Prevalence and Risk Factors for Cataracts in Persons with Type 2 Diabetes Mellitus
Article information
Abstract
Purpose
This study was performed to quantitatively evaluate the prevalence and risk factors of cataracts in Korean patients with type 2 diabetes mellitus.
Methods
Eight hundred fifty patients (males: 342, mean age: 58.07±8.60 years) with diabetes who underwent ophthalmologic evaluation were studied retrospectively. Diabetic patients were classified into a cataract group and control group (i.e. a group without cataracts). Risk factors like sex, age, duration of diabetes, fasting blood sugar, HbA1c, BUN, creatinine, and total cholesterol were compared between patients with and without cataracts.
Results
Four hundred twenty-five patients (50.00%) had cataracts at evaluation. Females were more common in the cataract group than the control group. The mean age did not differ between the two groups. Total cholesterol, triglyceride, and LDL cholesterol levels were not different between the two groups. Duration of diabetes was significantly longer in patients in the cataract group than in the control group (13.03±6.96 years vs. 7.03±6.04 years, p<0.001). The patients in the cataract group also had higher levels of HbA1c, BUN, creatinine, and fasting blood sugar than those in the control group. Multiple regression analysis revealed that the duration of diabetes (p<0.001) was significantly correlated with the presence of cataracts.
Conclusions
The duration of diabetes was the most significant risk factor for cataracts in patients with diabetes. This finding indicates that the accumulated effect of hyperglycemia is related to lens transparency in patients with diabetes.
Diabetes mellitus has been reported as the most critical factor causing visual loss. Among the various complications of diabetes mellitus in the eyes, diabetic retinopathy has been regarded as the most common cause of visual loss.1-3 Diabetes mellitus is also known as an important risk factor for cataracts. In epidemiologic studies published in European countries, factors such as a long duration of diabetic disease, advanced age at the time of clinical diagnosis, advanced retinopathy, treatment with diuretics, and poor control of blood sugar level are reported as risk factors for cataract in diabetics.4-11
However, reports about the prevalence and risk factors of cataract in diabetes are limited for Korean patients.12 Most diabetes mellitus cases in Korea are type 2, with a shorter duration than in European countries. The incidence and prevalence of type 1 diabetes mellitus and juvenile-onset diabetes mellitus is lower in Korea than that of European populations.13 Accordingly, it is expected that the incidence and risk factors for cataracts in diabetes mellitus are different. Furthermore, recent studies have reported that various complications such as cardiovascular, nephrologic, and ophthalmologic diseases could be prevented by controlling glucose in diabetic patients. Therefore, we conducted research on the frequency and risk factors of cataracts in Korean patients with diabetes.
From January 2004 to December 2005, 850 patients with type 2 diabetes mellitus of the Diabetes Center of Eulji Medical Center at Eulji Medical University were evaluated retrospectively. All patients underwent an ophthalmologic evaluation including slit lamp biomicroscopy and indirect ophthalmoscope fundus examination. Three hundred and forty-two patients (40.2%) were male and the mean age of all patients was 50.87±8.60 years.
A diabetic patient was defined as one who had a serum glucose concentration of more than 120 mg/dl while fasting more than twice or who had greater than 200 mg/dl when measured within two hours after a meal more than twice. The diabetic period was defined from the diagnosis of diabetes mellitus to the day of the indirect ophthalmoscope fundus examination. The fasting serum glucose concentration used in this analysis was the one examined closest to the day of the fundus examination. In addition, we investigated HbA1c, total cholesterol, triglyceride, HDL-cholesterol, LDL-cholesterol, BUN, and creatinine. Each patient underwent best-corrected distance visual acuity measurement with a Snellen chart. Visual acuity was defined as the average value of the corrected visual acuity of both eyes before examination. An ophthalmic examination was performed with slit lamp biomicroscopy and indirect ophthalmoscope fundus examination after the pupil was maximally dilated with 1.0% tropicamide (Mydriacyl) and 2.5% phenylephrine hydrochloride (Neosynephrine).
Diabetic patients were classified into a cataract group and a control group without cataracts. We compared clinical data and ophthalmologic results between the cataract group and the control group. Risk factors for cataracts, including sex, age, the diabetic period, blood sugar in fasting, HbA1c, and presence of diabetic retinopathy, were evaluated.
To analyze how the risk factors affected the occurrence of cataracts, chi-square analysis was used. To compare the difference of biochemical examination between the two groups, Student's t-test was used. Multiple regression analysis was performed to investigate the relationship between various variables and the degree of lens opacity. A p-value<0.05 was considered significant.
Results
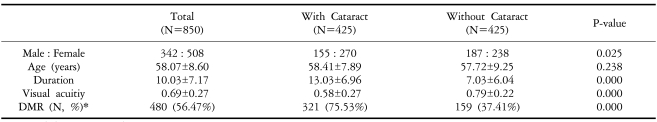
The clinical characteristics of the patients are shown in Table 1. From a total of 850 diabetic patients, 425 patients (50.0%) had cataracts. The mean patient age was 58.07±8.60 years old, the mean diabetic period was 10.03±7.17 years, and the mean visual acuity was 0.69±0.27.
Gender differed significantly between the cataract group and the controls (p=0.025). There were more females in the cataract group than the control group [370 (63.5%) vs. 238 (56.0%); p=0.025]. The mean age in each group was not statistically different. The diabetic period was significantly longer in the cataract group than in the controls (13.03±6.96 years vs. 7.03±6.04 years, p<0.001). The mean visual acuity was significantly worse in the cataract group than in the control group (0.58±0.27 vs. 0.79±0.22, p<0.001). More diabetic retinopathies were observed in the cataract group (321, 75.53%) than in the control group (159, 37.41%, p<0.001).
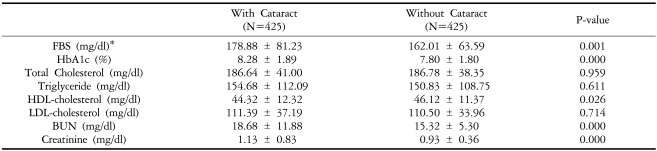
Biochemical analyses of the two groups are shown in Table 2. Total cholesterol, triglyceride and LDL cholesterol were not different between the two groups. The level of blood sugar after fasting was higher in the cataract group than in the control group (178.88±81.23 mg/dl vs. 162.01±63.59 mg/dl; p=0.001). The level of HbA1c was higher in the cataract group than in the control group (8.28±1.89% vs. 7.80±1.80%; p<0.001). The level of HDL-cholesterol was lower in the cataract group than the control group (44.32±12.32 mg/dl vs. 46.12±11.37 mg/dl; p=0.026). The level of BUN was higher in the cataract group than the control group (18.68±11.88 mg/dl vs. 15.32±5.30 mg/dl; p<0.001). The level of creatinine was higher in the cataract group than the control group (1.13±0.83 mg/dl vs. 0.93±0.36 mg/dl; p<0.001).
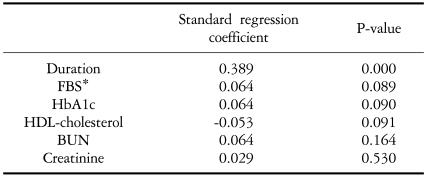
As illustrated in Tables 2 and 3, risk factors, such as the diabetic period, fasting blood sugar, HbA1c, HDL-cholesterol, BUN, and creatinine, were different between the two groups. In multiple regression analysis (Table 3), the diabetic period (p<0.001) was the significant factor associated with cataracts in patients with diabetes mellitus.
Discussion
Kini, et al14 reported that senile cataracts caused visual loss in 22% of the general population. In Korea, cataracts were also reported as a main cause of the visual loss by 29.7% to 31.2% of the general population.15,16 Persons with diabetes have been found to be at increased risk of visual impairment compared to non-diabetic persons.17,18
Since the study on the cataracts of diabetic patients in 1798 by John Rollo, much research on cataracts has been reported. Cataracts occur at a younger age in diabetics than non-diabetics. The incidence of cataracts increases proportionally with the degree and the period of the diabetes mellitus.4-11 It is reported that most patients having lenticular opacity had diabetes mellitus for more than five years, and that various types of opacities of the lens were developed in 64% of diabetic patients under treatment.19 Caird et al20 reported that 10.7% of patients of senile cataract extraction had diabetes mellitus and that the cataract extraction rate in those cases was four to six times higher than the cases without diabetes mellitus. In these results, the cataract incidence rate is higher in diabetes mellitus patients. In this study, the mean duration of diabetes mellitus in patients with cataracts was 13.03±6.96 years.
Patterson reported that there was lenticular opacity when the blood sugar was more than 225 mg%.21 The fasting blood sugar level was higher in the cataract group than in the control group (178.88±81.23 mg/dl vs. 162.01±63.59 mg/dl; p=0.001). However, in multiple regression tests, the level of blood sugar was not the significant factor associated with cataract for diabetes mellitus patients in this study. Previous studies reported that a direct relationship between glycated hemoglobin and cataracts was not found in the prevalence data; however, cataracts were associated with the duration of diabetes. It may be that the additional five-year duration was necessary to observe the effect of glycemia.8,9,22 In this study, the level of HbA1c was higher in the cataract group than in the control group; however, in multiple regression tests it, too, was not a significant factor for cataract incidence with diabetes mellitus.
When considering the higher prevalence of diabetes mellitus in females than males, it follows that the incidence of diabetic cataracts would be higher in females.5,19 The prevalence of diabetic cataracts was higher in women in this study. In terms of the relationship between cataracts and visual acuity, the worse the visual acuity deteriorated, the higher the incidence rate of cataract appeared. This is reasonable because cataracts are the cause of visual loss.
Previous studies reported that the retinopathy was an influential factor on the degree of cataract.8,9 In diabetic patients, according to Kirby,19 diabetic retinopathy was found in 40% of those without cataracts and 53% of those with cataracts. Our analysis shows that diabetic retinopathy appeared 37.41% of those without cataracts and 75.53% of those with cataracts. Thus, it is predicted that many patients will have diabetic retinopathy when their cataracts have progressed. Moreover, since the frequency of patients with diabetic retinopathy was highest in the cataract group, we can say that the degree of impairment of internal organs due to diabetes mellitus is related to cataracts.
In multiple regression analysis, we found that the duration of diabetes was the most important risk factor for diabetic cataracts, and the roles of fasting blood sugar level and HbA1c as risk factors were ambiguous. Because we used the fasting sugar level and other data that were checked on the day of the ophthalmic examination, these do not reflect the average values during the patients' diabetic periods. So, except for the duration of diabetes, we could not find the exact relationship between the risk factors associated with diabetes and cataract incidence.
In conclusion, the duration of diabetes mellitus was the significant risk factor for cataracts. This study suggests that lenticular opacity incurred by a long duration of hyperglycemia is related to the incidence of cataracts, and that it would be possible to prevent the disease by controlling hyperglycemia.