 |
 |
| Korean J Ophthalmol > Volume 37(6); 2023 > Article |
|
Abstract
Methods
A retrospective, clinic-based study was conducted on DED patients undergoing dry eye treatment. Patients were followed up at least twice, and symptoms and signs were evaluated using the Symptoms Assessment Questionnaire in Dry Eye (SANDE) score, tear secretion, tear film breakup time (TBUT), ocular staining score, and tear osmolarity. Mean humidity and temperature values for 1 week before ocular examinations were used as the environmental exposure level. The relationship between humidity and temperature, with DED clinical parameters was analyzed in single- and multi-environmental factor models.
Results
The study included 33 patients with a mean age of 53.9 ± 12.2 years. The low humidity group showed significantly higher SANDE scores (p = 0.023) and tear osmolarity (p = 0.008), and the low temperature group had higher SANDE scores (p = 0.004), ocular staining scores (p = 0.036), and tear osmolarity (p < 0.001). In the linear mixed model, single factor analysis showed that an increase in humidity resulted in decreased SANDE scores (p = 0.043), and an increase in temperature led to a decrease in SANDE score (p = 0.007), ocular staining score (p = 0.007), and tear osmolarity (p = 0.012). In the multifactor analysis, changes in humidity had no significant effect on dry eye parameters, but an increase in temperature was significantly correlated with decreased SANDE score (p = 0.026), ocular staining score (p = 0.024), and tear osmolarity (p = 0.002).
Dry eye disease (DED) is a common ocular surface disorder estimated to affect around 8.0% to 30.3% of the Korean population [1,2]. It is a multifactorial disease characterized by an unstable tear film, in which tear hyperosmolarity, ocular surface inflammation, and neurosensory abnormalities play etiological roles [3]. Subsequent symptoms of fluctuating visual acuity and ocular discomfort affect patients’ quality of life and pose a major public health issue.
Common risk factors of DED include older age, female sex, Asian race, and meibomian gland dysfunction [3]. Other than personal risk factors, environmental factors such as humidity and temperature are also known to be associated with dry eye prevalence, symptoms, and signs [4,5]. Specifically, low humidity has repeatedly been shown to be associated with higher dry eye prevalence [6-9]. In controlled experimental settings, lower relative humidity was reported to result in faster tear evaporation, shorter tear film breakup time (TBUT), and more ocular surface staining [10-13]. Moreover, the usage of moisture goggles was reported to ameliorate dry eye symptoms and reduce tear evaporation rate [14]. However, in real-world conditions and outside of laboratory settings, the effect humidity has on individual dry eye parameters has not yet been extensively studied. In addition, the role of temperature, one of the most important environmental factors, in dry eye is inconclusive. Some researchers suggested that higher ambient temperature was associated with more dry eye diagnosis [6,8,9], while others reported lower temperature correlated with better [15] or worse dry eye symptoms [16]. In experimental settings higher ambient temperature led to increased tear evaporation [17], but its effect on TBUT was conflicting [17,18]. Room temperature is known to be positively associated with ocular surface temperature [19] and ocular surface temperature is reported to be lower in evaporative dry eye [20]; however, the causal relationship is unclear, and the effect of environmental outside temperature on dry eye is yet to be investigated.
Domestic data regarding the influence of temperature and humidity on DED is limited. Often, clinicians tend to underestimate the impact of environmental factors, as DED treatment primarily focuses on routine artificial tears and other therapeutics. Highlighting the significance of the environment’s effects on the ocular surface, the recent TFOS Lifestyle Report [5] underscores the importance of considering these factors with patient treatment. To address this gap and gain a deeper understanding, we conducted a follow-up study on the same patients to assess how changes in humidity and temperature affect DED. This investigation involved analyzing climate data from the Korea Meteorological Administration along with clinical data obtained from a university hospital, to study the effects of real-world temperature and humidity on DED clinical parameters. Furthermore, we sought to identify which specific clinical parameters are more sensitive to these fluctuations.
This retrospective study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GBIRB2023-173). The requirement for informed consent was waived due to the retrospective nature of the study.
The study included dry eye patients who visited the clinic from February 2019 to August 2021. To avoid confounding due to geographical factors, only patients living in Incheon Metropolitan City, Korea, who did not move during the study period were included in the study. Dry eye diagnosis was based on the guidelines of the Korean Corneal Diseases Study Group [21]. Dry eye was diagnosed when the patient had dry eye symptoms and showed at least one objective dry eye sign. Dry eye symptoms included ocular symptoms such as dryness, discomfort, foreign body sensation, or pain, and visual symptoms such as blurring or vision fluctuation. Objective signs included TBUT ≤10 seconds or positive ocular surface staining of Oxford grade ≥1. All patients used the 0.05% cyclosporine twice daily and artificial tears were used as needed. Patients with contact lens wear, usage of glaucoma eyedrops, or those with other ocular surface diseases or systemic rheumatic diseases that could affect the ocular surface were excluded from the study.
All patients underwent clinical examination by an experienced cornea specialist (DHK) to assess dry eye symptoms and signs at least twice during follow-up. Dry eye symptoms were assessed using the Symptom Assessment Questionnaire in Dry Eye (SANDE) score [22]. Tear secretion was evaluated using the Schirmer test without anesthesia, and TBUT was measured as the time between the last eye blink and the time of tear breakup upon fluorescein instillation. Ocular staining score (OSS) was recorded using the Oxford grading scale [23], and tear osmolarity was measured with TearLab (TearLab Corp) according to the manufacturer’s manual.
Humidity and temperature data of Incheon Metropolitan City were collected from the Ministry of Environment of Korea on dates from February 2019 to August 2021. Data were acquired from the monitoring station closest to the subjects’ addresses. The mean values of temperature and relative humidity for 1 week before the ocular examinations were used as the environmental exposure level because environmental factors during the week preceding the examination had the most significant impact on dry eye signs and symptoms in a previous study [24].
For each patient, the dry eye parameters at the lowest humidity value were assigned to the low humidity group, while those at the highest humidity value were assigned for the high humidity group. The same logic was followed for the low and high temperature groups. To evaluate the differences in dry eye parameters between the low and high humidity or temperature groups, a paired t-test was conducted. Additionally, the effects of temperature or humidity changes on dry eye parameters were examined using a linear mixed model. This analysis was performed for both single- and multi-environmental factor models. In the single factor model, the effects of temperature and humidity were evaluated independently, while the multifactor model adjusted the temperature and humidity simultaneously to account for their potential interaction. Differences between sex were additionally analyzed. All data are presented as mean ± standard deviation, and all statistical analyses were performed using IBM SPSS ver. 20.0 (IBM Corp). A p-value of less than 0.05 was considered statistically significant.
Data from 33 patients were collected in the study. The mean age was 53.9 ± 12.2 years, and 24 patients (72.7%) were female. The mean follow-up period was 15.0 ± 3.2 months and the number of follow-ups was 2.2 ± 0.4. Mean SANDE score was 65.8 ± 27.1, mean TBUT was 4.0 ± 1.4 seconds, mean OSS was 1.0 ± 0.7, mean tear secretion was 10.5 ± 7.0 mm, and mean tear osmolarity was 303.9 ± 20.6 mOsm/L. Mean relative humidity was 67.9% ± 11.0%, and mean temperature was 14.7 ± 9.8 °C. Details of baseline demographics are presented in Table 1. Fig. 1 illustrates the relationship between relative humidity and temperature. There was a significant positive correlation between humidity and temperature (r = 0.528, p = 0.002).
Tables 2 and 3 illustrates the dry eye parameter differences between the lowest and highest humidity or the lowest and highest temperature. The mean relative humidity was 59.0% ± 7.2% in the low humidity group and 72.9% ± 8.1% in the high humidity group. SANDE score (p = 0.023) and tear osmolarity (p = 0.008) were significantly higher in the low humidity group. There were no significant differences in TBUT, OSS, and tear secretion between the low and high humidity groups. In terms of temperature, the mean temperature was 6.0 ± 7.3 °C in the low temperature group and 18.4 ± 7.3 °C in the high temperature group. SANDE score (p = 0.004), OSS (p = 0.036), and tear osmolarity (p < 0.001) were significantly higher in the low temperature group. TBUT and tear secretion were not significantly different among the two temperature groups.
In the linear mixed model using single environmental factor analysis, 1% increase in relative humidity led to a significant decrease in SANDE score (p = 0.043) and other parameters showed no significant association (Table 4). A 1 °C increase in temperature led to a significant decrease in SANDE score (p = 0.007), OSS (p = 0.007), and tear osmolarity (p = 0.012). In a multi-environmental factor analysis considering both humidity and temperature together, humidity change did not significantly affect dry eye parameters. As for temperature, 1 °C increase in temperature was associated with a significant decrease in SANDE score (p = 0.026), OSS (p = 0.024), and tear osmolarity (p = 0.002). Of the five DED parameters, tear osmolarity was the most sensitive to changes in temperature and humidity (Tables 2-4).
Differences between sex were also analyzed using the multi-environmental analysis model (Table 5). For both men and women, relative humidity change was not significantly associated with changes in dry eye parameters. Men exhibited a significant decrease in SANDE score (p = 0.015), ocular staining (p = 0.009), and tear osmolarity (p = 0.007) along with temperature increase, whereas women only experienced changes in SANDE score (p = 0.025) and tear osmolarity (p = 0.036) according to temperature change.
This study showed that increase in temperature was associated with alleviation of dry eye symptoms, less ocular surface staining, and lower tear osmolarity. While lower relative humidity was associated with worse symptom scores in the single factor analysis, other objective clinical parameters were not significantly affected, and the association became insignificant when using the multi-environmental model. Moreover, symptoms score and tear osmolarity were found to be consistently affected by changes in temperature regardless of analysis model or sex, and tear osmolarity was the most sensitive clinical parameter to be affected by the climate factors.
The relative lack of association between relative humidity and dry eye parameters was unexpected, considering the generalized idea from previous research that lower humidity aggravates dry eye. In experimental settings where asymptomatic patients were exposed to low relative humidity of 5% for 2 hours, ocular surface staining significantly increased and TBUT significantly decreased compared to before the exposure [11]. When Sjögren syndrome-associated dry eye patients were exposed to this condition, tear osmolarity and surface staining significantly increased [25]. In another experiment of asymptomatic patients who were exposed to shorter 1 hour exposure to 5% relative humidity, tear evaporation increased and TBUT significantly decreased [12]. Many more experiments with similar results exposed patients to desiccating stress under controlled environmental conditions, and relative humidity of desiccating stress ranged from 5% to 25% [13,26,27]. In our study the mean relative humidity was 67.9% ± 11.0%, and the minimum value was 40%, which is often the value used as the normal control condition [10,12]. It is possible that above a certain value of relative humidity, clinical parameters might not be significantly affected, which could be the reason for lack of correlation in our results. Moreover, since patients were on dry eye treatment, they may have been less affected by changes in humidity. However, in the linear mixed model of single environmental factor analysis decreased humidity was associated with worse SANDE scores, indicating patient symptoms may be affected, unlike objective parameters. That subjective symptoms worsen with lower humidity is consistent with aforementioned previous studies [6,7].
That higher temperature is associated with better clinical parameters are in line with some previous research [16,17]. A Taiwanese study [16] reported that in low ambient temperature was associated with higher ocular surface disease index (OSDI) score, similar to our study in which SANDE scores were higher with lower temperature. In an experiment using a controlled environmental chamber in which only temperature varied [17], mean TBUT increased significantly from 7.3 seconds at 5 °C to 12.4 seconds at 25 °C, and lipid layer thickness was also significantly higher at higher temperatures. While this study did not investigate ocular surface staining and our results did not reveal a significant correlation of temperature with TBUT, it can be inferred that lower temperature has a negative effect on the tear film, which might be related to the worse staining scores with lower temperature in our results. The effects of lower ocular surface temperature due to lower environmental temperature might have affected the pathophysiology of the ocular surface. When the ocular surface and eyelid temperature is below 33 °C meibum in glands was found to be thicker, impeding its normal delivery to the ocular surface [28], and ambient temperature below 10 °C was reported to result in ocular surface temperature of less than 32 °C [17]. Therefore, it is possible that in our study lower environmental temperature might have negatively affected the tear film dynamics, leading to worse symptoms and more staining.
To date, we could not find any studies on the effects of temperature on tear osmolarity. Our results showed that tear osmolarity was not only significantly higher with lower temperature, but it is also the most sensitive marker of DED to climate change. Tear osmolarity is an established diagnostic marker of DED, and increase in tear osmolarity reflects an increase in DED severity [29]. Other clinical parameters sometimes have poor correlation with subjective symptoms, which may be due to the multiple etiologies of DED and the specificity of each clinical test to one certain etiology [30]. In previous research comparing the objective clinical parameters of dry eye, tear osmolarity was found to be a superior predictor of dry eye severity [29,31]. In one study of 130 subjects [29], tear osmolarity had stronger statistical correlation with DED severity compared to TBUT and tear clearance. In another multicenter study of 314 subjects [31], tear osmolarity had superior diagnostic performance compared to TBUT, ocular surface staining, Schirmer test, and meibomian gland grading, with the highest area under the receiver operating characteristic curve. In our study, SANDE score and tear osmolarity were found to be consistently affected by temperature change regardless of analysis model or sex, suggesting that changes in tear osmolarity may be a precursor for DED symptoms. We believe that tear osmolarity may hold promise as a potential biomarker for DED in climate change.
Interestingly, the effects of temperature on DED parameters varied between men and women. While increased temperature correlated with decreased SANDE scores, OSS, and tear osmolarity in men, for women only SANDE scores and tear osmolarity were affected. It is known that due to sex steroids and other hormones, prevalence of DED is higher in women [32]. In previous studies investigating sex differences in DED symptoms and signs, women had higher OSDI scores, and less correlation between signs and symptoms [33,34]. In one study [35] women were more likely to show corneal staining compared to men, and in other studies [33,34] women had higher tear osmolarity, lower TBUT, along with higher staining scores. However, little is known about whether there are sex differences in the effects of temperature on the ocular surface. Since women did not exhibit changes in OSS along with temperature change, there may be differences in the way the ocular surface is affected between the men and women, in a mechanism that needs further investigation.
There are several limitations to our study. First, the relatively small sample size of DED patients (n = 33) may restrict generalization of the results to a larger population. Second, the relatively small number of follow-ups limited our ability to observe long term trends longitudinally within the same patient. Future studies should include a larger cohort with longer follow-up, and an additional cross-sectional approach would also be needed to assess DED parameters uniformly under consistent temperature and humidity levels across subjects. Additionally, while this study included patients undergoing the same topical treatment of twice daily 0.05% cyclosporine eyedrops, variable patient usage of artificial tears as needed could have impacted patient symptoms and ocular surface erosion status in subjects. Moreover, subjects may be more affected by indoor temperature or humidity than outside environmental exposure depending on their occupation and time spent outdoors. While this study was meant to investigate the influence of environmental humidity and temperature, in future investigations, we will incorporate such factors and if possible, adjust for indoor parameters for more detailed analysis. Furthermore, we only focused on humidity and temperature in this report; however, there are other meteorological (wind and sun exposure) and pollution-related environmental factors that could also play significant roles in DED, and taking these factors into account in future investigations would offer a more comprehensive understanding of the multifaceted influence of the environment on DED [5,24,36-38]. While these limitations underscore the need for further research, our results provide insights into the effect real-world temperature and humidity have on individual clinical DED parameters, emphasizing the significance of considering environmental factors in patients with dry eye disease.
In conclusion, this study showed that lower temperature is associated with worse dry eye symptoms and more ocular surface staining, along with higher tear osmolarity values. Tear osmolarity may be a sensitive indicator of DED to temperature change. Further research is needed to explore the potential impact of other environmental hazards such as air pollutants (ozone, nitrogen dioxide, and particulate matter), as they may be associated with DED [7,24,36].
References
1. Han SB, Hyon JY, Woo SJ, et al. Prevalence of dry eye disease in an elderly Korean population. Arch Ophthalmol 2011;129:633-8.


2. Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol 2014;158:1205-14.


3. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf 2017;15:276-83.


4. Mandell JT, Idarraga M, Kumar N, et al. Impact of air pollution and weather on dry eye. J Clin Med 2020;9:3740.



5. Alves M, Asbell P, Dogru M, et al. TFOS Lifestyle Report: impact of environmental conditions on the ocular surface. Ocul Surf 2023;29:1-52.


6. Um SB, Kim NH, Lee HK, et al. Spatial epidemiology of dry eye disease: findings from South Korea. Int J Health Geogr 2014;13:31.




7. Hwang SH, Choi YH, Paik HJ, et al. Potential importance of ozone in the association between outdoor air pollution and dry eye disease in South Korea. JAMA Ophthalmol 2016;134:503-10.


8. Chung CJ, Hsia NY, Wu CD, et al. Exposure to ambient NO2 increases the risk of dry eye syndrome in females: an 11-year population-based study. Int J Environ Res Public Health 2021;18:6860.



9. Zhong JY, Lee YC, Hsieh CJ, et al. Association between dry eye disease, air pollution and weather changes in Taiwan. Int J Environ Res Public Health 2018;15:2269.



10. McCulley JP, Aronowicz JD, Uchiyama E, et al. Correlations in a change in aqueous tear evaporation with a change in relative humidity and the impact. Am J Ophthalmol 2006;141:758-60.


11. Lopez-Miguel A, Teson M, Martin-Montanez V, et al. Dry eye exacerbation in patients exposed to desiccating stress under controlled environmental conditions. Am J Ophthalmol 2014;157:788-98.


12. Abusharha AA, Pearce EI. The effect of low humidity on the human tear film. Cornea 2013;32:429-34.


13. Teson M, Gonzalez-Garcia MJ, Lopez-Miguel A, et al. Influence of a controlled environment simulating an in-flight airplane cabin on dry eye disease. Invest Ophthalmol Vis Sci 2013;54:2093-9.


14. Ogawa M, Dogru M, Toriyama N, et al. Evaluation of the effect of moist chamber spectacles in patients with dry eye exposed to adverse environment conditions. Eye Contact Lens 2018;44:379-83.


15. Mendell MJ, Fisk WJ, Petersen MR, et al. Indoor particles and symptoms among office workers: results from a double-blind cross-over study. Epidemiology 2002;13:296-304.


16. Ho WT, Chiu CY, Chang SW. Low ambient temperature correlates with the severity of dry eye symptoms. Taiwan J Ophthalmol 2021;12:191-7.



17. Abusharha AA, Pearce EI, Fagehi R. Effect of ambient temperature on the human tear film. Eye Contact Lens 2016;42:308-12.


18. Maruyama K, Yokoi N, Takamata A, et al. Effect of environmental conditions on tear dynamics in soft contact lens wearers. Invest Ophthalmol Vis Sci 2004;45:2563-8.


20. Versura P, Giannaccare G, Fresina M, et al. Subjective discomfort symptoms are related to low corneal temperature in patients with evaporative dry eye. Cornea 2015;34:1079-85.


21. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol 2014;28:197-206.



22. Schaumberg DA, Gulati A, Mathers WD, et al. Development and validation of a short global dry eye symptom index. Ocul Surf 2007;5:50-7.


23. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003;22:640-50.


24. Kim Y, Choi YH, Kim MK, et al. Different adverse effects of air pollutants on dry eye disease: Ozone, PM2.5, and PM10. Environ Pollut 2020;265(Pt B):115039..


25. Lopez-Miguel A, Teson M, Martin-Montanez V, et al. Clinical and molecular inflammatory response in Sjögren syndrome-associated dry eye patients under desiccating stress. Am J Ophthalmol 2016;161:133-41.


26. Madden LC, Tomlinson A, Simmons PA. Effect of humidity variations in a controlled environment chamber on tear evaporation after dry eye therapy. Eye Contact Lens 2013;39:169-74.


27. Alex A, Edwards A, Hays JD, et al. Factors predicting the ocular surface response to desiccating environmental stress. Invest Ophthalmol Vis Sci 2013;54:3325-32.



28. Butovich IA, Arciniega JC, Wojtowicz JC. Meibomian lipid films and the impact of temperature. Invest Ophthalmol Vis Sci 2010;51:5508-18.



29. Versura P, Profazio V, Campos EC. Performance of tear osmolarity compared to previous diagnostic tests for dry eye diseases. Curr Eye Res 2010;35:553-64.


30. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol 2014;92:161-6.



31. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol 2011;151:792-8.


32. Sullivan DA, Rocha EM, Aragona P, et al. TFOS DEWS II sex, gender, and hormones report. Ocul Surf 2017;15:284-333.


33. Vehof J, Sillevis Smitt-Kamminga N, Nibourg SA, et al. Sex differences in clinical characteristics of dry eye disease. Ocul Surf 2018;16:242-8.


34. Borrelli M, Frings A, Geerling G, et al. Gender-specific differences in signs and symptoms of dry eye disease. Curr Eye Res 2021;46:294-301.


35. Lienert JP, Tarko L, Uchino M, et al. Long-term natural history of dry eye disease from the patient’s perspective. Ophthalmology 2016;123:425-33.



36. Kim Y, Paik HJ, Kim MK, et al. Short-term effects of ground-level ozone in patients with dry eye disease: a prospective clinical study. Cornea 2019;38:1483-8.


Fig. 1
Relationship between relative humidity and temperature. There was a significant positive correlation between relative humidity and temperature (r = 0.528, p = 0.002).
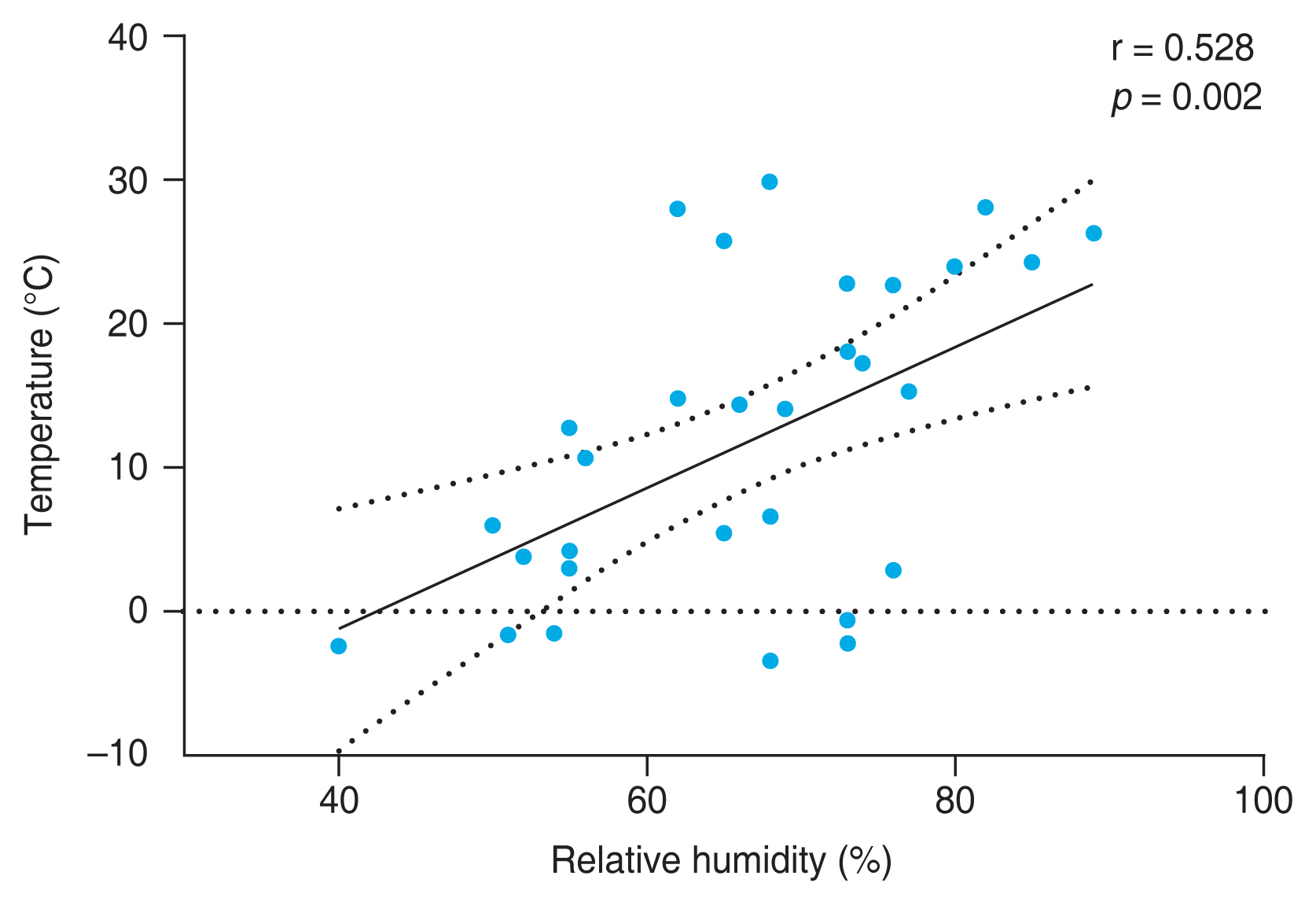
Table 1
Baseline characteristics of patients (n = 33)
Table 2
Comparison of dry eye disease parameters according to humidity (n = 33)
| Parameter | Low humidity | High humidity | p-value* |
|---|---|---|---|
| Humidity (%) | 59.0 ± 7.2 | 72.9 ± 8.1 | <0.001† |
| SANDE score | 68.7 ± 25.6 | 58.2 ± 24.4 | 0.023† |
| Tear film breakup time (sec) | 4.2 ± 1.1 | 4.4 ± 1.3 | 0.325 |
| Ocular staining score | 1.2 ± 0.6 | 0.9 ± 0.7 | 0.064 |
| Tear secretion (mm) | 9.7 ± 6.7 | 10.7 ± 7.0 | 0.166 |
| Tear osmolarity (mOsm/L) | 303.0 ± 10.9 | 296.0 ± 11.1 | 0.008† |
Table 3
Comparison of dry eye disease parameters according to temperature (n = 33)
| Parameter | Low temperature | High temperature | p-value* |
|---|---|---|---|
| Temperature (°C) | 6.0 ± 7.3 | 18.4 ± 7.3 | <0.001† |
| SANDE score | 72.7 ± 20.4 | 61.1 ± 25.4 | 0.004† |
| Tear film breakup time (sec) | 4.2 ± 1.1 | 4.3 ± 1.4 | 0.392 |
| Ocular staining score | 1.2 ± 0.6 | 0.9 ± 0.6 | 0.036† |
| Tear secretion (mm) | 9.8 ± 6.2 | 11.3 ± 7.4 | 0.076 |
| Tear osmolarity (mOsm/L) | 304.0 ± 11.9 | 294.9 ± 8.2 | <0.001† |
Table 4
Effects of environmental factors on dry eye disease using single- and multi-environmental factor analyses (n = 33)
| Factor | SANDE score | Tear secretion (mm) | Tear film breakup time (sec) | Ocular staining score | Tear osmolarity (mOsm/L) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Single factor analysis | ||||||||||
| Humidity change (per 1% increase) | −0.431 (−0.847 to −0.014) | 0.043* | −0.099 (−0.215 to 0.017) | 0.094 | −0.013 (−0.036 to 0.010) | 0.270 | −0.009 (−0.021 to 0.003) | 0.131 | −0.039 (−0.247 to 0.169) | 0.713 |
| Temperature change (per 1 °C increase) | −0.617 (−1.063 to −0.170) | 0.007* | −0.001 (−0.129 to 0.126) | 0.986 | −0.007 (−0.034 to 0.019) | 0.590 | −0.018 (−0.031 to −0.005) | 0.007* | −0.285 (−0.507 to 0.063) | 0.012* |
| Multifactor analysis | ||||||||||
| Humidity change (per 1% increase) | −0.396 (−0.808 to 0.016) | 0.060 | −0.111 (−0.227 to 0.005) | 0.061 | −0.013 (−0.037 to 0.010) | 0.264 | −0.008 (−0.021 to 0.003) | 0.164 | 0.008 (−0.192 to 0.208) | 0.934 |
| Temperature change (per 1 °C increase) | −0.532 (−1.080 to −0.034) | 0.026* | 0.078 (−0.078 to 0.235) | 0.323 | 0.002 (−0.032 to 0.036) | 0.887 | −0.019 (−0.035 to −0.003) | 0.024* | −0.434 (−0.708 to −0.160) | 0.002* |
Table 5
Comparison of effects of environmental factors on dry eye disease according to sex (multi-environmental factor analysis)
| Factor | SANDE score | Tear secretion (mm) | Tear film breakup time (sec) | Ocular staining score | Tear osmolarity (mOsm/L) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Men | ||||||||||
| Humidity change (per 1% increase) | −0.865 (−1.961 to 0.231) | 0.116 | −0.141 (−0.300 to 0.016) | 0.076 | −0.004 (−0.082 to 0.073) | 0.910 | −0.006 (−0.032 to 0.020) | 0.657 | −0.039 (−0.247 to 0.169) | 0.299 |
| Temperature change (per 1 °C increase) | −1.245 (−2.203 to −0.287) | 0.015* | −0.012 (−0.194 to 0.170) | 0.890 | 0.021 (−0.066 to 0.108) | 0.620 | −0.046 (−0.031 to −0.005) | 0.009* | −0.648 (−1.087 to −0.209) | 0.007* |
| Women | ||||||||||
| Humidity change (per 1% increase) | −0.465 (−0.935 to 0.003) | 0.052 | −0.073 (−0.225 to 0.078) | 0.336 | −0.008 (−0.037 to 0.022) | 0.914 | −0.007 (−0.022 to 0.007) | 0.314 | 0.044 (−0.199 to 0.288) | 0.717 |
| Temperature change (per 1 °C increase) | −0.572 (−1.067 to −0.075) | 0.025* | 0.022 (−0.141 to 0.186) | 0.785 | −0.006 (−0.031 to 0.018) | 0.589 | −0.012 (−0.028 to 0.003) | 0.114 | −0.340 (−0.656 to −0.023) | 0.036* |
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,591 View
- 65 Download
- Related articles
-
New Korean Guidelines for the Diagnosis and Management of Dry Eye Disease2024 April;38(2)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



