J Radiat Oncol Biol Phys 1976;1:1099-1105.


18. Smitt MC, Donalldson SH. Radiotheraphy is successful treatment for orbital lymphoma. Int J Radiat Oncol Biol Phys 1995;31:929-934.


19. Esik O, Ikeda H, Mukai K, Kaneko A. A retrospective analysis of different modalities for treatment of primary orbital non-Hodgkin's lymphoma. Radiother Oncol 1996;38:13-18.


20. Cheson BD, Horning SJ, Coiffier B, et al. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored Working Group. J Clin Oncol 1999;17:1244


21. Nango K, Furumura T, Uyama M. Histopathological analysis of 53 cases of orbital tumors. Folia Ophthamol Jpn 1992;42:1271-1278.
22. Hiroshi T, Kazuhito T, Hidetoshi Y. Diagnosis and treatment of orbital malignant lymphoma: 14-year review at Yamagata university. Jpn J Ophthalmol 2001;45:305-312.


23. Medeiros LJ, Harris NL. Lymphoid infiltrates of the orbit and conjunctiva: a morphologic and immunophenotypic study of 99 cases. Am J Surg Pathol 1989;13:459-471.


24. Knowles DM, Jakobiec FA, McNally L, Bruke JS. Lymphoid hyperplasia and malignant lymphoma occurring in the ocular adnexa (orbit, conjunctiva, and eyelids): a prospective multiparametric analysis of 108 cases during 1977 to 1987. Hum Pathol 1990;21:959-973.


25. Jo YJ, Yim JH, Park KS. MALT (mucosa associated lymphoid tissue) type lymphoma of the ocular adnexa. J Korean Ophthalmol Soc 2002;43:357-362.
26. Kim SS, Ahn SD, Chang HS, et al. Primary orbital lymphoma: A retrospective analysis of result of radiation therapy. J Korean Soc Ther Radiol Oncol 2002;20:139-146.
27. Cho EY, Han JJ, Ree HJ, et al. Clinicopathologic Analysis of ocular adnexal lymphomas: Extranodal marginal zone B-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol 2003;73:87-96.


28. Lee JL, Kim MK, Lee KH, et al. Extranodal marginal zone B-cell lymphomas of mucosa-associated lymphoid tissuetype of the orbit and ocular adnexa. Ann Hematol 2005;84:13-18.


30. Hornblass A, Jakobiek FA, Reifler DM, Mines J. Orbital lymphoid tumor located predominantly within extraocular muscles. Ophthalmology 1987;94:688-697.


31. Galieni P, Polito E, Leccisotti A, et al. Localized orbital lymphoma. Haematologica 1997;82:436-439.

33. de Jong D, Aleman BMP, Taal BG, et al. Controversies and consensus in the diagnosis, work-up and treatment of gastric lymphoma: an international survey. Ann Oncol 1999;10:275-280.


34. Byon DS, Moon YS, Kim JS, Kwak HJ. Histological progress observation of conjunctival MALToma. J Korean Ophthalmol Soc 2002;43:443-448.
- TOOLS
-
METRICS

- Related articles
-
Mini-Review: Clinical Features and Management of Granular Corneal Dystrophy Type 22023 August;37(4)
Orbital Lymphangioma: Characteristics and Treatment Outcomes of 12 Cases2017 June;31(3)
The Pathologic Characteristics of Pingueculae on Autofluorescence Images2013 December;27(6)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



