 |
 |
| Korean J Ophthalmol > Volume 37(5); 2023 > Article |
|
Abstract
Purpose
To evaluate the prevalence of dry eye symptoms after endoscopic dacryocystorhinostomy (EDCR) for patients with primary acquired nasolacrimal duct obstruction (PANDO) combined with dry eye syndrome.
Methods
The patients diagnosed with PANDO combined with dry eye syndrome who underwent EDCR were divided into two groups according to the questionnaire about dry eye symptoms after surgery. The medical records were retrospectively analyzed. Before and after surgery, we compared the tear meniscus height, tear breakup time, and the presence of corneal punctuate epithelial erosion. The level of dry eyes of patients after surgery was assessed by using the Korean guidelines for the diagnosis of dry eye.
Results
At 6 months after EDCR, the proportion of patients with dry eye symptoms was 30% in a total of 80 patients. The duration of epiphora and tear breakup time after EDCR were higher in the group without dry eye symptoms and the proportion of eyes with corneal punctuate epithelial erosion after EDCR was higher in the group with dry eye symptoms. About 15% of total patients started treatment with a dry eye of level 2 or higher.
Conclusions
About 15% of patients who underwent EDCR for PANDO combined with dry eye syndrome developed significant dry eye syndrome after surgery. The short onset of epiphora was associated with the development of the dry eye symptoms. Therefore, it is necessary to evaluate dry eye syndrome before surgery, and surgeons should be careful about this.
Tearing has many causes. Among them, primary acquired nasolacrimal duct obstruction (PANDO) is one of the most common causes, but reflex tearing is also one of the widespread causes, and there is an excessive secretion of tears due to dry eye syndrome [1]. In some cases, these two (PANDO and dry eye rebound tearing, etc.) are present together. Endoscopic dacryocystorhinostomy (EDCR) is the widely used method of PANDO treatment [1]. However, there are few papers analyzing the results after performing lacrimal surgery in patients with both of these factors. Oh et al. [2] reported on changes in the quality of life of patients after performing silicone tube intubation in patients with lacrimal stenosis and dry eye. However, as far as we are aware, there are no papers that report on the change and occurrence of dry eye symptoms in patients after EDCR. Therefore, the purpose of this study was to investigate the changes of dry eye symptoms after EDCR was performed in patients with both PANDO and dry eye.
We retrospectively analyzed the medical records of patients with PANDO combined with dry eye syndrome who underwent EDCR between March 2013 and April 2016 at the Department of Ophthalmology of Dongguk University Ilsan Hospital (Goyang, Korea). The Institutional Review Board of Dongguk University Ilsan Hospital approved this study and waived the need of informed consent (No. 2018-04-020-009). This study adhered to the tenets of the Declaration of Helsinki.
Inclusion criteria for this study were experiencing PANDO and undergoing EDCR by the same single surgeon, having an epiphora with dry eye syndrome, and having had at least 6 months follow-up time after surgery. Dry eye was diagnosed if tear breakup time (TBUT) is less than 10 seconds with punctate corneal erosion or symptoms related to dry eye syndrome. All patients enrolled in the study were evaluated by lacrimal probing and irrigation. The eyelid inspection focused on the location of the lacrimal punctum and the degree of lower lid laxity. Radiologic imaging with dacryocystography and dacryoscintigraphy were performed in each patient to identify the location of obstruction in the nasolacrimal duct, and only patients with PANDO were included in this study. Exclusion criteria were common canalicular obstruction, punctal ectropion, eyelid abnormalities, history of nasolacrimal surgery, and trauma. All patients enrolled in the study received endoscopic examination before surgery to exclude nasal cavity lesions, including mass, lesions, scars, and polyps.
In all patients, the silicone tube was removed 2 months after surgery and a survey was performed to patients through a subjective dry eye questionnaire. Until the removal of the silicone tube, levofloxacin 0.5% and flumetholone 0.1% eye drops were applied four times daily starting from the day after surgery. The enrolled patients were divided into two groups according to the subjective dry eye questionnaire: group 1 had no dry eye symptoms and group 2 did have symptoms 6 months after surgery if they had at least two of the following symptoms: dryness, foreign-body sensation, burning sensation, photophobia, visual fatigue or blurred vision, or red eye through a subjective dry eye questionnaire.
Patients were assessed for dry eye within 2 weeks before surgery (baseline) and 6 months after surgery in this sequence: (1) TBUT, (2) tear meniscus height (TMH), and (3) presence of corneal punctuate epithelial erosion (PEE). Furthermore, we used the Korean guidelines for the diagnosis of dry eye to evaluate the degree in patients who complained dry eye symptoms at postoperative 6 months (Fig. 1) [3].
To measure TBUT, we placed a fluorescein-impregnated strip in the lateral part of the inferior fornix; each patient was asked to blink, and the time before the corneal dry spot appeared in the stained tear film was recorded as the tear film breakup time. We measured the TMH using a video camera connected to a Haag-Streit slit-lamp. We defined grade 1 as 0.1 mm < TMH ≤ 0.2 mm, grade 2 as 0.2 mm < TMH ≤ 0.3 mm, grade 3 as 0.3 mm < TMH ≤ 0.4 mm, and grade 4 as 0.4 mm < TMH. We evaluated for corneal PEE after fluorescein staining under a yellow barrier filter and cobalt blue illumination, and we considered grade 2 or more positive following the Oxford system [4]. Each test was performed at least 5 minutes apart to exclude mutual influence between tests and was measured by the same person to reduce the error between measurers.
We performed all statistical analyses with IBM SPSS ver. 20.0 (IBM Corp). We tested the continuous variables for differences using the independent t of variance and categorical variables using chi-square analysis and linear by-linear regression. We considered p-value less than 0.05 significant.
The study population consisted of 80 patients, of whom 24 were male and 56 were female. The mean age of the subjects was 60.2 ± 12.1 years, ranging from 34 to 84 years. The duration of epiphora before surgery ranged from 2 months to 40 years, with a mean duration of 5.2 ± 8.1 years; the duration was significantly shorter in group 2 than in group 1 ( p = 0.014). There were no statistically significant differences in age, sex, laterality, presence of diabetes mellitus, presence of hypertension, or preoperative dacryocystitis between the two groups. Baseline characteristics of the patients are shown in Table 1.
We analyzed the proportion of patients complaining of dry eye symptoms after surgery according to their dry eye questionnaire findings. The proportions of patients who complained of postoperative dry eye symptoms were 11.3%, 8.8%, and 30.0% at 1, 2, and 6 months, respectively.
There was no statistically significant difference between the two groups in preoperative TBUT. However, there was a statistically significant difference in postoperative TBUT. At 6 months after surgery, TBUT was 6.1 ± 1.5 seconds in group 1 and 3.4 ± 1.1 seconds in group 2 ( p ≤ 0.01) (Table 2). There were also no statistically significant differences between the two groups in preoperative and postoperative TMH.
We also analyzed the proportions of patients who had corneal PEE before surgery and 6 months after surgery: before surgery, 7.1% in group 1 and 8.3% in group 2; 6 months after surgery, 1.8% in group 1 and 20.8% in group 2 (p = 0.003) (Table 2). That is, there was a statistically significant difference between groups in corneal PEE 6 months after surgery. Using the Korean guidelines for the diagnosis, we assessed dry eye levels in group 2 patients as follows: levels 1 (45.8%), 2 (41.7%), 3 (8.3%), and 4 (0%). Fifteen percent of all patients started treatment with a dry eye level of 2 or higher.
In our study, 24 patients (30%) who underwent EDCR subjectively complained of dry eye symptoms 6 months after surgery. None of these patients had complained of dry eye symptoms before surgery, but 12 patients (15%) were diagnosed with level 2 or higher following the Korean guidelines and required treatment for dry eye after surgery. In the remaining patients, symptoms were sufficiently mild that treatment of dry eye was not needed.
Patients who are suffering from tearing can be classified into two categories: tearing due to epiphora, which is mainly caused by obstruction or stenosis of the lacrimal drainage system; or hyperlacrimation, which can be caused by dry eye with reflex tearing, tear hypersecretion, and ocular surface disease [5]. Authors of a previous study [1] classified the tearing etiology into categories, and one of the most common causes is partial or complete nasolacrimal duct obstruction; 31.8% of patients who complained of tearing had nasolacrimal obstruction. However, these two different causes of tearing might not be independent but associated with each other.
The pathophysiology of PANDO has not yet been fully established, and nasolacrimal duct obstruction is known as obstructive fibrosis due to chronic inflammation of unknown cause [6,7]. In addition, infectious conjunctivitis [8], use of antiglaucoma medication [9,10], chronic sinusitis and chronic allergic diseases [11] are known to be causative factors, so that chronic inflammation of the lacrimal pathway is considered a cause of nasolacrimal duct obstruction. Dry eye is also related to inflammation, and some have reported that dry eye may also be a cause of PANDO.
Rose [12] found that tear evaporation led to significant concentrations of inflammatory mediators on dry ocular surfaces, resulting in impaired lacrimal drainage. Unlike the conjunctivodacryocystorhinostomy, in which there is a rationale for a possible postoperative “overdrainage” and the consequent “aqueous deficiency” dry eyes (as previously shown in Bladen et al. [13]), DCR has been actually suggested to be considered as a reasonable therapeutic option in cases of dry eyes with concomitant NLDO [12]. A previous study showed that tear clearance using lacrimal scintigraphy was significantly delayed in patients with dry eye [14]. In addition, dry eye aggravates the obstruction of lacrimal drainage system and causes involutional or atrophic changes of nasolacrimal duct [9].
Based on these findings, we assumed that among patients with PANDO, some might also have dry eye components, and our hypothesis was that some patients might have dry eye symptoms and signs after successful DCR based on our clinical experience. There are a number of objective tests for evaluating dry eye, such as TBUT, which reflects the stability of the tear film, corneal staining, and Schirmer test, but there is no method that can be an absolute standard in the diagnosis and evaluation of dry eye [15,16]. subjective symptoms are most important for patients, and it is more reproducible and reliable than objective tests even though subjective [17-19]. In this study, we used TBUT, TMH, and presence of corneal PEE to evaluate postoperative dry eye. In a previous study about changes to the tear film layer after DCR, specular images of the tear film in the cornea were examined and TMH was measured in five eyes; the lipid layer of the tear film after DCR was thicker than it before DCR, and the TMH was lower after surgery than before [20]. Francis et al. [21] found that lacrimal drainage surgery for PANDO reduced TMH measured by videoreflective dacryomeniscometry. Our study also showed decreased TMH after surgery compared with before surgery in both groups.
However, we classified the patients into two groups focusing more on their symptoms reported by the subjective questionnaire rather than these objective tests because of poor relationship between dry eye tests and symptoms. Additionally, some of the objective tests are less reliable in patients with PANDO than in those without it.
According to the outcomes of our study, there were three significant differences between the two groups: tearing onset, TBUT, and the severity of corneal staining after surgery; group 2 had a shorter onset time than did group 1. Moderate to severe dry eye might be more related to severe inflammation; it is possible that a relatively short-term but severe inflammatory response may cause lacrimal drainage pathway obstruction or worsen compared with patients without dry eyes before EDCR. On the other hand, in patients without significant dry eye before EDCR, lacrimal drainage pathway obstruction can develop slowly due to unknown causes over a long period of time. Most symptoms and signs of dry eye must be masked by PANDO. However, because EDCR causes tears to drain well, we thought that dry eye symptoms were revealed and heightened in patients who had severe dry eye. Almost 8% of patients had preoperative PEEs, and the average TBUT was 6 seconds, which is quite reduced and highly suggestive that some patients indeed had evaporative dry eyes (which were probably asymptomatic due to reflex tearing).
There are also some limitations to this study. First, this was a retrospective chart review study, and as such, we did not conduct some of the important assessments such as the Schirmer test and the Ocular Surface Disease Index. Furthermore, due to the retrospective nature of the study, objective assessments of PEE and at 1 and 2 months were not conducted, and this is presented as a limitation of the study. Second, some dry eye symptoms could be difficult to distinguish from symptoms caused by silicone tubes themselves such as allergic conjunctivitis. However, to minimize this confusion, we evaluated patients 2 months after we removed their silicone tubes, and we considered their outcomes reliable for this study. In addition, the sample size was small, and the follow-up periods were short. Nevertheless, to our knowledge, this is the first study to describe postoperative dry eye after EDCR.
In conclusion, about 15% of patients who underwent EDCR had significant dry eye syndrome. The short onset of tearing was associated with the development of the dry eye. Therefore, it is necessary to evaluate the dry eye before surgery, and surgeons should be careful about this.
References
1. Mills DM, Meyer DR. Acquired nasolacrimal duct obstruction. Otolaryngol Clin North Am 2006;39:979-99.


2. Oh JR, Chang JH, Yoon JS, Jang SY. Change in quality of life of patients undergoing silicone stent intubation for nasolacrimal duct stenosis combined with dry eye syndrome. Br J Ophthalmol 2015;99:1519-22.


3. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol 2014;28:197-206.



4. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003;22:640-50.


5. Mainville N, Jordan DR. Etiology of tearing: a retrospective analysis of referrals to a tertiary care oculoplastics practice. Ophthalmic Plast Reconstr Surg 2011;27:155-7.


6. Lee-Wing MW, Ashenhurst ME. Clinicopathologic analysis of 166 patients with primary acquired nasolacrimal duct obstruction. Ophthalmology 2001;108:2038-40.


7. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology 1986;93:1055-63.


8. Ohtomo K, Ueta T, Toyama T, Nagahara M. Predisposing factors for primary acquired nasolacrimal duct obstruction. Graefes Arch Clin Exp Ophthalmol 2013;251:1835-9.



9. Kashkouli MB, Rezaee R, Nilforoushan N, et al. Topical antiglaucoma medications and lacrimal drainage system obstruction. Ophthalmic Plast Reconstr Surg 2008;24:172-5.


10. Seider N, Miller B, Beiran I. Topical glaucoma therapy as a risk factor for nasolacrimal duct obstruction. Am J Ophthalmol 2008;145:120-3.


13. Bladen JC, Cascone N, Pearson AR, et al. Dry eye after Lester Jones tube insertion for epiphora. Orbit 2019;38:357-61.


14. Woog JJ. The incidence of symptomatic acquired lacrimal outf low obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 2007;105:649-66.


15. Perry HD, Donnenfeld ED. Dry eye diagnosis and management in 2004. Curr Opin Ophthalmol 2004;15:299-304.


16. Smith J, Nichols KK, Baldwin EK. Current patterns in the use of diagnostic tests in dry eye evaluation. Cornea 2008;27:656-62.


18. Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea 2004;23:272-85.


19. Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease. Cornea 2004;23:762-70.


Fig. 1
Korean guidelines for the diagnosis of dry eye. TBUT = tear breakup time. * Positive ocular signs may include conjunctival injection, lid abnormalities, and tear film abnormalities. However, these findings are not considered in the grading of disease severity; †Oxford system. Adapted from Hyon et al. [3], available under the Creative Commons License.
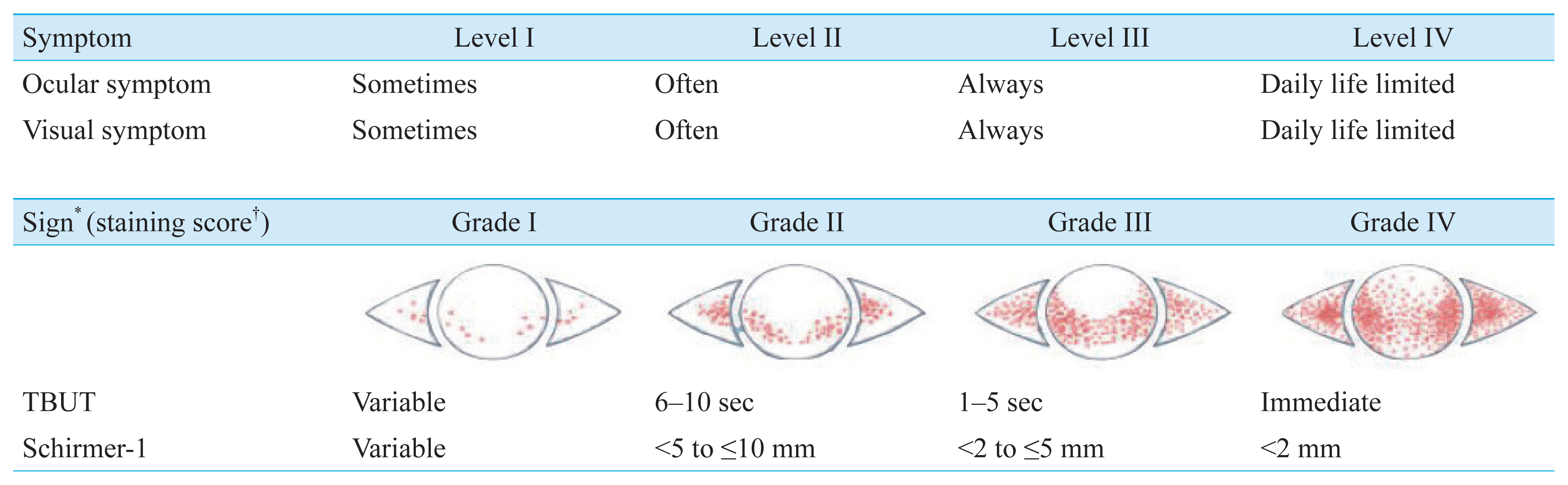
Table 1
Clinical characteristics (n = 80)
| Characteristic | Group 1 (n = 56) | Group 2 (n = 24) | p-value |
|---|---|---|---|
| Age (yr) | 60.7 ± 11.5 | 58.8 ± 13.5 | 0.564* |
| Sex | 0.301† | ||
| Male | 19 (33.9) | 5 (20.8) | |
| Female | 37 (66.1) | 19 (79.2) | |
| Laterality | 0.769† | ||
| Right eye | 26 (46.4) | 12 (50.0) | |
| Left eye | 30 (53.6) | 12 (50.0) | |
| Duration of epiphora (yr) | 6.4 ± 9.0 | 2.6 ± 4.5 | 0.014* |
| Diabetes mellitus | 6 (11.4) | 2 (10.2) | 0.923† |
| Hypertension | 20 (36.4) | 8 (31.6) | 0.715† |
| Dacryocystitis | 7 (12.5) | 3 (12.5) | >0.999† |
Table 2
Comparison of preoperative and postoperative 6 months corneal PEE and TBUT between two groups
| Variable | Preoperative | Postoperative 6 mon | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Group 1 (n = 56) | Group 2 (n = 24) | p-value | Group 1 (n = 56) | Group 2 (n = 24) | p-value | |
| Corneal PEE (%) | 7.1 | 8.3 | 0.853* | 1.8 | 20.8 | 0.003* |
| TBUT (sec) | 5.9 ± 1.5 | 5.8 ± 2.4 | 0.874† | 6.1 ± 1.5 | 3.4 ± 1.1 | <0.001† |
- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




