Dear Editor,
Several SARS-CoV-2 vaccines, including messenger RNA vaccines (BNT162b2, Pfizer-BioNTech) and adenovirus vector vaccines (ChAdOX1 nCov-19, AstraZeneca), have been approved for use worldwide. However, ocular side effects have rarely been reported. Herein, we report the case of corneal graft rejection after ChAdOX1 vaccination. The patient provided written informed consent for publication of the research details and clinical images.
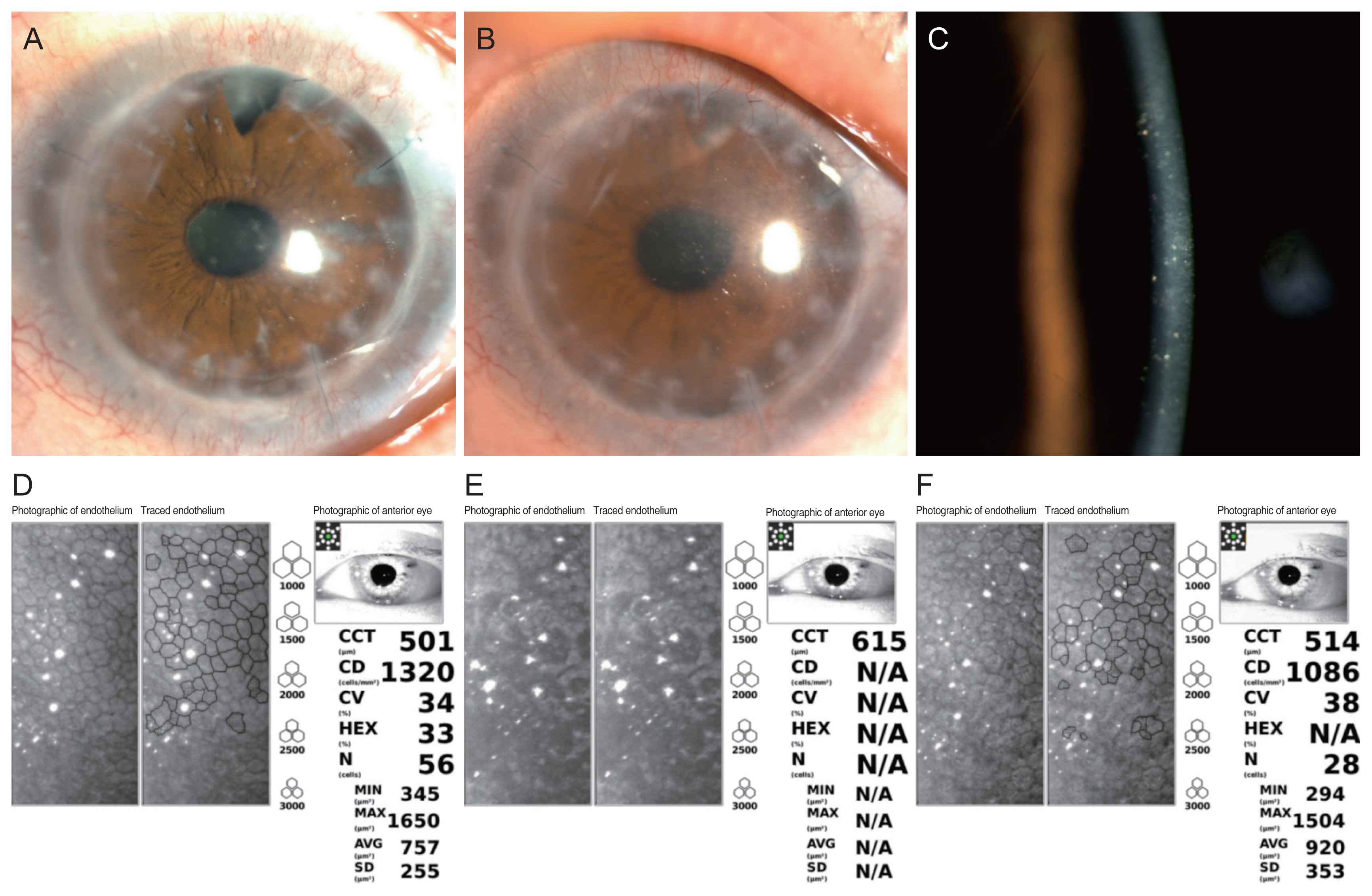
A 64-year-old male patient had a history (2000 and 2017) of undergoing penetrating keratoplasty (PKP) for corneal opacity in his right and left eyes, respectively. In 2019, another PKP had been performed in his left eye due to graft rejection, which reoccurred 3 months after. Therefore, in 2020, he underwent Descemet stripping automated endothelial keratoplasty (DSAEK) and maintained a clear grafted cornea for 1 year (Fig. 1A).
In May 2021, he received the first dose of the ChAdOx1 vaccine. After 3 hours, he experienced a pressing sensation in the left eye; 2 days later, he experienced blurred vision. At presentation, the uncorrected visual acuity was 20 / 50 and the intraocular pressure was 13 mmHg, unchanged compared with 6 months ago. Slit-lamp examination revealed slight conjunctival injection with mild corneal edema. Fine keratic precipitates were found in the central cornea, and a trace anterior chamber reaction was observed (Fig. 1B, 1C). Central corneal thickness had increased from 563 to 615 ╬╝m. The number of corneal endothelial cells and their degree of hexagonality decreased (Fig. 1D, 1E). The patient was diagnosed with graft rejection and treated with hourly administration of topical and systemic steroid. Three days later, the symptoms and signs of inflammation resolved, and central corneal thickness decreased to 537 ╬╝m. Steroid doses were tapered gradually, and there were no inflammation signs at the 3-month follow-up. However, the corneal endothelial cell count remained lower than on the previous specular microscopy before the rejection (Fig. 1F). No additional signs of graft rejection were observed after received a second dose.
This is the first case report of graft rejection after SARS-CoV-2 vaccination in South Korea. There have been three reports of graft rejection in patients after BNT162b2 vaccination. Phylactou et al. [1] reported two cases of graft rejection after BNT162b2 vaccination in patients who underwent DescemetŌĆÖs membrane endothelial keratoplasty. The rejection occurred a week after the first dose in one case and 3 weeks after the second dose in the other. Wasser et al. [2] reported two cases of graft rejection 2 weeks after the first dose in patients who had undergone a PKP. Abousy et al. [3] reported one case of bilateral graft rejection 4 days after receiving the second dose in a patient who underwent DSAEK.
In this case, the patient received the ChAdOx1 vaccine, which uses a chimpanzee adenovirus that carries the SARS-CoV-2 spike protein. Although the exact mechanism underlying graft rejection following the vaccination is unclear, an immunologic response following seroconversion could be a possible cause [1]. Positive anti-spike immunoglobulin G can be developed over 2 to 4 weeks following SARS-CoV-2 vaccination. All previous cases occurred 4 days to 3 weeks after vaccination, corresponding to the seroconversion period.
While there is no definite proof of causation, factors suggestive of a possible causal relationship include the temporal association following vaccination. Here, graft rejection occurred 2 days after SARS-CoV-2 vaccination. After BNT162b2 vaccination, systemic side effects were more commonly reported after the second dose [4]. After ChAdOx1 vaccination, the rate of adverse events after the first dose was relatively higher [5]. Phylactou et al. [1] reported a case of graft rejection after the second BNT162b2 dose. Here, rejection occurred after the first ChAdOx1 dose.
Though vaccination increases the systemic immune reaction, only the left eye was involved in our case. Anterior chamber immunological privilege can be violated after multiple PKP procedures because the anterior chamber can be more responsive to an immune reaction after vaccination. Patients with graft rejection following vaccination respond well to steroids. In our case, the symptoms and signs resolved within 3 days of treatment. However, corneal endothelial cell loss was inevitable after rejection.
Patients should be aware of the possible correlation between SARS-CoV vaccination and graft rejection. Ophthalmologists should pay close attention to symptoms within 2 to 4 weeks of vaccination. Early identification and management are important because graft rejection is potentially reversible.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






