Dear Editor,
Double primary malignancies are relatively rare, occurring in only 0.18% of cancer patients, according to a study that analyzed 23,260 cancer patients who were registered to a regional cancer institute in India [
1]. Double primary malignancies can be totally incidental, but it can also be relevant to note whether they share inherited, environmental, and iatrogenic risk factors. It has been reported that multiple myeloma (MM) patients show an increased incidence of squamous cell carcinoma (SCC) [
2]. To the best of our knowledge, however, this is the first case report of conjunctival SCC in a MM patient. Written informed consent for publication of the research details and clinical images was obtained from the patient.
A 69-year-old man with a past history of coronary artery occlusive disease, chronic kidney disease, and MM, was referred to the Department of Ophthalmology, Severance Hospital, Yonsei University College of Medicine (Seoul, Korea) for conjunctival mass in his left eye. About 1 year prior to his visit, he was diagnosed with MM at Severance Hospital, and went through nine cycles of a bortezomib-melphalan-prednisolone (VMP) regimen systemic chemotherapy.
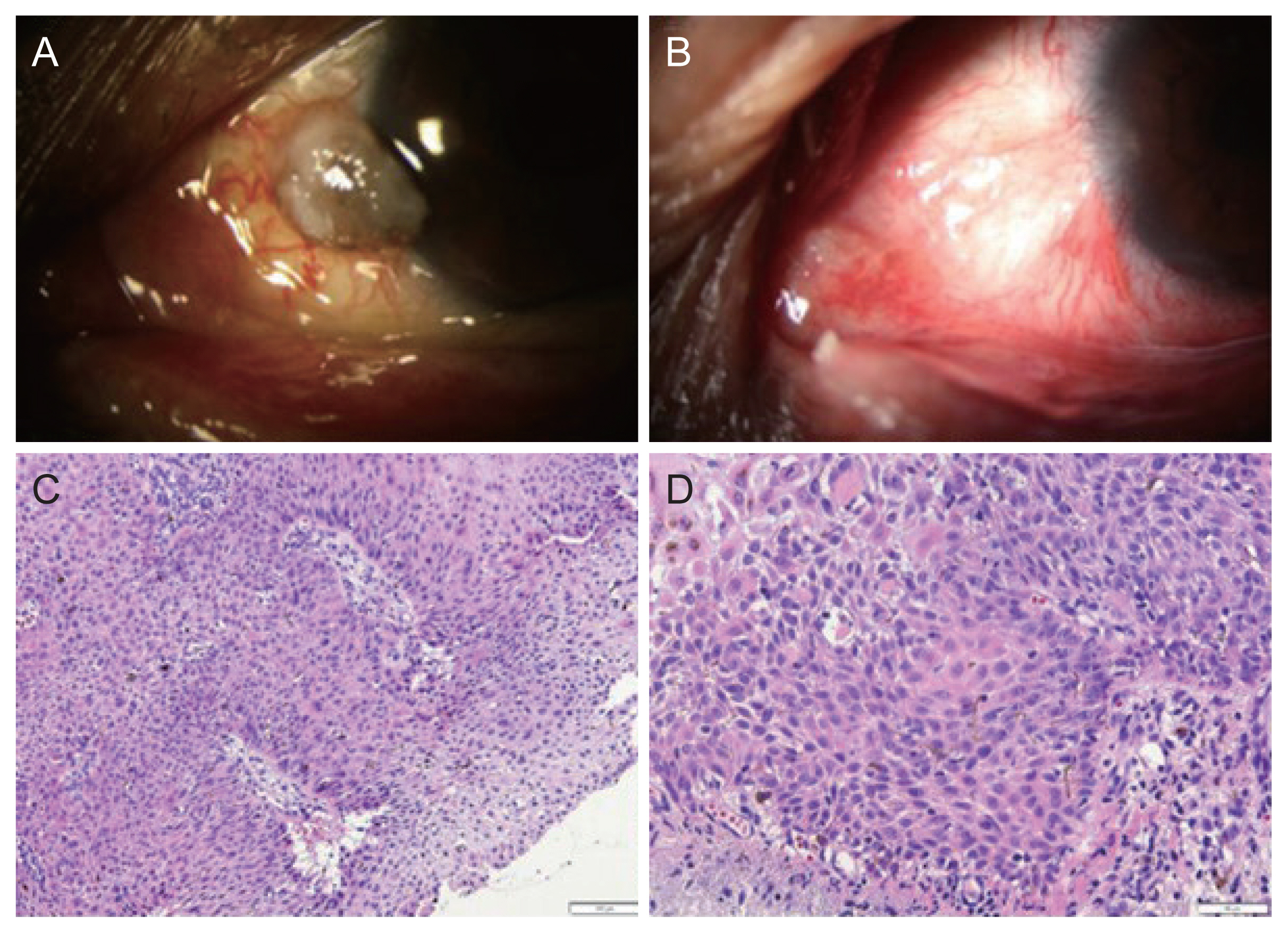
Upon the slit-lamp examination of his left eye, gray-whitish, gelatinous, well circumscribed, immobile, elevated 2 ├Ś 2-mm sized conjunctival mass was detected at the nasal perilimbal area (
Fig. 1A). The morphologic findings and location suggested the impression of conjunctival intraepithelial neoplasia or SCC.
Conjunctival mass excision with biopsy and local cryotherapy was done on July 1, 2020. The biopsy results confirmed the diagnosis of well differentiated type of SCC. Hematoxylin-eosin-stained sections presented with nests of atypical squamous cells (
Fig. 1C, 1D). Postoperative orbital magnetic resonance imaging with contrast enhancement showed no residual tumor, and interferon alfa-2a 1 mIU/mL eye drops, made from Roferon-A prefilled injection (3 mIU/0.5 mL, Roche), were applied to his left eye four times a day for 1 month as an adjuvant chemotherapy. After this course, 0.04% mitomycin C (MMC) eye drops, diluted from MMC injection 10 mg (Korea United Pharm Inc) were used four times per day since, interferon alfa-2a became unavailable. After three cycles (one cycle meaning 2 weeks of use and 2 weeks of rest) of topical MMC chemotherapy, regular follow-ups were done for 2.5 years and no recurrence was noticed until the last follow-up on January 5, 2023 (
Fig. 1B).
The association between MM and nonmelanomatous skin cancer (NMSC) has been noticed relatively recently, since MM patients have begun to live longer with improved treatment techniques. Robinson et al. [
2] designated MM diagnosis as one of the significant predictors of skin cancers, along with age and Caucasian ethnicity. Among the skin cancers, SCC was found to be significantly more related to MM than basal cell carcinoma (BCC).
The reason for this association between MM and SCC has not been clearly established, but one plausible theory blames the immunocompromised nature of MM patients. MM causes the formation of abnormal plasma cells, which leads to systemic immunodeficiency through various mechanisms. Immunodeficiency facilitates the proliferation of human papillomavirus, which acts as a cocarcinogen of the skin cancer. Euvrard et al. [
3] reported that immunosuppression in solid organ transplant recipients resulted in 65- to 250-fold and 10-fold increased risks of developing SCC and BCC, respectively.
Another theory focuses on MM treatment-related risk factors for second primary malignancies. The major drugs used in MM therapy include alkylating agents (melphalan, cyclophosphamide), corticosteroids (dexamethasone, prednisone), immunomodulatory drugs (thalidomide, lenalidomide, pomalidomide), and proteasome inhibitors (bortezomib, carfilzomib, ixazomib). Combinations of two or more of these drugs are the current standard treatment options for MM. Musto et al. [
4] reviewed and concluded that the incidence of second primary malignancies increased when lenalidomide was administered either after or concurrently with melphalan.
Here, we report a second primary conjunctival SCC in a MM patient. There has been a recent report of orbital SCC in a MM patient [
5], but this is the first report of conjunctival SCC in a MM patient, to the best of our knowledge. Although an explicit mechanism of the relationship between MM and SCC has not yet been established, there are some possible theories, and further research is needed to fully understand the relationship. Hematological clinicians who deal with MM patients are advised to pay more attention to suspicious skin lesions, and even to the conjunctival masses of MM patients, since they may be indicative of SCC.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



