Dear Editor,
Gonococcal conjunctivitis is typically a neonatal disease. However, the incidence of gonococcal conjunctivitis in adults is increasing because of the increased frequency of urogenital gonococcal infections [1]. Most cases occur in neonates or sexually active adults. It is rarely considered in older children or adolescents. Since it is relatively rare in adolescents, clinical diagnosis may be delayed [2,3]. Inappropriate treatment timing means that gonococcal conjunctivitis could progress in a rapid and fulminant fashion, threatening patientsŌĆÖ vision. If systemic antibiotic therapy and topical eye-drop treatment are instituted before severe corneal complications occur, serious sequelae and visual loss could be reduced. We report a rare case of acute gonococcal conjunctivitis in an adolescent teenager diagnosed using a bacterial culture test without any ocular complications. The patient provided informed consent for the publication of clinical photographs.
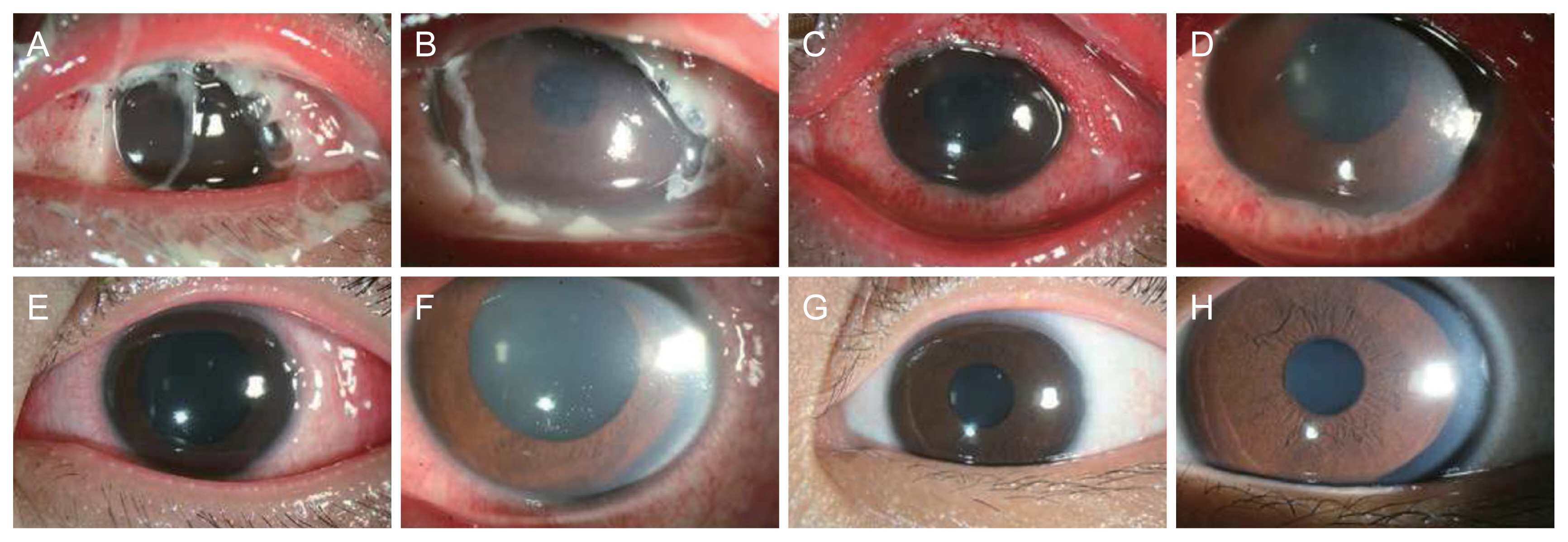
A 13-year-old adolescent boy presented with severe eyelid swelling and ocular pain with purulent discharge from the left eye, which started 5 days before presentation. The best-corrected visual acuity (BCVA) of the right eye was 20/20 and that of the left eye was 20/400. Severely decreased visual acuity of the left eye was observed. Slitlamp examination revealed unremarkable findings in the right eye; however, the left eye showed severe chemosis with conjunctival injection, vessel dilatation, and multiple tarsal conjunctival follicles. Diffuse superficial punctate corneal lesions with hazy and mild edema and purulent discharge in the conjunctival sac were also observed (Fig. 1A, 1B). The patient denied a history of sexual contact and showed no evidence of genitourinary symptoms. However, because gonococcal conjunctivitis was strongly suspected, bacterial culture using a disinfectant swab was performed at the first visit, and other laboratory examinations and urine analyses were performed. This patient, with gram-negative intracellular diplococci on Gram stain, subsequently had positive conjunctival cultures for Neisseria gonorrhoeae. Other blood markers of inflammation, such as C-reactive protein and erythrocyte sedimentation rate, were slightly elevated, but urinalysis results were normal.
The patient was administered a single dose of 1 g of intravenous ceftazidime (Cefazim, HK inno.N) and 500 mg azithromycin (Zithromax, Pfizer Inc) orally twice a day for 5 days. Topical fortified tobramycin and cephalosporin eye drops were instilled every 1 hour. Within a day, the patient showed reduced ocular discharge and inflamed conjunctiva (Fig. 1C, 1D). Topical fortified eyedrops were tapered and used every 2 hours. After 5 days, the BCVA of the left eye was 20/50, and conjunctival injection and corneal haziness improved (Fig. 1E, 1F). The patient was discharged after 5 days of treatment. Topical fortified eyedrops were used four times a day. After 2 weeks, the left eye BCVA was 20/20, and eyelid swelling, corneal haziness, and conjunctival injection were mostly reduced; corneal edema remained slight. Topical fortified eyedrops were stopped, and the patient was switched to levofloxacin eye drops. Three weeks after discharge, the patient had a visual acuity of 20/20 in the left eye without any conjunctival or corneal complications (Fig. 1G, 1H).
To our knowledge, this is the first report of acute gonococcal conjunctivitis in an adolescent in Korea. The patient reported no history of sexual contact. Nevertheless, the clinical symptoms strongly suggested the possibility of N. gonorrhoeae conjunctivitis. There have been reports of nonsexual transmission of gonococcal infection in an 11-year-old girl by a thermal pool [4]. In adolescent patients, sexual abuse should always be the first consideration and should be investigated. No evidence of sexual assault or other sexually transmitted infections was found in the urinalysis or genitourinary evaluations. Many studies have been conducted to determine the survival time of gonococci on several materials, such as towels and sheets. Gonococcus was found in almost all materials after 24 to 48 hours and survive up to 72 hours or more on certain materials [5]. In previous report, gonococcal conjunctivitis did not necessarily require sexual contact as an antecedent factor [4,5]. Therefore, if gonococcal conjunctivitis is strongly suspected, a conjunctival culture test to confirm gonococci can be helpful in the diagnosis.
In conclusion, acute gonococcal conjunctivitis can be observed in young adolescents who are sexually inactive. Therefore, conjunctival swap culture helps diagnose gonococcal infection and conjunctivitis presenting with severe purulent discharge. Systemic intravenous third-generation cephalosporin and oral azithromycin intake were effective in relieving the symptoms of gonococcal conjunctivitis.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






