Thin but Nonkeratoconic Cornea: A Case Report
Article information
Dear Editor,
The cornea is composed of five layers: epithelium, Bowman layer, stroma, Descemet membrane, and endothelium. In addition to healthy layers, it is also important to maintain necessary layer thickness to assure integrity and function. In previous studies, central corneal thickness less than 500 μm was regarded as clinically thin and was observed in a subpopulation of healthy young adults [1]. Central corneal thickness less than 480 μm is regarded as extremely thin cornea and is highly suggestive for keratoconic or ectasic cornea [2]. But standard measurement or thickness to diagnosis thin cornea remain debated [3]. Here, we introduce a case of extremely thin cornea, less than 400 μm, that was nonkeratoconic. The patient provided written informed consent for publication of her examination results and images.
A 26-year-old female patient first visited Severance Hospital for refractive surgery evaluation. She had no previous systemic or ocular disease. Also, she had no family history for ocular disorder within three generations of her family. She has worn soft contact lenses about two or three times per week for 10 years but had stopped using them for 2 weeks before the examinations.
The best-corrected distant visual acuities were 20 / 20 in both eyes. The manifest refraction was −5.50 Sphere −2.50 Cylinder × 180° in the right eye and −7.00 Sphere −2.00 Cylinder × 180° in the left eye. Fig. 1A–1H show the images of both eyes. The slit-lamp examination (Fig. 1A, 1E) for both eyes did show thin cornea without any other sign suggesting hypoxia or mechanical trauma on cornea. Fundus examination for both eyes also showed no remarkable sign.
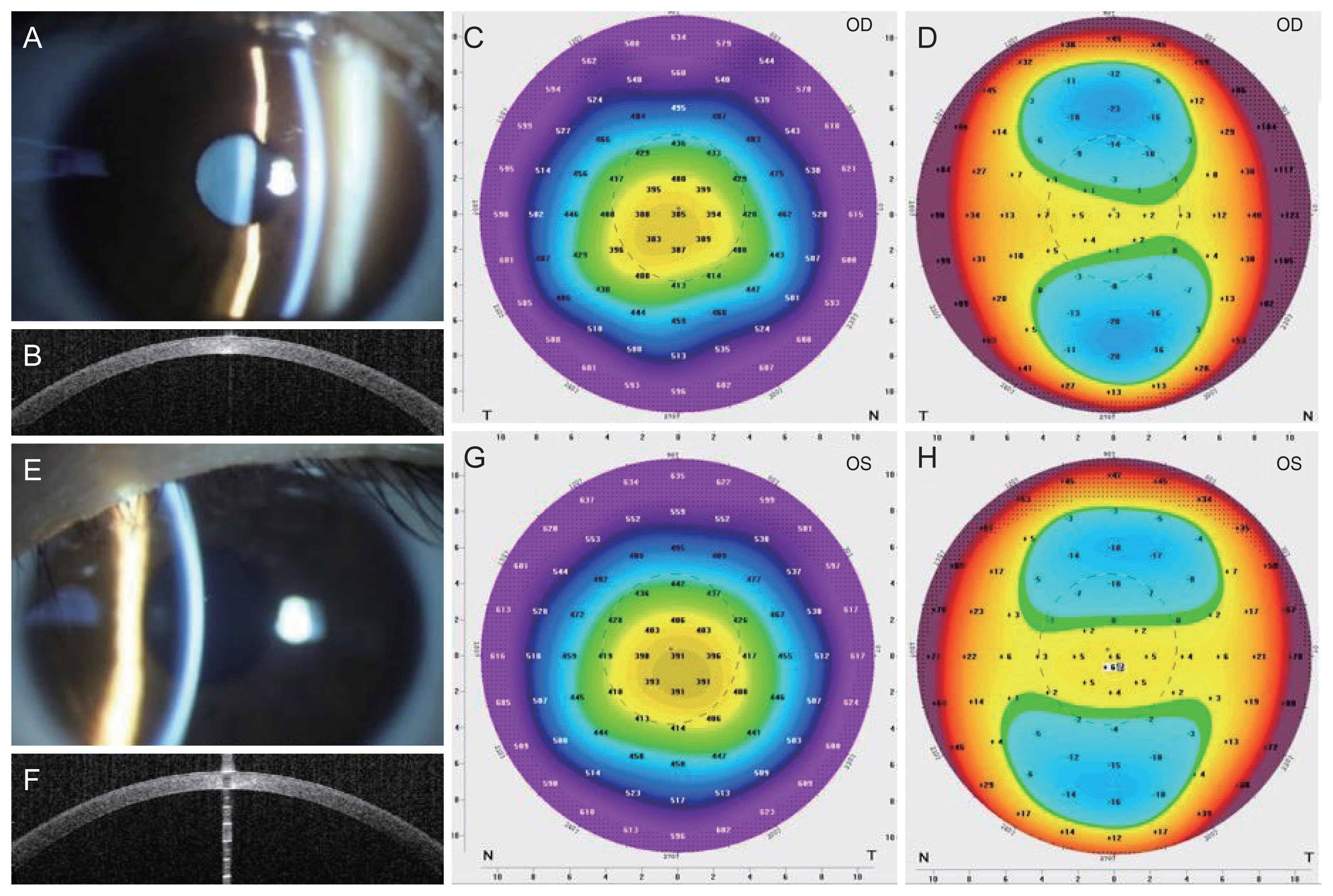
Images of (A–D) the right eye (OD) and (E–H) the left eye (OS). (A,E) Cornea slit examination, (B,F) the anterior segment optical coherence tomography, and (C,G) thickness map and (D,H) elevation map of Scheimpflug tomography. All images show thin cornea throughout the whole diameter. N = nasal; T = temporal.
Corneal thickness measured with Scheimpflug tomography (Pentacam; Oculus, Wetzlar, Germany) was 383 μm at the thinnest point, 385 μm for the corneal apex of the right eye, 389 μm at the thinnest point, and 391 μm for the corneal apex of the left eye. Topography with placido-scanning-slit system (ORBscan II; Bausch & Lomb, Rochester, NY, USA), noncontact tono-pachymetry (NT-530P; Nidek, Gamagori, Japan), and specular microscope (EM-4000; Tomey, Nagoya, Japan) also showed central corneal thickness less than 400 μm, about 10% difference among measuring methods.
Elevation and curvature maps of both eyes showed symmetric bow-tie pattern with-the-rule topography (Fig. 1D, 1H). In sagittal curvature map, inferior-superior asymmetry index was 1.0 for each eye, regarded as normal. Indices representing irregularity of cornea curvature, index of surface variance, index of vertical asymmetry, keratoconus index, central keratoconus index, index of height asymmetry, index of height decentration, and the smallest radius of sagittal/axial corneal curvature were all within normal range.
The Belin/Ambrósio enhanced ectasia display (BAD) showed no significant elevation from a reference surface. The corneal thickness spatial profile curve showed progressive thickening of the cornea from the thinnest point to the periphery, without breakaway, following the thinnest line. However, the final BAD score, denoted as a deviation (D) value, was 3.61 for the right eye and 3.39 for the left eye, red colored, larger than 2.6 standard deviations from the mean, largely resulting from the standard deviation of corneal thickness at the thinnest point from the mean of the normative database [4].
Other than thin cornea, her both eyes showed normal corneal characteristics. Anterior segment optical coherence tomography (CASIA SS-1000, Tomey) also showed well-organized layers of the cornea without any defect or abnormal infiltration. In addition, specular microscopy showed endothelial cell density 2,728 cells/mm2 for the right eye and 2,681 cells/mm2 for the left eye with no definite sign of endothelial cell dysfunction. With the development of refractive surgery, long-term efficacy and safety of refractive surgery for thin cornea have been improved [5]. Still, preoperative corneal thickness is one of the most important factors for determining candidate of corneal refractive surgery due to its risk for developing corneal ectasia after corneal refractive surgery. We did not recommend refractive surgery involving corneal surface ablation due to her thin cornea.
To conclude, we report a case of extremely thin cornea of a healthy Korean female patient without any pathologic change in either eye. Regardless of its extreme thinness, the cornea showed normal topographical structure and function.
Acknowledgements
None.
Notes
Conflicts of Interest: Tae-im Kim is a member of the Editorial Board of the Korean Journal of Ophthalmology since 2020. However, she was not involved in the peer reviewer selection, evaluation, or decision process of this article. Otherwise, no other potential conflicts of interest relevant to this article were reported.
Funding: None.