Rhegmatogenous Retinal Detachment in Waardenburg Syndrome: A Case Report
Article information
Dear Editor
Waardenburg syndrome (WS) is a rare auditory-pigmentary disorder and characterized by sensorineural hearing loss, pigmentary disturbances of the skin, hair, iris, and choroid [1]. WS is caused by mutations of several genes that affect the division and migration of neural crest cells (NCCs) during embryonic development. Rhegmatogenous retinal detachment (RRD) in WS has been rarely discussed in the literature. Herein, we report an extremely rare case of RRD in a patient with WS who was successfully treated with surgical management. Written informed consent was obtained from the patient
A 24-year-old male patient diagnosed with WS was referred to Seoul National University Hospital with decreased visual acuity in his left eye (OS). On general examination, he had grey hair and skin hypopigmentation. He also had a cochlear implant because of congenital sensorineural hearing impairment. Genetic analysis revealed heterozygous pathogenic variant c.649_651del (p.Arg-217del) of the MITF gene, confirming a diagnosis of WS type 2A. He had no history of ocular trauma or atopic dermatitis. His best-corrected visual acuity (BCVA) were 20 / 32 in the right eye (OD) and hand motion OS. The spherical equivalents were −6.88 diopters (D) OD and −4.63 D OS, and axial lengths were 26.89 mm OD and 23.44 mm OS. Slit-lamp examination showed heterochromia with blue iris (Fig. 1A). The right fundus revealed diffuse choroidal hypopigmentation and multiple choroidal pigmentation (Fig. 1B). On fluorescein angiography, blocked hypofluorescence corresponded to areas of choroidal hypopigmentation was noted (Fig. 1C). The left fundus demonstrates bullous, nearly total RRD (Fig. 1D). Because of poor mydriasis and choroidal hypopigmentation, no retinal break could be determined. Optical coherence tomography (OCT) showed foveal hypoplasia with macula-off RRD (Fig. 1E). The patient underwent a pars plana vitrectomy with silicone oil (SO) tamponade. During the surgery, retinal breaks were identified at 2 and 9 o’clock in the peripheral retina.
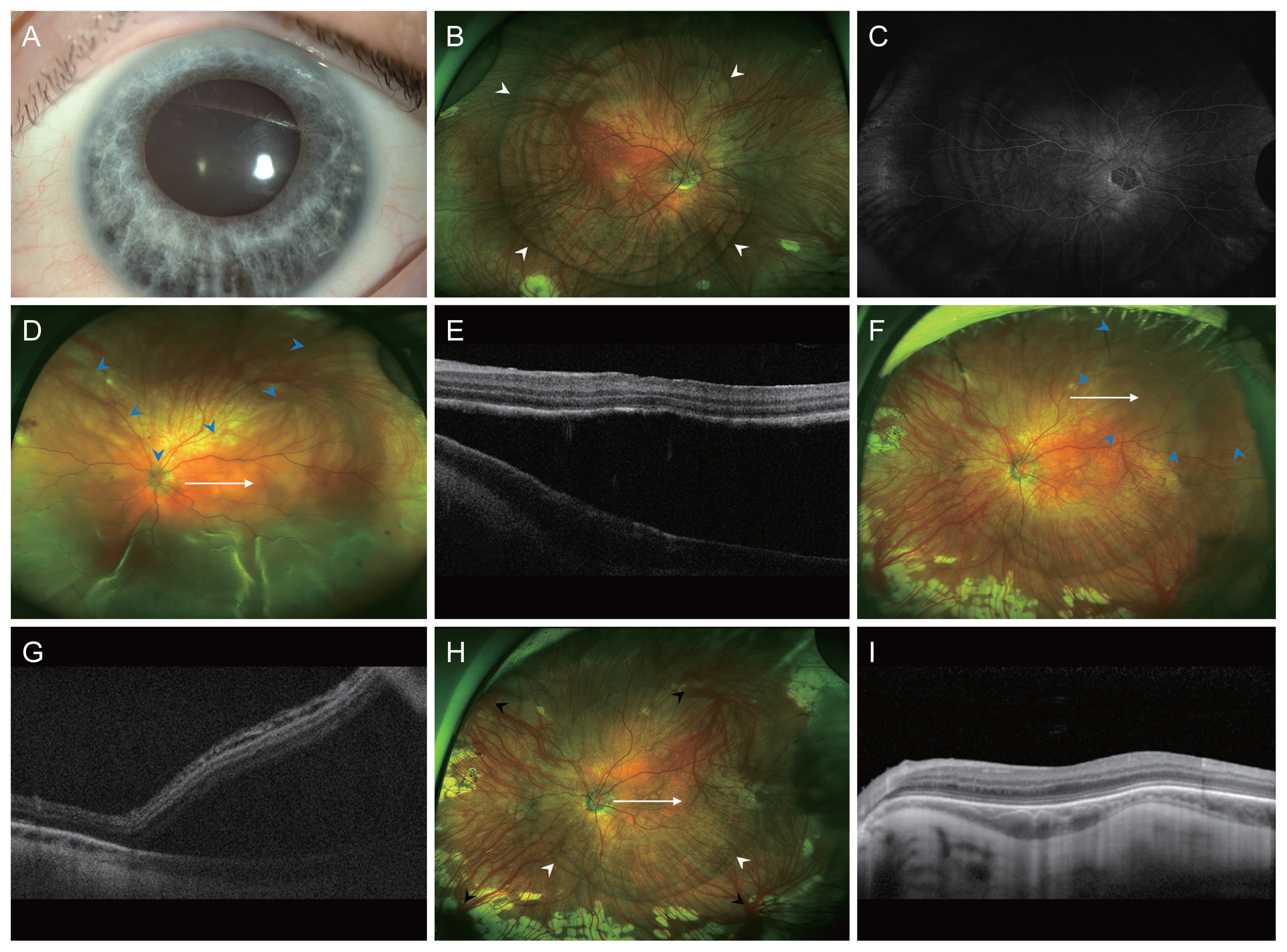
Images of patient with Waardenburg syndrome. (A) Anterior segment photograph revealing heterochromia with blue iris in diffuse pattern. (B) Widefield fundus photography demonstrating choroidal hypopigmentation with multiple concentric ring-shaped choroidal pigmentation (white arrowheads) in the right eye. (C) Widefield fluorescein angiography reveals mild transmitted hyperfluorescence and blocked hypofluorescence corresponded to areas of choroidal hypopigmentation. (D) Widefield fundus photography and (E) horizontal optical coherence tomography (OCT) scan of the corresponding area (white arrow) of left eye shows bullous rhegmatogenous retinal detachment (blue arrowheads) at initial presentation. (F) Widefield fundus photography and (G) OCT scan of the corresponding areas (white arrow) reveals localized retinal detachment (blue arrowheads) at the time of recurrence. (H) Widefield fundus photography and (I) OCT of left eye at final visit demonstrating reattached retina. Note diffuse choroidal hypopigmentation with multiple concentric ring-shaped choroidal pigmentation (white arrowheads) and prominent vortex veins (black arrowheads). OCT shows foveal hypoplasia with irregular bowing out of the choroidal-scleral interface.
One year after surgery, the BCVA was 20 / 40 OS, and the retina was completely flat. Accordingly, SO was removed and cataract surgery was performed during vitrectomy. After SO removal, the retina remained flat during the 23 months of follow-up. Two years after SO removal, he had sudden reduction of visual fields. His BCVA was 20 / 50 OS and fundus examination revealed recurred RRD in the superotemporal retina (Fig. 1F, 1G). He underwent repeated vitrectomy with gas tamponade (sulfur hexafluoride [SF6], 20%). Intraoperatively, a new retinal break was identified at 2 o’clock. After surgery, the retina was entirely flat. At the last visit, 6.5 years after the surgery, his BCVA was 20 / 40 OS, and the patient had no recurrence of RRD. Fundoscopy demonstrated diffuse choroidal hypopigmentation with multiple ring-shaped choroidal pigmentation in the left eye (Fig. 1H). OCT showed foveal hypoplasia and irregular bowing out of the choroidal-scleral interface (Fig. 1I).
To the best of our knowledge, this is the first case of RRD in a patient with WS. WS is caused by variants in the EDN3, EDNRB, MITF, PAX3, SNAI2, and SOX10 genes which results in defective neural crest development and melanocyte migration [2]. During embryonic development, NCCs infiltrate the iris to provide its pigmentation and also differentiate into the pericytes of the choroid, as well as the sclera [3]. It is reasonable to speculate that choroidal concentric pigmentation, foveal hypoplasia, and irregular bowing out of the choroidal-scleral interface may be attributable to the defective melanocyte migration and developmental anomaly of embryogenesis derived from NCCs. However, it remains unclear whether the relationship between WS and RRD is causal or coincidental as of now.
The diagnosis and treatment of RRD in WS are challenging. There is difficulty in finding the retinal breaks from hypopigmented choroid. The lack of pigment causing difficulties with efficient visualization of laser burn and lack of coagulation and adhesive effect could be another challenge. Cryopexy may be needed if the visible laser marks could not be achieved even after increasing the power and duration of laser [4]. Although there was one recurrence of RRD after SO removal in this case, proliferative vitreoretinopathy did not develop, and successful reattachment was achieved with reoperation. Lack of pigmented cells had been suggested to cause reduced incidence of proliferative vitreoretinopathy in these patients [5].
In conclusion, we report a rare case of RRD in a patient with WS. Even though the diagnosis and treatment of RRD can be challenging, vitrectomy appears to be a good surgical technique in this patient population.
Acknowledgements
None.
Notes
Conflicts of Interest: None.
Funding: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (the Ministry of Science and ICT) (No. NRF-2021R1F1A1045417).