Kimura Disease with Lacrimal Sac and Nasolacrimal Duct Involvement: A Case Report
Article information
Dear Editor,
Kimura disease (KD) is a rare allergic or autoimmune chronic inflammatory disease of the soft tissue in the head and neck region. Painless subcutaneous masses are presented in the salivary glands, lymph nodes, or deep subcutaneous tissue, which frequently occur in young Asian men. The periocular invasion has been reported in orbit, lacrimal gland, and medial canthus [1,2]. However, the invasion of the nasolacrimal duct along the inside of the lacrimal sac has not been reported. Compared to the angi-olymphoid hyperplasia with eosinophilia (ALHE), KD extends to deeper tissue, and when the lacrimal sac or nasolacrimal duct is invaded, epiphora can be the main symptom. Furthermore, in a fibroinflammatory disease spectrum, immunoglobulin G4-related disease (IgG4-RD) should be differentially diagnosed. Herein, we report a case of KD with lacrimal sac and nasolacrimal duct involvement, along with the differential diagnosis process. Informed consent for publication of the research details and clinical photographs was obtained from the patient.
A 64-year-old man presented with enlarged swelling of both his inner canthus accompanied by bilateral tearing for ten months (Fig. 1A). He had no history of surgery or trauma at the periorbital area and only had a medical history of hypertension and hypertensive chronic renal failure. On physical examination, a hard palpable mass at the medial canthus and tear trough area was noted in both eyes, and the lymph nodes behind the ear were palpated. Orbital magnetic resonance image revealed T1-weighted contrast-enhanced soft tissues not only in both medial canthi but also in the lacrimal sac and along nasolacrimal ducts (Fig. 1C, 1D). He underwent an incisional biopsy on the mass at his left medial canthus. In histopathological examination, lymphoid follicles with germinal centers and eosinophilic abscess were formed in the stromal fibrosis, and abundant eosinophils and IgG4 plasma cells were infiltrated (Fig. 1E–1H). Blood samples showed eosinophilia (15.6%; normal range, 0%–7%), elevation in serum IgE level (>5,000 IU/mL; normal range, 0–100 IU/mL), and normal range of serum IgG quantitation (1,253 mg/dL; normal range, 700–1,600 mg/dL) and IgG4 concentrations (1,120 mg/L; normal range, 30–2,010 mg/L). Based on the patient’s clinical features, histological examination, and blood tests, the patient was diagnosed with KD. After the patient was administered 30 mg of prednisolone for a week, the symptoms improved (Fig. 1B), and the steroid was tapered out.
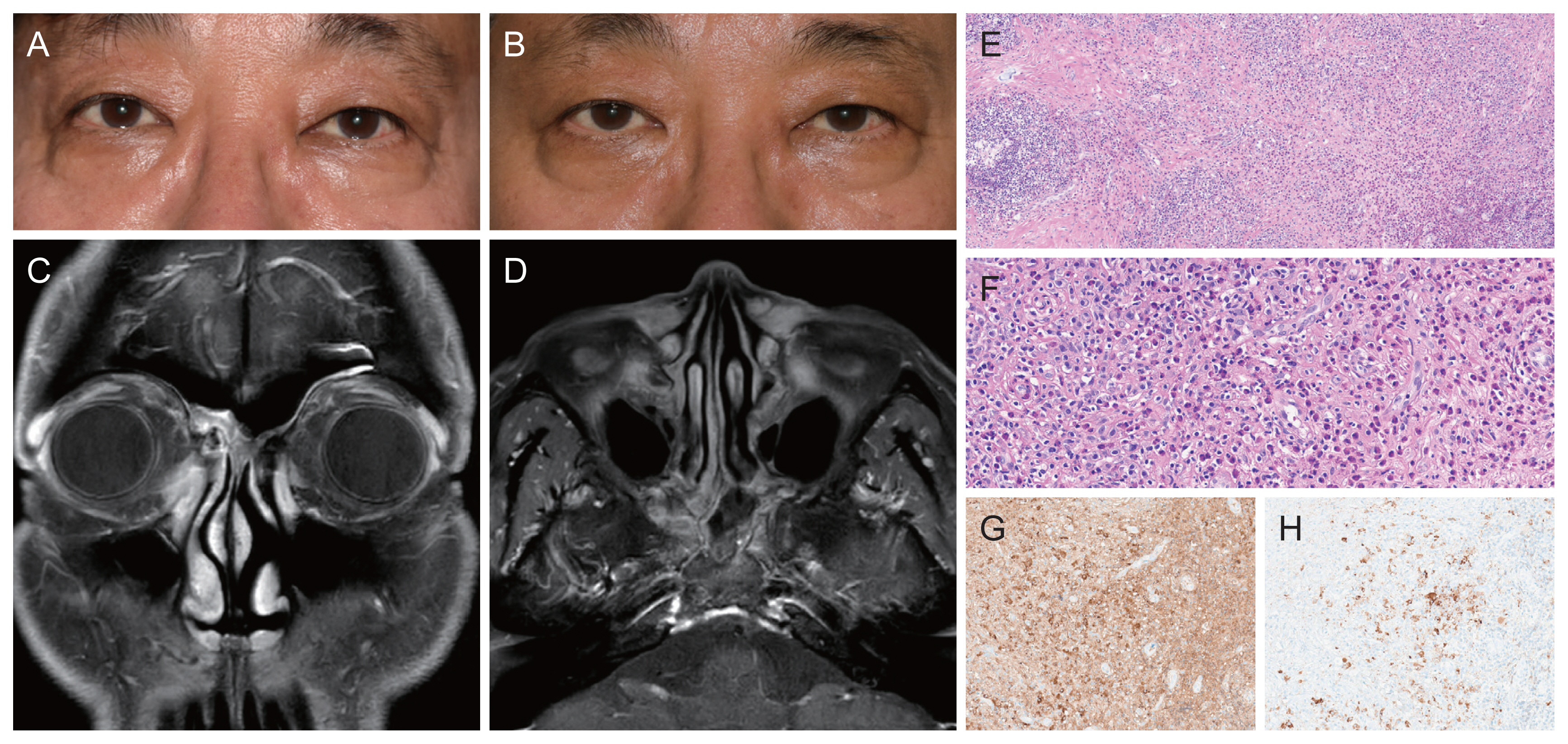
Clinical and histopathologic findings of the patient. (A) Clinical photograph of the patient at the initial visit. Firm oval shaped palpable masses sized 1.0 × 2.5 cm arising from the medial canthus and continuing to the tear trough in both eyes were observed. (B) Clinical photograph after prednisolone treatment. The palpable masses at the medial canthus and tear trough in both eyes were improved. (C) Coronal view of magnetic resonance image. T1-weighted gadolinium-enhanced fat suppression image revealed enhancement of both lacrimal sacs. (D) Axial view of magnetic resonance image. T1-weighted gadolinium-enhanced fat suppression image showed enhanced nasolacrimal duct and soft tissue at the tear trough region in both eyes. (E) Microscopic finding of the specimen with a low-power view. Mixed inflammation with abundant eosinophils was seen in the background of lymphoid follicles and stromal fibrosis (hematoxylin-eosin, ×100). (F) Microscopic finding of the specimen with higher magnification. Marked eosinophils were infiltrated with polymorphous population of lymphocytes and plasma cells (hematoxylin-eosin, ×400). (G) Immunoglobulin G (IgG) immunohistochemical staining (×200). (H) IgG4 immunohistochemical staining (×200). High IgG4/IgG ratio (>40%) and high IgG4 plasma cell counts (63 cells/high power field) was shown. Informed consent for publication of the clinical photograph was obtained from the patient.
The patient in the present report had KD invasion in the lacrimal sac and nasolacrimal duct as well as medial canthus, causing epiphora and palpable masses. For a differential diagnosis with ALHE and IgG4-RD, the location of occurrence, clinical features, histopathology, and serology should be comprehensively considered. Unlike ALHE, which is a benign vascular proliferative tumor manifested as more superficial hemangiomatous papules or nodules on the face, KD usually presents as a discrete subcutaneous mass accompanied by lymph node involvement, and is characterized by eosinophilia, IgE elevation, and systemic symptoms such as nephrotic syndrome [1,2]. Recently, differentiation from IgG4-RD, histologically showing stromal fibrosis and lymphocyte infiltration like KD, is also required. According to the 2019 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria for IgG4-RD, if a tumor-like mass or histological finding showing lymphoid plasma cell infiltration is involved in typical organs including the orbit and lacrimal gland, entry criteria is met. However, eosinophilia is an exclusion criterion for IgG4-RD as a second step; therefore, other diseases should be considered first if such hematologic values are observed [3]. Furthermore, IgG4 plasma cell invasion can also occur in neoplastic diseases or other inflammatory diseases including KD [4,5]. As a result, it should be diagnosed through comprehensive consideration that includes histopathology, serology, and clinical features of specific organs, not diagnosed solely on the basis of IgG4-positive cell infiltration. In this case, except for the immunostaining, enlargement of lymph nodes, elevated serum IgE levels, and eosinophilia were observed, and typical histological findings such as follicular hyperplasia with reactive germinal centers, eosinophilic infiltration, eosinophilic abscess, and interstitial fibrosis without storiform fibrosis and obliterative phlebitis played a critical role in the diagnosis of KD.
In conclusion, for patients who come to the hospital with tears accompanied by medial canthal swelling, it is necessary to take KD into consideration and imaging study, blood tests and biopsy are essential for accurate diagnosis and treatment.
Acknowledgements
None.
Notes
Conflicts of Interest: Jin Sook Yoon is a member of the Editorial Board of the Korean Journal of Ophthalmology since 2022. However, she was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding: None.