Comparison of Stab Incision and Eyelid Crease Incision Techniques in Children with Revision Frontalis Sling Surgeries Using Silicone Rods
Article information
Abstract
Purpose
To compare stab and eyelid crease incision techniques in revision frontalis sling surgeries using silicone rods.
Methods
This retrospective study involved 52 eyes in 48 consecutive pediatric patients who underwent revision frontalis sling surgery between 2008 and 2019. All primary surgeries were performed by making eyelid crease incisions and suturing of silicone rods onto the tarsal plates. The revision surgeries were performed by either making stab incisions over the eyelid through which to pass the silicone rods (group A), or by refixing the same or a new silicone rod to the tarsal plate (group B). The surgical results were compared.
Results
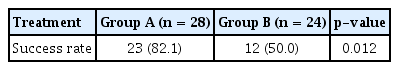
The mean follow-up period was 22.4 months (range, 6–62 months) and the mean age of the patients was 6.1 years (range, 1–16 years). There were 28 female and 20 male patients. Surgical success was achieved in 23 of 28 patients (82.1%) in group A, and 12 of 24 patients (50.0%) in group B. The difference between the groups was statistically significant (p = 0.012). Superficial punctate epithelial defects were detected in six group A patients (21.4%) and seven group B patients (29.1%). In group B, lid hematoma occurred in three patients (12.5%) and entropion occurred in three patients (12.5%). The silicone rods were removed from two eyes, and entropion spontaneously resolved in one eye with close follow-up.
Conclusions
Using the stab incision technique increases revision frontalis sling surgery success rates when primary surgeries are performed using eyelid crease incisions and suturing silicone rods to the tarsal plates in children.
The frontalis sling is a surgical procedure performed to correct congenital ptosis in cases with low levator function [1]. Ptosis recurrence is a common problem after surgery [2]. Recurrence rates are reportedly between 0% and 100% and increase with longer follow-up periods, regardless of the sling materials or surgical techniques used [3–6]. In cases with a failed initial sling procedure, the outcomes of frontalis suspension surgery as a revision surgical option have not been extensively reported in the literature. We used both the stab incision and tarsal fixation techniques in this study’s revision surgeries. We reported our revision results and compared both techniques in revision surgeries in pediatric patients.
Materials and Methods
Ethics statement
The Institutional Review Board of the Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa approved the study (No. E-83045809-604.01.01-569673). Informed consent was obtained from all parents before the initiation of any procedure. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki
Study design
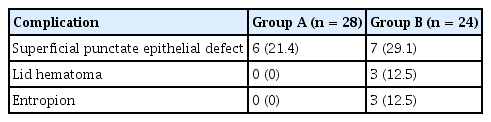
This retrospective study enrolled 52 eyes of 48 consecutive patients who underwent revision frontalis sling surgery between 2008 and 2019. Sex, age, surgery type, postoperative results, and patient complications were recorded. The mean patient follow-up period was 22.4 months (range, 6–62 months), and the mean patient age was 6.1 years (range, 1–16 years). Of the patients, 28 were male and 20 were female. All primary surgeries were performed by making an eyelid crease incision and suturing a silicone rod (Beaver-Visitec International Inc) to the tarsal plate. The revision surgeries were performed either by making stab incisions over the eyelid through which to pass the silicone rod (group A) (Fig. 1A–1F), or by refixing the same or a new silicon rod to the tarsal plate (group B) (Fig. 2A–2F), as in the primary surgery. A single-loop design technique was used in all cases. In both groups, three stab incisions were made in the same place as the old ones. Two incisions were embedded in the eyebrow in line with the medial and lateral canthi, and one incision was made between the previous incisions, 1 cm above the eyebrow. The silicone rods in group A were removed through the stab incisions, and two additional incisions were made 3 mm above the eyelashes, in line with the limbus. The silicone rod was passed through the stab incisions using a wright needle in a pentagonal fashion. For group B, an eyelid crease incision was made, and the anterior face of the tarsal plate was opened without traumatizing the present silicone rod. An initial attempt was made to find and resuture the extant silicone rod to the tarsal plate. If the rods could not be sutured or the ptosis could not be corrected, the original silicone rod was removed, and a new one was sutured to the superior third of the tarsus using a nonabsorbable suture and then passed through the upper stab incisions. In both groups, the ends of the silicone rods were tied after achieving the desired eyelid elevation, and the knots were buried in a pocket under the frontalis muscle. The eyelid crease and stab incisions were sutured. A successful outcome was achieved if the postoperative eyelid position was maintained within 1 mm of the normal eyelid position in unilateral cases, and the upper lid margin to central corneal reflex maintained a distance of at least 3 mm in bilateral cases.

Illustration of the stab incision technique drawn by the authors. (A) Preoperative photograph. (B) Externalization of the silicone rod knot from the center of the previous suprabrow incision localization and trying to elevate the eyelid by pulling the silicone rod ends. (C) Silicone tube was removed by cutting one of its loops after a failed attempt to achieve the desired eyelid elevation. (D) Silicone rod passes through the stab incisions. (E) Desired eyelid elevation was obtained by pulling the silicone rod ends. (F) Knots are buried under the frontalis muscle in a pocket and then sutured.
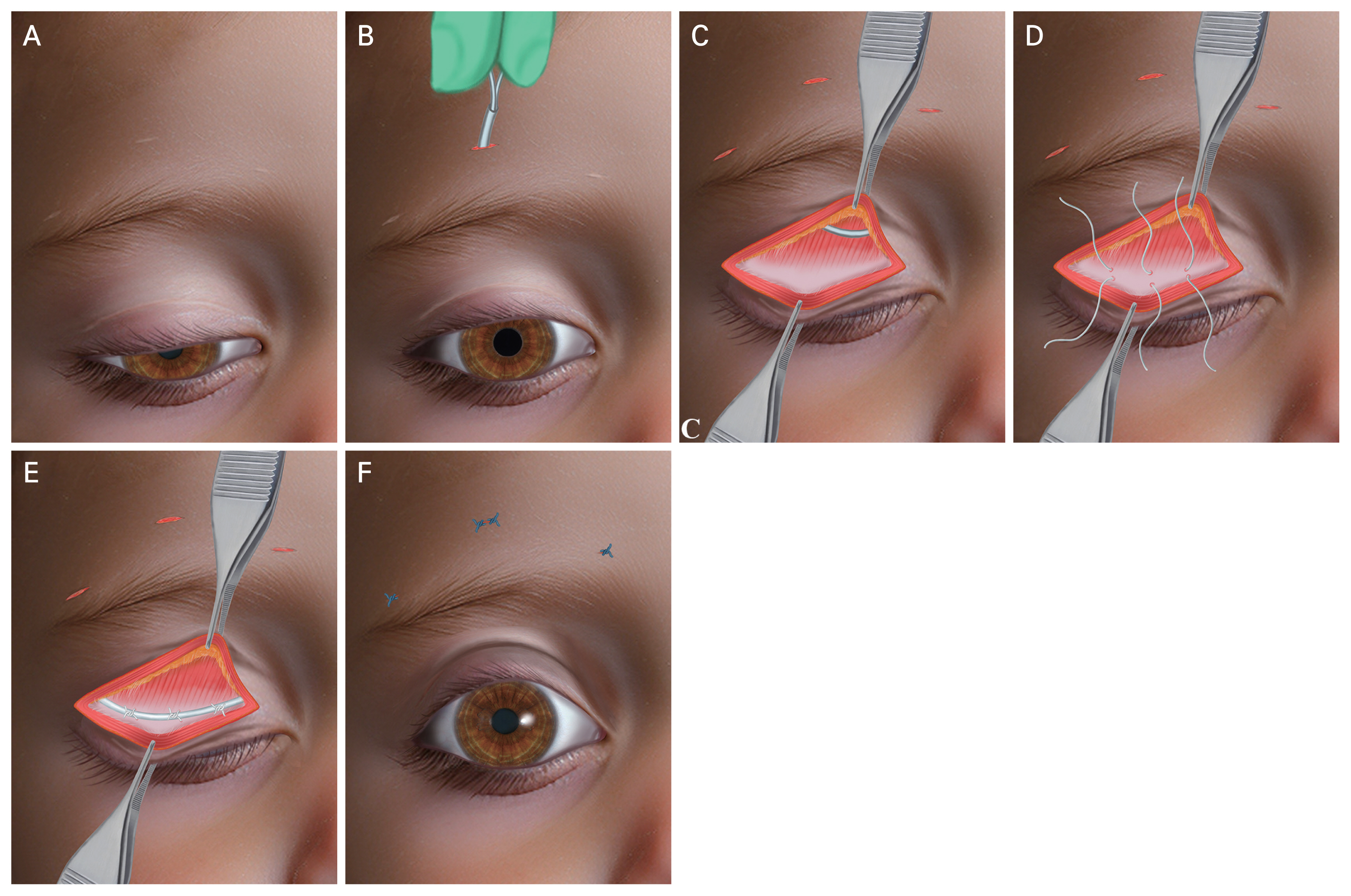
Illustration of the tarsal fixation technique drawn by the authors. (A) Preoperative photograph. (B) Externalization of silicone rod knot. (C) Slipping of silicone rods through the upper tissues. (D) Silicone rod was removed after failing to achieve the desired eyelid elevation by resuturing the same silicone rod to the tarsal plate. (E) Suturing of a new silicone rod to the superior one-third of the tarsus using a nonabsorbable suture. (F) Burial of the knots under the frontalis muscle after achieving the desired eyelid elevation.
Statsitical analysis
Patients who were followed up for less than 6 months were excluded from the study. The chi-square test was used to analyze the categorized data. A p-value of less than 0.05 was considered statistically significant.
Results
The results of the study show that in group A, adequate lid elevation and good lid contour could not be achieved by untying the knot, pulling the end of the rods, and retying them more tightly in group A. In group B, the silicone rods slipped through the upper tissues and deep septum in 22 patients, and two patients had broken silicone rods. In eight patients, the original silicone rod was resutured to the tarsal plate; new silicone rods were used in 16 patients. Surgical success was achieved in 23 of 28 group A patients (82.1%), and 12 of 24 group B patients (50.0%). The difference was statistically significant in both groups (Table 1). Superficial punctate epithelial defects were detected in six group A patients (21.4%) and seven group B patients (29.1%). Lid hematoma occurred in three group B patients (12.5%). Entropion was the main complication, and it occurred in three group B eyes (12.5%) (Table 2). The silicone rods were removed in two eyes, and entropion resolved spontaneously in one eye, with close follow-up.
Discussion
Blepharoptosis, a condition characterized by drooping of the upper eyelid, is associated with certain cosmetic and functional deficits. Blepharoptosis has conventionally been treated by assessing preoperative levator function, with a frontalis sling operation being the surgical choice for patients with poor levator function [7,8]. Different suspension materials have been used for frontalis sling surgery. These include the fascia lata (autogenous or preserved), Gore-Tex strips (W. L. Gore & Associates Inc), nonabsorbable sutures, and silicone rods [9,10]. Different sling designs (single loop and double pentagon) can be used. Stab incisions can be made over the eyelid to pass the suspension material through, or the suspension material can be sutured to the tarsus via an eyelid crease incision. The best approach to frontalis sling surgery remains controversial. Frontalis suspension surgery with different sling materials may result in similar cosmetic and functional results [3]. Tillett and Tillett [11] described the use of silicone as a suspensory material. Silicone rods have some advantages over the other options, as they can be easily loosened, tightened, or removed. The elasticity of the silicone rod may be ideal for patients with a minimal Bell phenomenon, because they can close their eyes more effectively with an elastic suspensory material [2].
In our facility, we routinely use silicone rods in frontalis sling operations. However, ptosis recurrence is a major problem after these procedures. In a study by Carter et al. [12], only 7% of the patients required revision or replacement of the sling. On the higher end, Ben Simon et al. [3] reported a recurrence rate of 44%, Kersten et al. [13] reported a need for reoperation in 22% of patients, Leone and Rylander [14] reported reoperation in 32% of patients, and Leone et al. [15] reported reoperation in three of 20 eyelids (15%). In a previous study, Buttanri et al. [2] had a 50% success rate with the stab incision technique and one of 83.9% with the lid crease incision technique in a mean follow-up of 16.3 months in cases of primary frontalis sling surgery. This particular study demonstrated the benefit of fixation in decreasing recurrence after primary operations. However, the effect of fixation on the silicone rod in revision surgeries has yet to be studied. Generally, the reasons for recurrence after frontalis suspension surgery are not well understood. In our study, the main reason for recurrence was the slippage of the silicone rod. The cheesewiring effect of the rod may be the reason for this sliding. While fixation of the rod may prevent sliding, it can induce scar formation on the tarsal plate around the silicone rod. On the contrary, a skin crease incision may weaken the attachment of the orbicularis to the tarsal plate and disrupt the anatomy of the lid.
In this study, we compared the stab incision technique used for group A with the lid crease incision and fixation techniques used for group B in revision surgeries. The stab incision technique was more successful (p = 0.012). After the first operation, some fibrosis occurred on the anterior surface of the tarsus and on the lid. When we performed a stab incision, the resulting fibrosis may have kept the silicone rod tight. However, when the anterior surface of the tarsus was reopened, and the silicone rod was refixated, these fibrotic areas could be disrupted and cut, thus facilitating the reslipping of the silicone rod. In these patients, since the fixation had been performed in the first operation, the tarsus could be structurally damaged, and the sutures could cut the tarsus more easily. According to our results, lid crease incision and fixation of the silicone rod may be more effective in primary surgeries; however, in revision surgeries, the stab incision technique may be a better approach.
In both groups, loosening of silicone rod knots was not observed. In group A, adequate lid elevation could not be obtained by pulling the ends of the rods after untying them. In group B, in all the patients, except for two (silicone rods were broken), the silicone rods slipped through the upper tissues. Therefore, to increase the success rate, the main aim may be to prevent sliding of the silicone rod and to induce scar formation on the tarsal plate around it.
In the stab incision technique, the skin may hang on the tarsus, and as a result, the lid crease may not be formed. One reason we make a lid incision is that we want to create a lid crease. Since we created a lid crease in the first operation in these patients, there was no advantage to performing an incision again. In all surgical branches, revision surgeries are much more difficult and are always prone to bleeding [7]. In these patients, the formation of a lid crease incision and suturing of the silicone rod could have been hemorrhagic and traumatic. Specifically, lid hematoma occurred in three patients (12.5%) in group B. Fixation may be much more difficult in hemorrhagic lids, and accordingly, the stab incision technique is generally less traumatic.
The main complication was entropion, which occurred in three eyes in group B. In two eyes, we had to remove the silicone rods, and in one eye, entropion was resolved spontaneously with close follow-up. Direct traction application to the tarsus by the silicone rod may result in deterioration of the lid stability. In our study, we may have passed the sutures very close to the upper edge of the tarsus in the fibrotic lids. Fibrosis of the lid after the first operation can cause this complication. In contrast, in the stap incision technique, there was no direct traction to the tarsus and no entropion.
Serious corneal complications can occur and lead to blindness after frontalis sling operations [16]. Eyelids may not be closed after the operation especially at nights. Superficial punctate epithelial defects were detected in six patients (21.4%) in group A and in seven patients (29.1%) in group B. In group B, three of these patients had entropion. As a result, artificial teardrops and gels were prescribed. All patients, except for two patients with entropion, recovered within 1 month without any sequelae. Chronic corneal problems, infections and ulcers did not occur in any patients. In a related study using silicone rods, Fogagnolo et al. [17] reported corneal staining in five of 22 patients, and all of these patients improved, except for one, who required removal of the silicone rods due to corneal ulcers. The corneal complication rates due to lagophthalmus were approximately the same in the primary and revision surgeries in our studies.
The limitations of this study are the relatively small sample size, and the retrospective study design.
The stab incision technique seems to be more successful than the lid crease incision technique in revision frontalis sling surgeries in pediatric patients. This may also be true for other sling materials. Further studies comparing these revision techniques should be conducted.
Acknowledgements
None.
Notes
Conflicts of Interest
None.
Funding
None.