Dermatochalasis is an eyelid disease that develops due to excess skin tissue on the upper eyelids, mostly occurs with advancing age, affects the field of vision and creates a feeling of heaviness [1]. There may be pain, erythema, and edema after surgery, as well as pain during surgery [2]. Intraoperative and postoperative pain management should be performed with appropriate and potent analgesic agents before operation [3]. Considering the potential effect of pain, it is necessary to keep the patients posted in detail before the procedure and different studies have shown that appropriate and adequate preoperative information is important in postsurgical recovery [4-6]. Because pain differs from person to person and becomes more important in individuals with high anxiety [7].
The pain assessment of patients after first and second eye surgery in different ophthlamic surgeries was evaluated and contributed to the literature [8-10]. To the best of our knowledge, no study has been found on which eyelid pain is felt more during surgery in upper eyelid blepharoplasty (UEB). The aim of this study is to contribute to the preoperative detailed information of the patient and intraoperative pain management by evaluating whether the pain felt during upper eyelid dermatochalasis surgery is more in the first operated or second operated eyelid.
Materials and Methods
This cross-sectional observational study was performed at a tertiary ophthalmology clinic from January 2022 to January 2023, with approval from the Institutional Review Board of Ankara City Hospital (No. E1-23-3195). The study adhered to the tenets of the Declaration of Helsinki and an informed consent was obtained from all subjects included in this study.
Eighty patients who had undergone UEB surgery for upper eyelid dermatochalasis were included in the study. Patients with diabetes mellitus, hypertension, anxiety, panic attack, cardiovascular disease history, preoperative nonsteroidal anti-inflammatory medicine use, analgesic or additional medicine use, and smokers were excluded in the study.
Preoperative detailed anamnesis of all patients was taken. Dermatochalasis affecting the field of vision was controlled with the confrontation test. All surgeries were performed under local anesthesia. Before the procedure, marking was made with a surgical skin marker pen, 8 to 10 mm above the lash line and 8 to 10 mm below the lower border of the eyebrow, in line with the upper eyelid fold. It was checked through forceps. The marked areas were rechecked with forceps in the supine position. After appropriate and adequate surgery site cleaning, surgical procedure was started on the first right upper eyelid of 40 patients and the left upper eyelid of the other 40 patients. Before the local anesthesia, all patients were informed ŌĆ£I will apply a local anesthetic to your eyelid soon, you may feel a slight pain on the first contact with your skin, but this pain is not unbearable and the injection process will take a short time, after this procedure you will not feel such pain in other stagesŌĆØ. The upper eyelid was infiltrated with a mixture of 2% lidocaine and 1:200,000 epinephrine, and a scalpel blade was used to make a scratch incision along the marked lines. An equal amount of local anesthetic was applied to both upper eyelids. After local anesthesia, it was waited for 5 minutes for the distribution of the anesthetic substance. Afterwards, an incision line was created from the marked areas with the help of a sharp-edged cutter. Starting from the medial region, the skin and subcutaneous tissue were excised through a cutter moving towards the lateral, without excising the orbicularis muscle tissue. After the excision, the bleeding areas were kept under control using cautery. One 6.0 polyglactin vicryl suture was placed in the medial, central, and lateral regions to protect the upper eyelid crease line. Starting from the medial region and continuing towards the lateral region, it was sutured with a 6.0 polyglactin vicryl suture. After the first operated eyelid surgery was completed, the same amount of local anesthetic was applied to the second operated eyelid. After that, the same procedures were applied to the second operated eyelid with all its stages. The same procedures were performed on all patients in the same order by the only surgeon (EKA) experienced in the department of oculoplasty. Postoperatively, the wound was closed with oxytetracycline ophthalmic ointment. At the end of the procedure, all patients were asked to rate and express their pain during each eyelid surgery using the visual analoge scale (VAS) and the Wong-Baker Facial Pain Expression Scale (WBFPES).
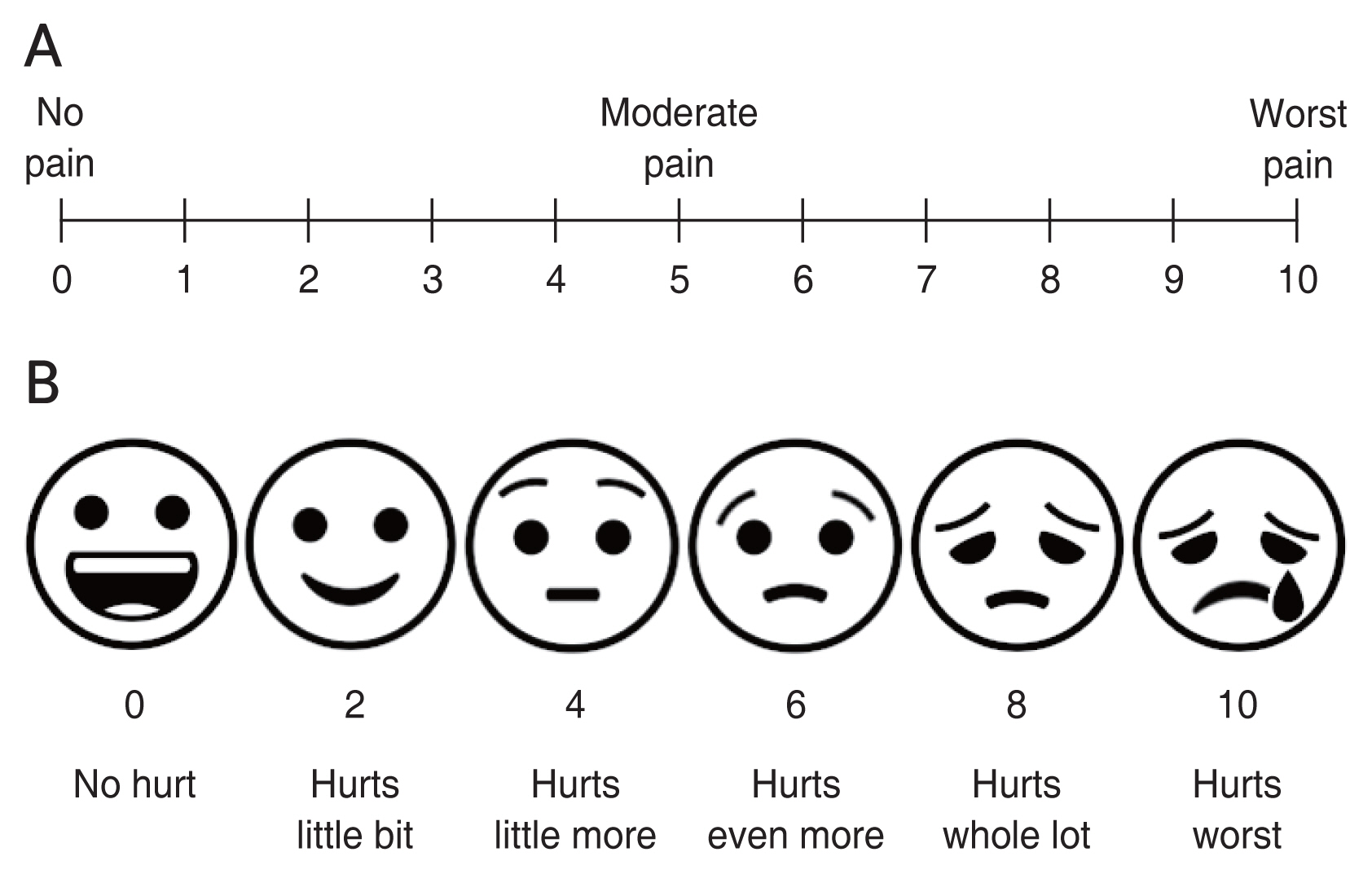
In the VAS, ŌĆ£no painŌĆØ was classified as 0 and ŌĆ£excruciating painŌĆØ was classified as 10 points (Fig. 1A). The pain felt by the patient after each eyelid surgery was scored by the patient. In addition, patients were asked to choose a facial expression that represented the pain felt during both eyelid surgeries using the WBFPES (Fig. 1B).
IBM SPSS ver. 22 (IBM Corp) was used for statistical analysis. Quantitative values were stated as mean ┬▒ standard deviation. The conformity of the data to the normal distribution was evaluated visually by histogram and statistically by the Shapiro-Wilks test. Continuous data were analyzed with paired sample t-test as the data conformed to the normal distribution. A value of p < 0.05 was considered statistically significant.
Results
Eighty patients who underwent UEB due to bilateral upper eyelid dermatochalasis were included in the study. There were 40 patients in group 1 who had blepharoplasty on the right upper eyelid first, and 40 patients in group 2 who had blepharoplasty on the left upper eyelid first. The mean age of group 1 was 51.8 ┬▒ 5.2 years, and the mean age of group 2 was 50.9 ┬▒ 5.6 years (p = 0.65). There were 20 female and 20 male patients in both groups (Table 1).
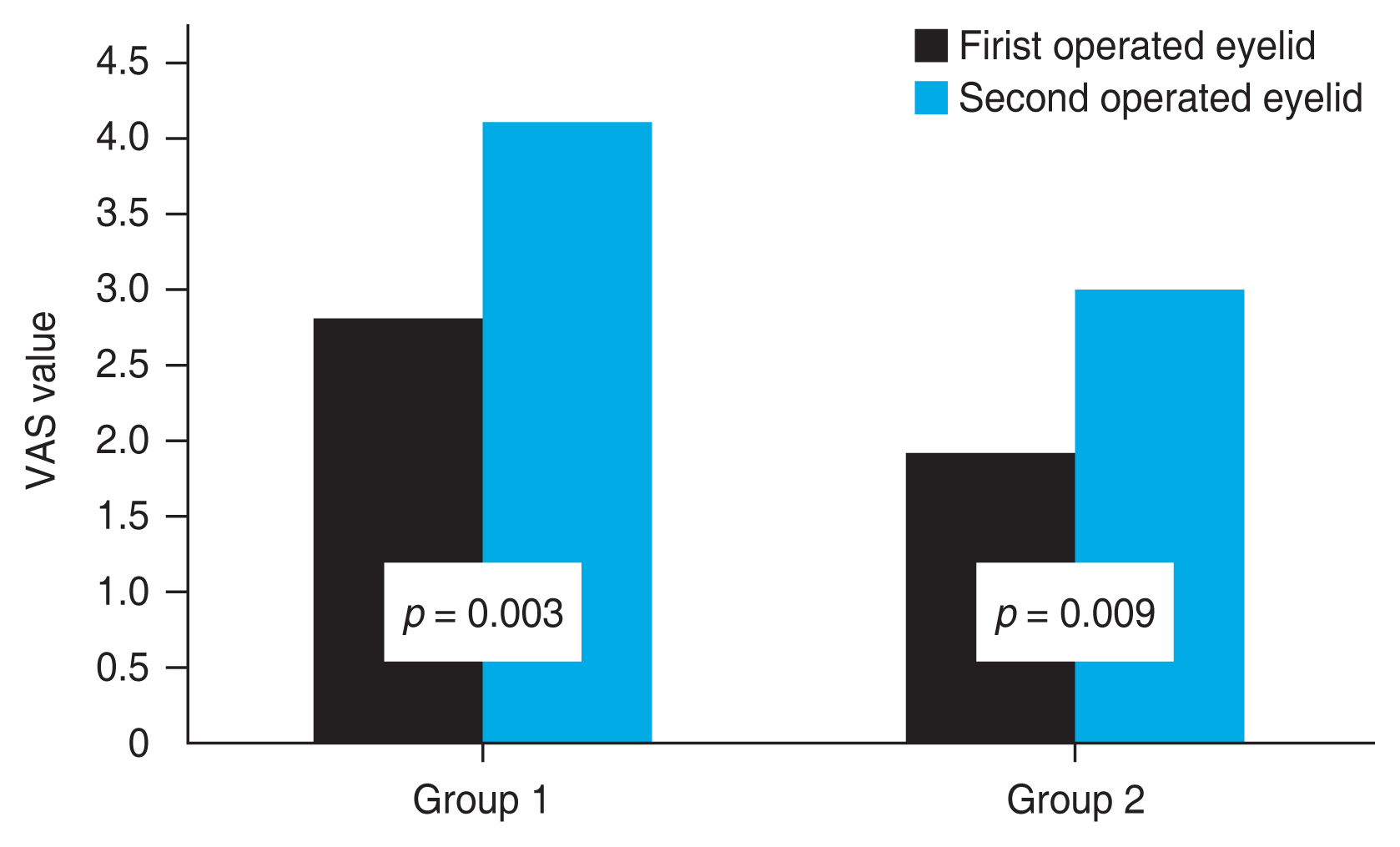
In group 1, the VAS value after the first operated upper eyelid surgery was 2.8 ┬▒ 1.5 and the VAS value after the second operated upper eyelid surgery was 4.1 ┬▒ 1.8 and there was a statistically significant difference (p = 0.003). The WBFPES value was 2.7 ┬▒ 1.6 after the first operated upper eyelid surgery and 3.9 ┬▒ 1.8 after the second operated upper eyelid surgery, and there was a statistically significant difference (p = 0.002).
In group 2, the VAS value after the first operated upper eyelid surgery was 1.9 ┬▒ 1.0 and the VAS value after the second operated upper eyelid surgery was 3.0 ┬▒ 1.5, and there was a statistically significant difference (p = 0.009). The WBFPES score was 2.0 ┬▒ 1.0 after the first operated upper eyelid surgery and 2.8 ┬▒ 1.6 after the second operated upper eyelid surgery, and there was a statistically significant difference (p = 0.005) (Table 2).
Discussion
UEB is a surgical procedure performed secondary to sagging of the eyelids [11]. Although there are studies on the evaluation of pain after the first and second eye in different ophthalmic surgeries in the literature, there was no study on which eyelid pain was more common in UEB surgery. For this purpose, the pain felt in the eyelids in UEB surgery was compared in this study.
Local anesthesia is generally preferred in UEB [11]. Local anesthesia does not have a risk compared to both general anesthesia and sedation applications and an additional anesthesiologist or technician is not required for its application. In a study evaluating the effects of lidocaine and prilocaine (used as local anesthetics) on pain, pain was found to be lower in cases where lidocaine was applied [12]. In previous studies evaluating the effect of lidocaine and prilocaine on pain, it has been reported that prilocaine has a similar effect or causes less pain than lidocaine [13,14]. The pain felt during local anesthetic injection is caused by the insertion of the needle or the passage of the medicine into the tissues with filtration. The mechanism of pain formation is the transport of afferent impulses along the A-delta fibers by stimulation of paccini corpuscles, mechanoreceptors and Ruffini terminals [15]. The effect of lidocaine begins quickly and the mean duration of action of mixtures with epinephrine is 2.2 hours (range, 2-4 hours) [16]. In our study, the mean duration of UEB surgery was 45 minutes. Therefore, in our study, we performed UEB with a local anesthesia method to all patients and our local anesthetic medicine of choice was lidocaine. Longer-acting local anesthetics than lidocaine can also be used. For example, the mean duration of action of bupivacaine is 4.3 hours (range, 4-12 hours). However, its effect starts slowly, and systemic side effects are known [17].
VAS is a scoring scale used in the evaluation of pain in different diseases in clinical practice. On this scale, 0 points describe no pain, and 10 points describe unbearable pain. Pain scores were evaluated with VAS before and after treatment in 2,879 patients using pregabalin for chronic pain and a reduction in pain value of 2 points or more was reported in 30% of patients [18]. Although this scoring is preferred in chronic pain, it has been stated that it may be more appropriate in the assessment of acute pain. For this reason, we applied the pain assessment at the end of the surgery when the patient felt the best. This time was about 5 to 10 minutes. In the study of Lee et al. [19], in the evaluation of the mean pain scores from the end of the surgery to the 1st month, it was found that the pain decreased at each visit.
In a study evaluating pain after cataract surgery, topical anesthesia was applied in both eye surgeries, and it was reported that VAS and WBFPES values were higher in secondary eye surgery [20]. In the study of Sharma et al. [21], sedation was preferred as anesthesia, pain conditions were evaluated after cataract surgery in the first and second eyes and no significant difference was found between the pain scores of the two eyes. The reason they came to this conclusion may be that pain assessment is not done properly while the patient is under sedation. In the study of Bardocci et al. [22], no difference was found between the pain scores of cataract surgery in both eyes. In the study of Jiang et al. [20], it was thought that pain was felt more in second eye surgery and that the patient focused more on the concerns about the success of the surgery in first eye surgery. In a meta-analysis on cataract surgery, it was reported that pain is more common in second eye surgery as a result. They reported that in first eye surgeries, patients focus more on the course of the surgery, in harmony with previous studies, and that pain sensation may come to the fore in second eye surgery after successful operation [23].
It is known that pain is associated with inflammation and a significant relationship has been reported between various mediators and pain score. Similar to our study, Zhang et al. [24] evaluated pain in patients who underwent first and second eye cataract surgeries, and found that monocyte chemotactic protein was higher in the aqueous in the second eye surgery and stated that this mediator may be associated with pain. In diabetic cataract patients, substance P and monocyte chemotactic protein 1 levels evaluated from the aqueous fluid taken in first and second eye cataract surgery were found to be higher in second eye surgery, and it has been reported that these mediators that are associated with pain, play a role in sympathetic inflammation, and may cause noninfectious inflammation. As a result, it was thought that cataract surgeons should be more careful of pain in second eye surgery [25].
Lee et al. [19] assessed pain scores in UEB in 30 Asian patients. At the end of the operation, pain scores were asked by VAS at the postoperative 2nd and 4th hours, and on the 1st, 2nd, 7th, and 30th days postoperatively and they found it to be 2.9 in all patients, 3.5 in female patients and 2.2 in male patients at the end of the operation. In our study, the score was 2.8 in the first operated upper eyelid surgery, 4.1 in the second operated upper eyelid surgery in the group that started with the right upper eyelid first and 1.9 in the first operated eyelid surgery and 3.0 in the second operated upper eyelid surgery in the group that started with the left upper eyelid. Pain score was significantly higher during the second operated eyelid surgery in both groups (Fig. 2).
Among the limitations of our study, the lack of patients belonging to different races can be counted as the first. Another is that not all patients have the same eyelid structure, and the excised skin and subcutaneous tissue are uneven. In addition, the VAS score, which we use in pain assessment, is a subjective measurement based on patient interpretation and evaluates 11 points between 0 and 10. More objective results can be obtained with evaluations on a wider scale. Another limitation is the inability to compare the effect different local anesthetic medicine on the pain felt during operation on the second eyelid.
Pain can usually be defined as the fifth vital sign. Knowing the presence of pain and evaluating its severity are important on the physical and psychosocial function of the person. As a result, patients may experience pain at a level that does not seriously affect their comfort of life in UEB. More pain may be related to the fact that patients are more interested in the course and outcome of the surgery at the beginning of the surgery and that this anxiety decreases after a while. Another possible mechanism is that pain begins to be learned after the beginning of surgery and is expressed more clearly towards the end. In this study, pain scores were found to be higher in the second operated upper eyelid surgery in both upper eyelid surgeries that started with both the right upper eyelid and the left upper eyelid. For this purpose, local anesthetics should be used in the second operated upper eyelid surgery in the light of this information. Our preference is to apply anesthesia to the second operated eyelid before suturing the first operated eyelid. In addition, the patient should be given detailed information about pain before the operation.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






