 |
 |
| Korean J Ophthalmol > Volume 38(1); 2024 > Article |
|
Abstract
Purpose
To compare topical and peribulbar anesthesia in cataract surgery for hemodynamic changes, rate of complications and pain score in patients with cardiovascular disease.
Methods
A prospective comparative study at a tertiary care center in India. Patients >40 years old with treated/controlled hypertension and cardiovascular disease scheduled for cataract surgery under topical or peribulbar anesthesia were recruited. Heart rate, blood pressure, and ophthalmic and systemic complications were noted: preoperatively, immediately after block, intraoperatively, immediately postoperatively and 1 hour postoperatively. A visual analog scale was used to assess the pain score.
Results
A total of 150 patients (75 in each group) underwent cataract surgery. There was a significant rise in pulse rate and blood pressure after peribulbar injection and intraoperatively, which gradually reduced to baseline 1 hour after surgery in both groups (p < 0.001), with systolic blood pressure intraoperatively being significantly greater in the peribulbar group (155.49 ┬▒18.14 mmHg vs. 147.95 ┬▒17.71 mmHg, p = 0.01). The topical group had slightly lower visual analog scale scores (1.12 ┬▒ 0.99) than the peribulbar group (1.44 ┬▒ 0.90, p = 0.04).
Conclusions
Cataract surgery appears safe in patients with adequately controlled cardiovascular disease, and topical anesthesia may be preferable due to noninvasiveness, adequate analgesia, and minimal effect on hemodynamic parameters. Therefore, hemodynamically stable patients of cardiovascular disease undergoing uncomplicated cataract surgery may be counselled for topical anesthesia.
Cataract is the leading cause of blindness in the world, being particularly common in low-income countries. Since most of these patients are elderly, they often suffer from concomitant cardiovascular disease. Systemic hypertension affects one billion individuals worldwide and is endemic in the elderly population [1,2]. Previous studies have shown an increased incidence of hemodynamic instability, myocardial ischemia, and cardiac arrhythmias in patients with severe hypertension (systolic blood pressure [SBP], >180 mmHg; diastolic blood pressure [DBP], >110 mmHg). Still, there is little evidence of perioperative complications with blood pressure (BP) <180/110 mmHg [3].
Patients undergoing cataract surgery are susceptible to ischemic heart disease due to risk factors like hypertension, old age, atherosclerosis, and diabetes [4]. While topical anesthesia is the current norm for cataract surgery, patients who cannot cooperate with it require regional anesthesia. This includes patients with multiple systemic comorbidities, particularly cardiovascular disease, which increase in prevalence with age. Regional anesthesia most commonly used for cataract extraction carries a low to moderate risk of hemodynamic instability in these patients [5]. We aimed to compare peribulbar injection with topical anesthesia for preinjection/postinjection (peribulbar group), preoperative (topical anesthesia), intraoperative, and postoperative changes in hemodynamic parameters/complications and pain score in a tertiary care hospital in India.
The study was approved by the Institutional Ethics Committee of Indira Gandhi Government General Hospital and Post Graduate Institute (No. GHIEC/2016). Informed consent was obtained from the participants after an explanation of the nature and possible consequences of the study. The study followed the tenets of the Declaration of Helsinki.
This hospital-based prospective comparative clinical study was conducted at Indira Gandhi Government General Hospital and Post Graduate Institute Hospital (Puducherry, India), a tertiary care hospital in South India. The study was conducted on 150 patients >40 years of age, scheduled for cataract surgery (phacoemulsification/manual small incision cataract surgery) with concomitant controlled cardiovascular disease receiving treatment from the internal medicine or cardiology departments after physician approval and informed consent. Antiplatelet medications were discontinued for 5 days before surgery in patients who were taking them. Exclusion criteria were the following: patients allergic to lignocaine 2%, bupivacaine 0.5%, or proparacaine 0.5%; patients with severe hypertension (SBP >180 mmHg, DBP >110 mmHg); hemodynamically unstable patients; and patients with complicated cataract, traumatic cataract, uveitic cataract, pseudoexfoliation, and lens-induced glaucoma.
Patients were recruited into two groups (peribulbar injection or topical) based on their willingness for topical anesthesia, each group comprising 75 patients: group A, topical proparacaine 0.5% with or without lignocaine 2% gel; and group B, peribulbar bupivacaine 0.5%, lignocaine 2%, and hyaluronidase. Patients in group A received four doses (approximately 40 ╬╝L per dose) of unpreserved proparacaine 0.5% drops that were instilled on the ocular surface (two doses on the cornea, and one each in the superior and inferior conjunctival cul-de-sac) 10 minutes before surgery. Five minutes before surgery, two further doses were instilled in the cornea. If necessary, lignocaine 2% gel was also used. Patients in group B received a 5 mL mixture of lignocaine 2%, bupivacaine 0.5%, and hyaluronidase that was injected into the peribulbar area at the junction of the outer one-third and inner two-thirds of the inferior orbital rim 10 minutes before surgery with a 1-inch 26-gauge needle, with an additional 2 to 4 mL injected at the junction of inner one-third and outer two-thirds of the superior orbital rim, if necessary.
All patients received monitored anesthesia care throughout the surgery. In the topical anesthesia group, pulse rate and BP were recorded preoperatively in the waiting area, intraoperatively, immediately after surgery and 1 hour after surgery in the ward. In the peribulbar group, pulse rate and BP were recorded before giving a peribulbar anesthetic injection in the waiting area, after the injection, intraoperatively, immediately, and 1 hour after surgery. Preoperative and postoperative electrocardiograms (ECG) were taken. None of the patients required sedation.
Any intraoperative complications during the surgery were recorded. Patients were given a postoperative questionnaire to assess their comfort levels during surgery. Total surgical time was noted from the start of the incision to the closure of the wound. For the pain score, a visual analog scale (VAS) questionnaire (on a scale of 0-10, with 0 indicating no pain and 10 indicating unbearable pain) was administered to the patient 1 hour after the surgery for overall pain scoring.
A power analysis using the G*Power (Heinrich Heine University D├╝sseldorf) indicated that a total sample of 140 would be needed (70 in each group) to detect medium effects (d = 0.30) with 90% power using a t-test between means with ╬▒ at 0.05 [6].
The collected data were analyzed using descriptive and inferential statistics. The independent samples t-test was used to evaluate the statistical significance of change between the two groups of each measured variable. Repeated measures analysis of variance (RM-ANOVA) was used to test the significant difference in changes over time within the group. Chi-square was used for measuring the differences between categorical variables. A p-value of less than 0.05 was considered statistically significant. All statistical analysis was done using statistical software, IBM SPSS ver. 19.0 (IBM Corp).
The study was conducted on 150 patients aged 40 years and above with underlying cardiovascular disease requiring cataract surgery. Patients undergoing cataract surgery under topical anesthesia were significantly younger (58.91 ┬▒ 8.17 years) than those under peribulbar anesthesia (64.83 ┬▒ 8.15 years, p < 0.001). Patients in both groups had a comparable number of comorbidities ( p = 0.352). In the peribulbar group, a greater number of patients, 10 patients, were suffering from coronary artery disease as compared to the four patients in the topical anesthesia group (Table 1). In the peribulbar group, 65 patients had immature senile cataracts and 10 presented with mature senile cataracts, whereas these numbers were 74 and 1, respectively, for the topical anesthesia group (p = 0.004). All patients underwent uneventful phacoemulsification with posterior chamber intraocular lens implantation, with full visual recovery.
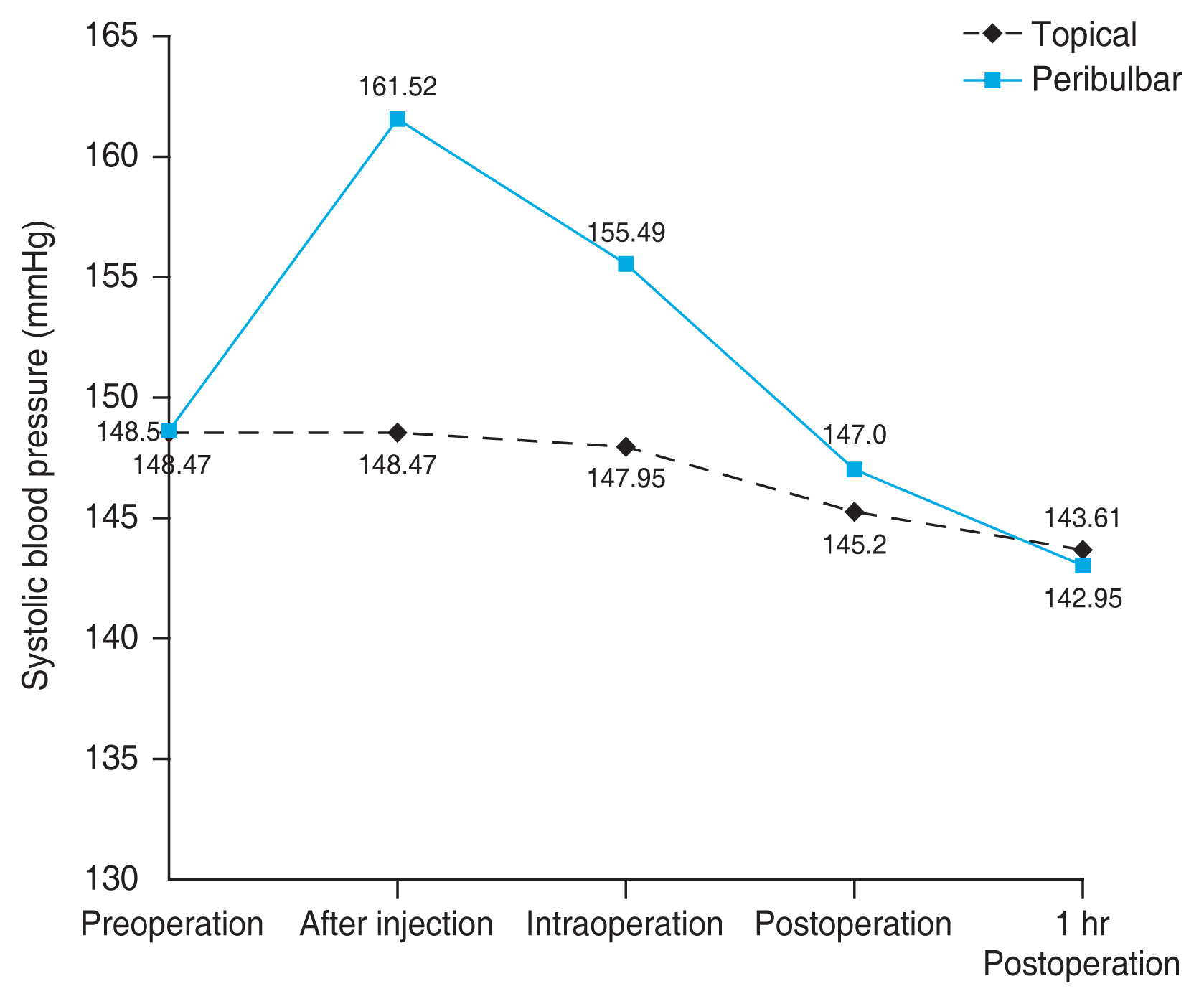
There was a significant rise in pulse rate and BP after peribulbar injection and intraoperatively, which gradually reduced to baseline one hour after surgery in both groups (p < 0.001), with SBP intraoperatively being significantly higher in the peribulbar group (155.49 ┬▒ 18.14 mmHg vs. 147.95 ┬▒ 17.71 mmHg, p = 0.01) (Fig. 1). The quantum of change was maximum following the peribulbar injection, especially in the SBP (Table 2). We did not find any new ECG changes before, during, or after surgery in any patient.
Total surgical time was comparable between both groups (topical group, 11.80 ┬▒ 1.50 minutes; peribulbar group, 11.87 ┬▒ 1.70 minutes; p = 0.80). No systemic and ophthalmic complications were noted in any patient. There was a significant difference in VAS scores between the topical (1.12 ┬▒ 0.99) and peribulbar patients (1.44 ┬▒ 0.90, p = 0.04), indicating greater patient satisfaction with topical than peribulbar anesthesia. There was no statistically significant difference between the two groups for reported discomfort.
This prospective comparative clinical study shows the effect of topical and peribulbar anesthesia on hemodynamic and ECG changes. In addition, complication rates (systemic and ophthalmic), patient discomfort and total surgical time were also noted. In our study, patients undergoing cataract surgery under topical anesthesia (58.91 ┬▒ 8.17 years) were significantly younger than those under the peribulbar block (64.83 ┬▒ 8.15 years). Younger patients who are more alert and cooperative likely chose topical anesthesia.
We found the rise in pulse rate greatest after peribulbar injection with a gradual return to baseline in the postoperative period, with no significant difference between the two groups, similar to earlier reports [5,7]. We also observed a significant difference in intraoperative SBP changes, higher in the peribulbar group. The SBP peaked after peribulbar injection, but no adverse events were noted. The DBP was not significantly different between the two groups, though a slight increase was seen after peribulbar injection. Glantz et al. [4] reported a few minutes of transient hypertension when the block was performed. A significantly higher SBP after regional anesthesia compared with topical and subtenon injection was also noted by Ryu et al. [7]. Yap et al. [8] found a significant rise in SBP intraoperatively, in the preassessment and anesthetic room. Fichman [9] reported that only 1% of patients had raised BP when topical anesthesia alone was used in cataract surgery. Hence, it appears that topical anesthesia has a lower propensity to affect hemodynamic changes due to its noninvasiveness.
Agarwal et al. [10] reported a significant increase in hypertensives who developed isolated systolic hypertension in the holding area while studying the effect of perioperative BP on intraoperative complications during phacoemulsification surgery under local anesthesia. Basta et al. [11] prospectively studied systemic adverse events during phacoemulsification under monitored anesthesia care and observed that arterial hypertension and agitation were the most frequent. We, too, noted a sudden rise in BP in a few patients in the holding area, and deferred surgery for these patients (as per standard hospital protocol), pending further physician evaluation. Only those patients whose cardiovascular status was subsequently controlled to meet our criteria were operated upon later and included in the study. This extra care may be one of the reasons for zero cardiovascular adverse events in our study, similar to previous reports [12,13]. All participants were receiving appropriate therapy for all other disorders as well.
The total surgical time was similar between the two groups. Expert surgeons performed all the surgeries, and we did not observe any complications during cataract surgery. We observed that patients who underwent cataract surgery under topical anesthesia perceived slightly less pain than patients who underwent cataract surgery under a peribulbar block. A similar finding was reported by Coelho et al. [14] when they performed phacoemulsification without sedation using topical and peribulbar anesthesia. Zehetmayer et al. [15] also evaluated the efficacy of topical anesthesia as an alternative to peribulbar anesthesia in cataract surgery. They observed that subjective pain was comparable whether topical or peribulbar anesthesia was used. They reported good patient cooperation (motility control) in topical anesthesia and no significant differences in complications. The slightly favorable results in the topical anesthesia group in our study may be due to the younger age of patients who chose topical anesthesia over a regional block. Younger, alert patients are more likely to cooperate with the surgery requirements. Comparable VAS scores prove that topical anesthesia can effectively control pain during cataract surgery by phacoemulsification similar to a peribulbar block.
We did not randomize the patients between topical and peribulbar anesthesia as patient co-operation and choice are the inherent requirements for topical surgery. While this is an important limitation of the current study, the findings suggest similar results between the two choices of anesthesia management for a short procedure in stable cardiovascular patients by expert surgeons.
It is observed that owing to improvements in technology and expertise most ocular surgeries are increasingly performed topically. However, there are many situations where peribulbar anesthesia is required, even in candidates for topical surgery. Our study emphasizes the need for rigorous monitoring of cardiovascular status preoperatively, with deferring of surgery in case of sudden-onset hypertension, to minimize the risk of adverse events. Also, in the presence of adequate preoperative cardiovascular control and consenting patients, topical anesthesia for cataract surgery by phacoemulsification may be the optimum choice in patients with concomitant cardiovascular disease.
References
1. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52.


3. Howell SJ, Sear JW, Foex P. Hypertension, hypertensive heart disease and perioperative cardiac risk. Br J Anaesth 2004;92:570-83.


4. Glantz L, Drenger B, Gozal Y. Perioperative myocardial ischemia in cataract surgery patients: general versus local anesthesia. Anesth Analg 2000;91:1415-9.


5. Haddadi S, Marzban S, Fazeli B, et al. Comparing the effect of topical anesthesia and retrobulbar block with intravenous sedation on hemodynamic changes and satisfaction in patients undergoing cataract surgery (phaco method). Anesth Pain Med 2015;5:e24780.



6. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91.



7. Ryu JH, Kim M, Bahk JH, et al. A comparison of retrobulbar block, sub-Tenon block, and topical anesthesia during cataract surgery. Eur J Ophthalmol 2009;19:240-6.



8. Yap YC, Woo WW, Kathirgamanathan T, et al. Variation of blood pressure during topical phacoemulsification. Eye (Lond) 2009;23:416-20.



9. Fichman RA. Use of topical anesthesia alone in cataract surgery. J Cataract Refract Surg 1996;22:612-4.


10. Agarwal PK, Mathew M, Virdi M. Is there an effect of perioperative blood pressure on intraoperative complications during phacoemulsification surgery under local anaesthesia? Eye (Lond) 2010;24:1186-92.



11. Basta B, Gioia L, Gemma M, et al. Systemic adverse events during 2005 phacoemulsifications under monitored anesthesia care: a prospective evaluation. Minerva Anestesiol 2011;77:877-83.

12. Katz J, Feldman MA, Bass EB, et al. Injectable versus topical anesthesia for cataract surgery: patient perceptions of pain and side effects. Ophthalmology 2000;107:2054-60.


13. Rocha G, Turner C. Safety of cataract surgery under topical anesthesia with oral sedation without anesthetic monitoring. Can J Ophthalmol 2007;42:288-94.


Fig.┬Ā1
Comparison of changes in systolic blood pressure from preoperative period to 1-hour postoperative period in topical and peribulbar groups.
Table┬Ā1
Comparison of the demographic data between the topical and peribulbar anesthesia groups (n = 150)
| Characteristic | Topical group (n = 75) | Peribulbar group (n = 75) | p-value |
|---|---|---|---|
| Age (yr) | 58.91 ┬▒ 8.17 | 64.83 ┬▒ 8.15 | <0.001* |
| Sex | 0.734 | ||
| ŌĆāMale | 26 | 28 | |
| ŌĆāFemale | 49 | 47 | |
| Comorbidity | 0.352 | ||
| ŌĆāHypertension | 75 | 75 | |
| ŌĆāCoronary artery disease | 4 | 10 | |
| ŌĆāDiabetes mellitus | 26 | 31 | |
| ŌĆāOther | 1 | 3 |
Table┬Ā2
Comparison of vitals (pulse rate and blood pressure) between topical and peribulbar anesthesia groups
| Variable | Preoperation | After injection | Intraoperation | Immediate postoperation | 1-hr Postoperation | p-value |
|---|---|---|---|---|---|---|
| Pulse rate (beats/min) | ||||||
| ŌĆāTopical group | 83.28 ┬▒ 10.93 | - | 83.57 ┬▒ 9.71 | 81.77 ┬▒ 9.78 | 81.37 ┬▒ 10.56 | 0.004* |
| ŌĆāPeribulbar group | 83.15 ┬▒ 12.26 | 89.28 ┬▒ 13.44 | 85.04 ┬▒ 11.06 | 81.57 ┬▒ 10.12 | 80.11 ┬▒ 9.41 | <0.001* |
| ŌĆāp-value | 0.94 | - | 0.39 | 0.90 | 0.44 | |
| Systolic blood pressure (mmHg) | ||||||
| ŌĆāTopical group | 148.47 ┬▒ 18.67 | - | 147.95 ┬▒ 17.71 | 145.20 ┬▒ 19.42 | 143.61 ┬▒ 19.53 | <0.001* |
| ŌĆāPeribulbar group | 148.59 ┬▒ 17.68 | 161.52 ┬▒ 19.11 | 155.49 ┬▒ 18.14 | 147.00 ┬▒ 15.76 | 142.95 ┬▒ 13.67 | <0.001* |
| ŌĆāp-value | 0.97 | - | 0.01* | 0.53 | 0.81 | |
| Diastolic blood pressure (mmHg) | ||||||
| ŌĆāTopical group | 84.88 ┬▒ 9.29 | - | 85.97 ┬▒ 9.63 | 84.72 ┬▒ 9.81 | 82.91 ┬▒ 9.54 | <0.001* |
| ŌĆāPeribulbar group | 84.47 ┬▒ 10.72 | 91.07 ┬▒ 11.32 | 87.29 ┬▒ 10.02 | 85.28 ┬▒ 9.65 | 83.01 ┬▒ 9.16 | <0.001* |
| ŌĆāp-value | 0.80 | - | 0.41 | 0.73 | 0.94 | |



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




