 |
 |
| Korean J Ophthalmol > Volume 36(4); 2022 > Article |
|
Abstract
Purpose
We investigated the association between the level of control and exodeviation after the monocular occlusion test (MO) in pediatric patients with intermittent exotropia.
Methods
We retrospectively reviewed the records of pediatric patients with intermittent exotropia who visited Yeungnam University Hospital between September 2015 and December 2020. The largest exodeviation obtained before and after 1 hour of MO were compared. The LACTOSE (Look And Cover, then Ten seconds of Observation Scale for Exotropia) control scoring system was used to measure the level of control. Controllability was defined when the patient had the subjective awareness of exotropia and the instinctive ability to correct ocular deviation.
Results
Five hundred and three consecutive patients (260 male and 243 female patients; mean age, 7.8 years) were included. In all control scores, exodeviation significantly increased after the MO (p < 0.001). However, the patients with an increase in exodeviation Ōēź5 prism diopters (PD) after the test did not show any significant association with the control scores. The presence of controllability was significantly associated with an increase of Ōēź5 PD at near (p = 0.034).
Conclusions
Exodeviation showed significant increase after the MO, regardless of the level of control, in pediatric patients with intermittent exotropia. There was no significant association between the control scores and an increase of Ōēź5 PD after the MO. Patients with controllability were more likely to show increase in exodeviation after the MO.
The monocular occlusion test (MO) is a diagnostic method to measure largest exodeviation in patients with intermittent exotropia [1-3]. It involves placing an occlusive patch over one eye for 30 to 60 minutes, followed by measuring the deviation without letting the patient restore binocular fusion [2]. The idea is to totally suspend all tonic fusional convergence by occluding one eye, forcing the full latent deviation to manifest. The largest ocular deviation is usually the target of surgery in patients with intermittent exotropia. Therefore, MO may aid in the planning of appropriate surgical strategy for a favorable surgical outcome [1-3].
The level of control is associated with fusional capacity and variability in the exodeviation of patients with intermittent exotropia [3]. The level of control in patients with intermittent exotropia can be affected by several factors including general health, alertness, attention span, and level of anxiety [1,4]. The results of the MO may be affected by and differ according to the level of control [3]. To the best of our knowledge, no previous studies have investigated the association between results of the MO and the level of control in pediatric patients with intermittent exotropia. Accordingly, we investigated the changes in exodeviation after the MO in pediatric patients with intermittent exotropia and their association with the level of control.
This study was approved by the Institutional Review Board of Yeungnam University Hospital (No. 2019-12-038), which waived the requirement for informed consent owing to the retrospective nature of the study and the use of anonymized patient data. We retrospectively reviewed the medical records of pediatric patients (aged <18 years) with intermittent exotropia who visited Yeungnam University Hospital between September 2015 and December 2020. Only the basic type of intermittent exotropia with the distance deviation is within 10 prism diopters (PD) of the near deviation was included in this study. Patients with any other types of strabismus such as oblique muscle dysfunction, dissociated vertical deviation, A-V pattern, and nystagmus were excluded from this study. Patients with previous intraocular surgery, any neurological impairment such as cerebral palsy, or unilateral amblyopia were also excluded.
All patients underwent complete ophthalmologic examinations at their first visit. The angles of deviation were measured by the prism and alternate cover test at distance (6 m) and near (33 cm), using accommodative targets. The occlusive patch was provided to all patients at the first visit. All patients were informed that we planned to occlude the nondominant eye for 1 hour at the next visit to measure the largest exodeviation. A Ōēź5 PD increase of exodeviation after the MO was considered a clinically significant increase. All measurements of ocular deviation were performed by one clinician (WJK). The level of control was measured using the LACTOSE (Look And Cover, then Ten seconds of Observation Scale for Exotropia) control scoring system, which evaluates both distant and near control (5-point scales, range 0-4 for each), making total scores of 0 to 8. Higher control scores were indicative of poorer level of control [5]. Controllability was defined when patient had the subjective awareness of exotropia and instinctive ability to correct ocular deviation. The stereoacuity test was conducted using the Lang I test (Lang-Stereotest AG, Kusnacht, Switzerland) and Stereo Fly Stereotest (Stereo Optical, Chicago, IL, USA).
Statistical analyses were performed using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). The paired t-test was used to evaluate the differences within each group. The largest ocular deviations before and after MO were compared. The unpaired t-test and chi-squared test were used to compare the clinical factors of patients who exhibited a meaningful increase after MO, and others who exhibited no meaningful increase or a decrease in the ocular deviation. The association between clinical factors and a meaningful increase after the MO was evaluated using the logistic regression test. A p-value of less than 0.05 was considered statistically significant.
Five hundred and three consecutive patients (260 male and 243 female patients; mean age, 7.8 years) were included in this study. Basic characteristics of included patients are presented in Table 1. The ocular deviation was 24.0 ┬▒ 6.9 PD (range, 10-50 PD) at distance and 25.1 ┬▒ 7.2 PD (range, 10-55 PD) at near. The level of control was measured for 345 patients. The mean control scores at distance, near, and total were 2.6, 2.1, and 4.7, respectively. The control scores showed a significant association with the results of the Lang I test (p = 0.005 for distant control, p = 0.014 for near control; linear-by-linear association). The number of patients who failed the Lang I test increased in proportion to the increase in the distant and near control scores. The distant control scores were associated with the Stereo Fly Stereotest scores (p = 0.003 at Ōēż400 arc seconds; linear-by-linear association). The near control scores were also associated with the Stereo Fly Stereotest scores, however statistical significance was not obtained (p = 0.064). Among the 503 patients, 97 patients (19.3%) had controllability of exotropia. The mean control scores at distance, near, and total of patients with controllability were 1.8, 1.5, and 3.3, respectively. The control scores in these patients were better than those of patients without controllability (mean distance, near, and total control scores were 2.9, 2.2, and 5.1, respectively; all p < 0.05; unpaired t-test).
The exodeviation at distance increased significantly from 24.0 ┬▒ 6.9 to 26.4 ┬▒ 7.1 PD after MO ( p < 0.001, paired t-test). The exodeviation at near increased significantly from 25.1 ┬▒ 7.2 to 30.3 ┬▒ 7.4 PD after MO (p < 0.001). The mean change in exodeviation after MO was 2.3┬▒4.4 PD (range, 17-22 PD) at distance and 5.2┬▒6.0 PD (range, 17-30 PD) at near. The largest increase of exodeviation after MO was 22 PD at distance and 30 PD at near. Fig. 1A, 1B shows the distribution of percentage of patients according to amount of change in exodeviation after the MO. Of the 503 patients, 186 patients (37.0%) exhibited a meaningful increase at distance, and 321 patients (63.8%) exhibited a meaningful increase at near.
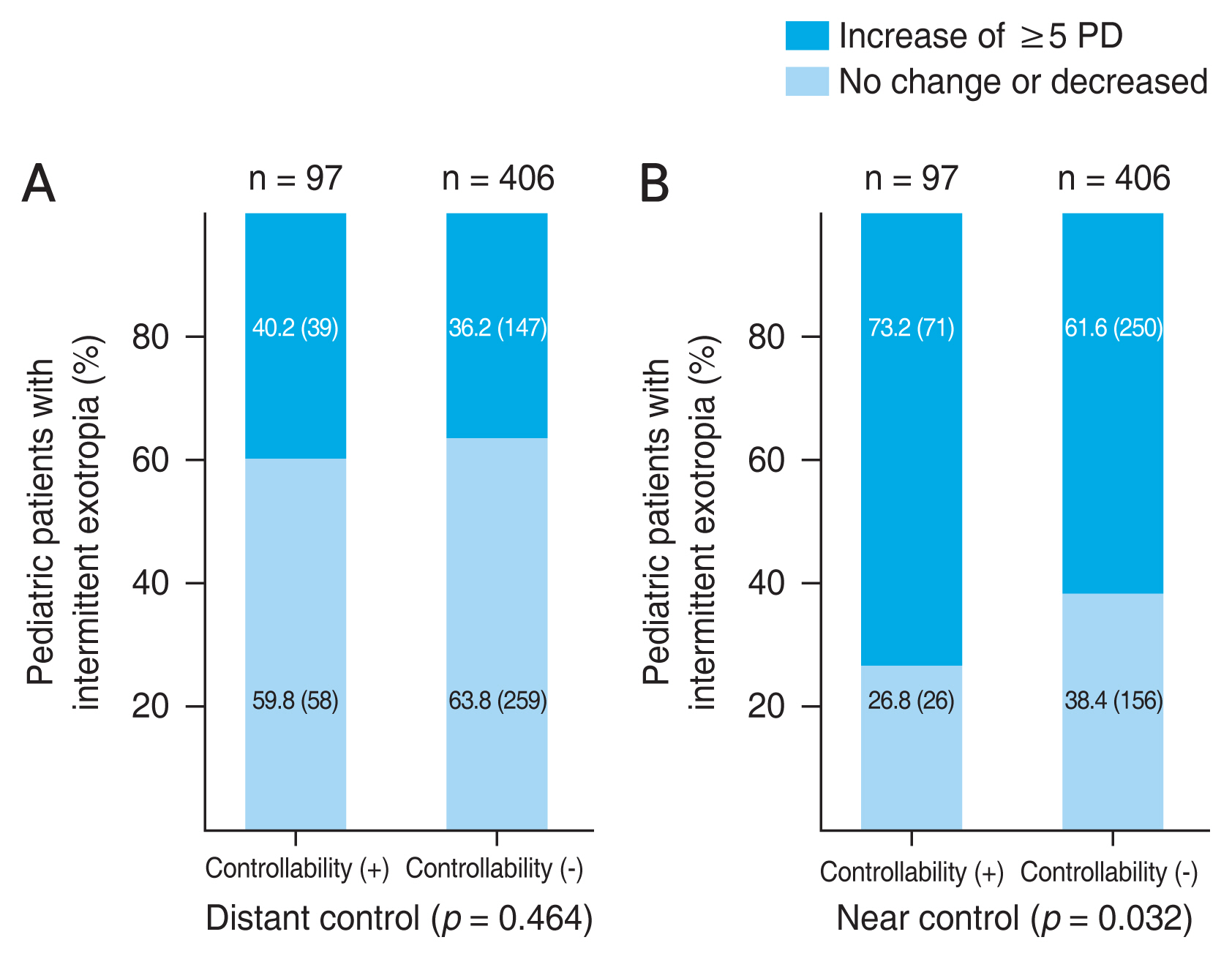
We analyzed the association between the change in exodeviation after the MO and the level of control. In all control scores, the amount of ocular deviation at both distance and near showed a significant increase after the MO in pediatric patients with intermittent exotropia ( p < 0.001, paired t-test) (Fig. 2A, 2B). The percentages of patients with a meaningful increase after the MO rose with the fall in the control scores, however failed to achieve statistical significance (p = 0.773 for distant control, p=0.082 for near control; chi-square test) (Fig. 3A, 3B). The percentage of patients with a meaningful increase at near after the MO significantly increased with the presence of controllability (p = 0.032, chi-square test) (Fig. 4A, 4B). Other clinical factors including mean age at the onset of exotropia, sex distribution, and spherical equivalent refractive error did not differ between patients exhibiting a meaningful increase and those with no meaningful changes or a decrease in the ocular deviation (all p > 0.05).
The associations between clinical factors and a meaningful increase after MO were analyzed using the logistic regression test. The presence of controllability was also significantly associated with a meaningful increase at near (odds ratio, 1.704; 95% confidence interval, 1.042-2.786; p = 0.034 for a presence of controllability). The patients with controllability are more likely to show a meaningful increase at near after MO. No clinical factor was associated with a meaningful increase after the MO (all p > 0.05).
Exodeviation showed a significant increase after MO, regardless of the level of control, in pediatric patients with intermittent exotropia. The control scores did not show a significant association with a meaningful increase after MO. The patients with controllability were more likely to show an increase in ocular deviation after MO.
For patients with intermittent exotropia undergoing surgery, the surgery should be performed for the largest deviation measured [6]. Patients with intermittent exotropia often show ocular angle variability during follow-up [7]. A previous study found that over half of such patients exhibited variable ocular deviation preoperatively [7]. The MO is a well-known method to reveal the largest angle of ocular deviation in patients with intermittent exotropia [1-3]. The level of control can also vary during the follow-ups and can influence the amount of ocular deviation.
Several clinical scales have been developed for the assessment of level of control, which may be important for the decision regarding the surgery and to confirm the largest deviation for patients with intermittent exotropia [3,5,8]. However, the association between the level of control and effect of the MO has not been evaluated in pediatric patients with intermittent exotropia. If there is a significant association between the results of the MO and the level of control, it may be helpful for clinicians to postulate the change of ocular deviation after the MO based on the level of control and determine the surgical treatment required. Therefore, we investigated the association between the level of control and the change in ocular deviation after the MO.
In this study, pediatric patients with intermittent exotropia exhibited significantly increased exodeviation after the MO regardless of the level of control. The largest increase was 22 PD at distance and 30 PD at near. Even patients with control score 4, which means poor level of control, the largest increase was 15 PD at distance and 21 PD at near. If these differences were not detected before surgical treatment, the surgical outcome would not have been favorable.
Although the amount of ocular deviation significantly increased after the MO for all control scores, the percentage of patients with a meaningful increase after the MO did not show any significant association with the level of control. These results are contrary to the results in adult patients with intermittent exotropia, whose higher degree of near control was found to be significantly associated with an increase of Ōēź5 PD in near fixation after the MO [9]. We considered that the control score may have limitation in reflecting the overall level of control and predicting the effect of MO in pediatric patients with intermittent exotropia. We postulated that these results were caused by the variability in the level of control in pediatric patients rather than by the score system itself. The results of the LACTOSE score system may have a good correlation with the pre-existing stereoacuity test including the Lang I test and Stereo Fly Stereotest. Pediatric patients with intermittent exotropia usually show a better level of control than adults [10]. The study by Jung and Lee [10] reported that the rate of fusion evaluated using the Worth 4-dot test (Flashlight type; Mag instrument, Ontario, CA, USA) at near and distance fixation were higher in pediatric patients than in adults. A better level of control was associated with better fusional capacity and greater variability in the level of control [7,11]. It would be difficult to predict the results of the MO based on the level of control in pediatric patients with intermittent exotropia. The test is noninvasive and relatively short. Therefore, the MO should be performed for all pediatric patients with intermittent exotropia regardless of the control score.
Pediatric patients with controllability were significantly associated with a meaningful increase at near after the MO. Approximately one-fifth of the included patients had controllability and showed a better level of control than patients without controllability. The level of control in patients with intermittent exotropia can be affected by both intrinsic and extrinsic factors [1]. Pediatric patients may be easily frightened during examination at the initial visit. This may increase anxiety, which in turn leads to a temporal increase in the level of control and a decrease in ocular deviation. The level of control in pediatric patients with controllability may be easily affected by intrinsic factors, such as anxiety, and may result in a decrease in ocular deviation at initial examination [4]. Clinicians should be aware of the possibility of hidden ocular deviation, especially in pediatric patients with controllability.
The limitation of this study was that the measurements before and after the MO were not performed on the same day. The MO usually performed within 4 months after initial visit. The level of control may be variable depending on the day [11]. However, the other clinical settings such as examiner, fixation distances, accommodative target size, and room illumination are same in all examinations. The effect of examination performed on the different day may had little influence on the results. In addition, we analyzed the control scores measured at the first visit. Future studies should include serial measurements of level scores.
In conclusion, significant increase of exodeviation after the MO was observed regardless of the level of control in pediatric patients with intermittent exotropia. There was no significant association between the control scores and an increase of Ōēź5 PD after the MO. Patients with controllability were more likely to show increase in exodeviation after the MO.
References
1. von Noorden GK, Campos EC. Binocular vision and ocular motility: theory and management of strabismus. 6th ed. St. Louis: Mosby; 2002.
2. Wright KW, Mocan MC. Exotropia. In: Wright KW, Strube YN, Pediatric ophthalmology and strabismus. 3rd ed. New York: Oxford University Press; 2012. p. 306-16.

3. Kushner BJ. Strabismus: practical pearls you wonŌĆÖt find in textbooks. 1st ed. Cham: Springer; 2017.
4. Lim J, Kim WJ. Dramatic decrease in ocular deviation 1 day before surgery in patients with intermittent exotropia. Korean J Ophthalmol 2020;34:361-6.




5. Kim H, Kim DH, Ahn H, Lim HT. Proposing a new scoring system in intermittent exotropia: towards a better assessment of control. Can J Ophthalmol 2017;52:235-9.


6. Kim WJ, Kim MM. The clinical course of recurrent intermittent exotropia following one or two surgeries over 24 months postoperatively. Eye (Lond) 2014;28:819-24.




7. Kim WJ, Kim MM. Variability of preoperative measurements in intermittent exotropia and its effect on surgical outcome. J AAPOS 2017;21:210-4.


8. Mohney BG, Holmes JM. An office-based scale for assessing control in intermittent exotropia. Strabismus 2006;14:147-50.



9. Shin J, Kim WJ. Changes in exodeviation after the monocular occlusion test in adult patients with intermittent exotropia and its association with the level of control. Korean J Ophthalmol 2020;34:485-90.




Fig.┬Ā1
The distribution percentage of pediatric patients with intermittent exotropia according to the results of the monocular occlusion test. At (A) distant and (B) near. PD = prism diopters.
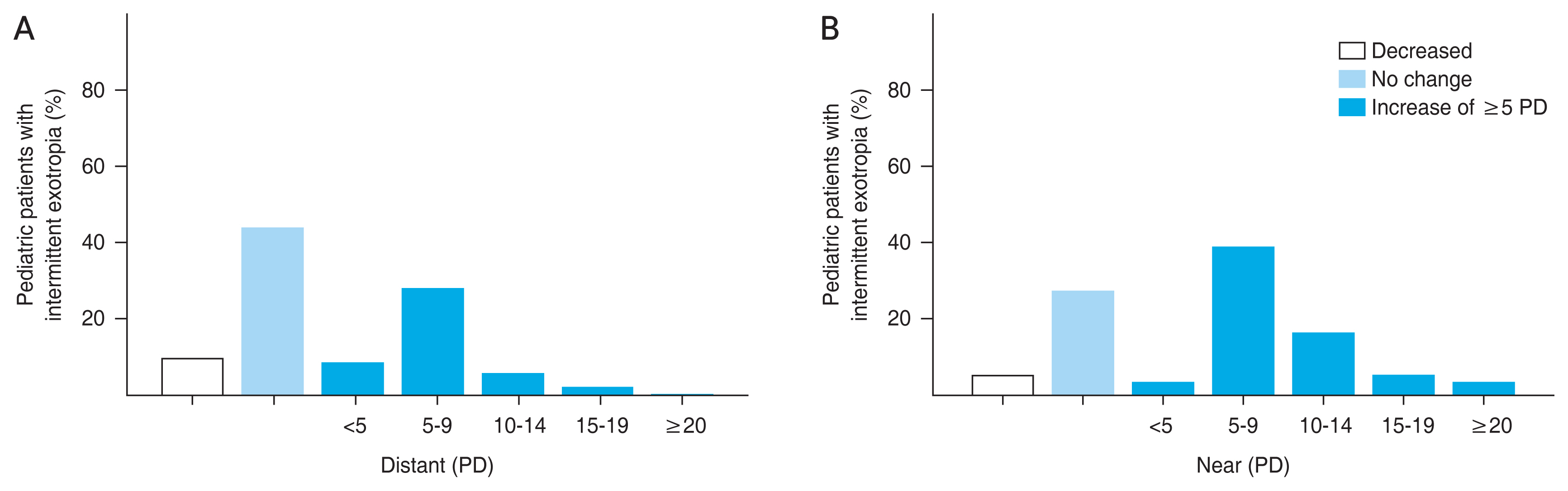
Fig.┬Ā2
The exodeviation after the monocular occlusion test (MO) according to the level of control. In all distant and near control scores, exodeviation significantly increased after the MO. The level of control was measured using the LACTOSE (Look And Cover, then Ten seconds of Observation Scale for Exotropia) control scoring system, which evaluates both distant and near control (5-point scales, range 0-4 for each), making total scores of 0 to 8. Higher control scores were indicative of poorer level of control. At (A) distant control and (B) near control.
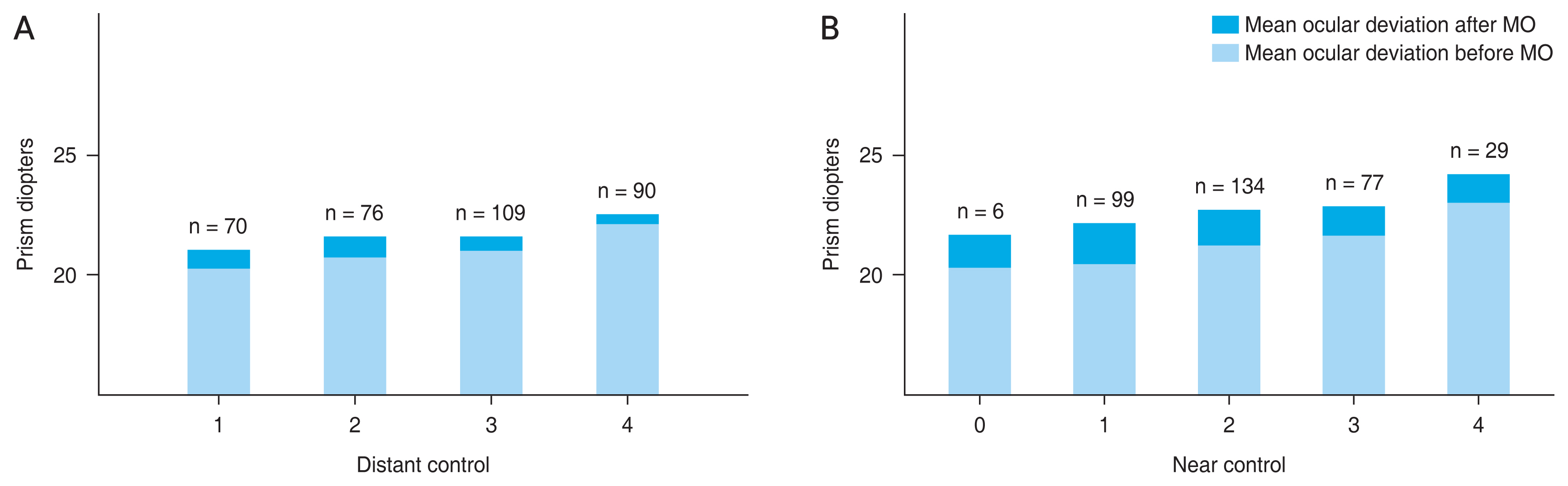
Fig.┬Ā3
The percentage of pediatric patients with intermittent exotropia having an increase of Ōēź5 prism diopters (PD) after the monocular occlusion test (MO) according to the level of control. The level of control was measured using the LACTOSE (Look And Cover, then Ten seconds of Observation Scale for Exotropia) control scoring system, which evaluates both distant and near control (5-point scales, range 0-4 for each), making total scores of 0 to 8. Higher control scores were indicative of poorer level of control. The percentage of patients exhibiting an increase of Ōēź5 PD after the MO at (A) distance and (B) near rose with the fall in the control scores; however, it failed to achieve statistical significance (p = 0.773 for distant control, p = 0.082 for near control; chi-square test).
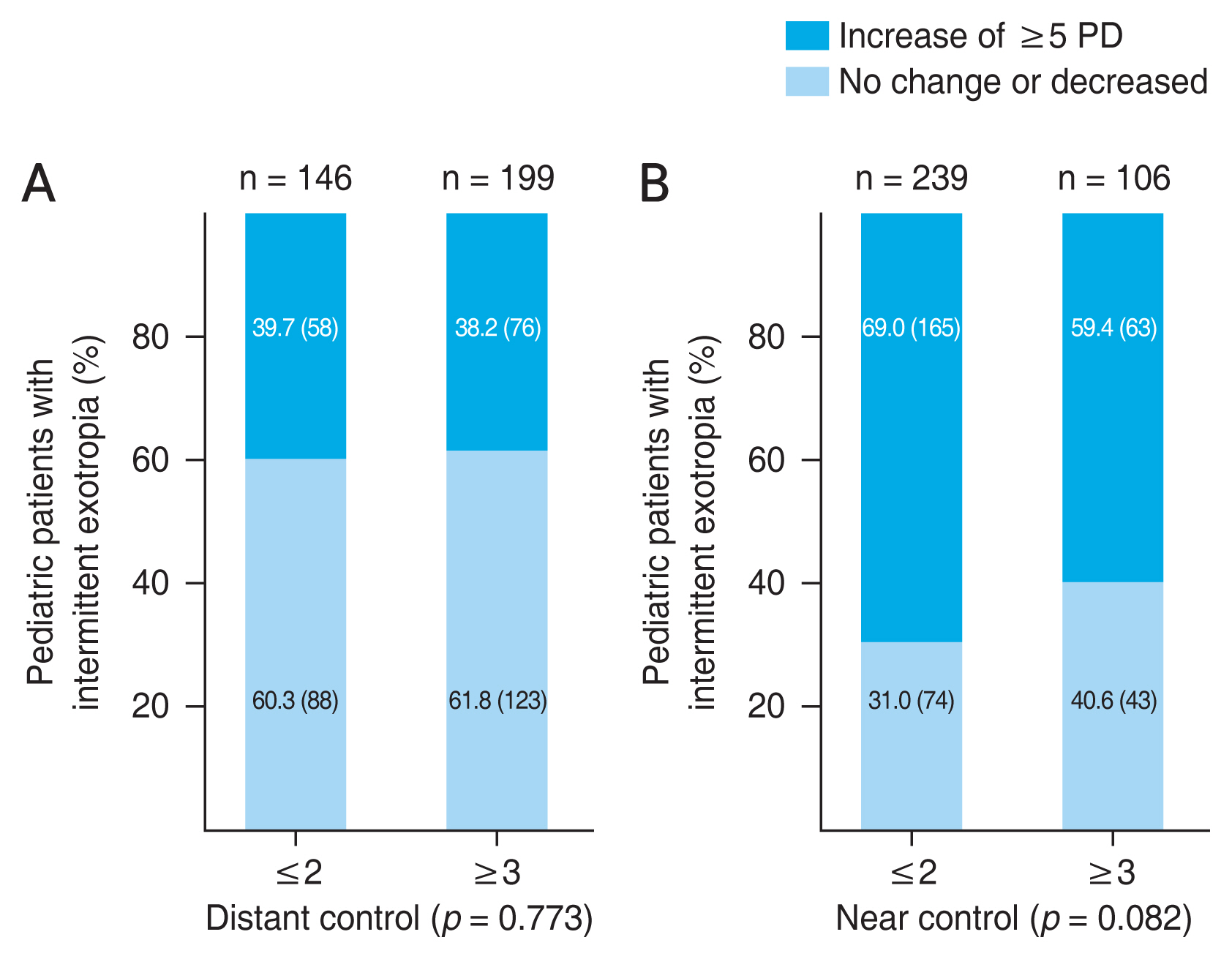
Fig.┬Ā4
The percentage of pediatric patients with intermittent exotropia having an increase of Ōēź5 prism diopters (PD) after the monocular occlusion test according to the presence of controllability. Controllability was defined when patient had subjective awareness of exotropia and ability to correct the ocular deviation instinctively. The percentage of patients with an increase in exodeviation Ōēź5 PD at near after the monocular occlusion test significantly increased with the presence of controllability (p = 0.032 for near control, chi-square test). At (A) distant control and (B) near control.
Table┬Ā1
Basic characteristics of the included pediatric patients with intermittent exotropia (n = 503)
Values are presented as mean ┬▒ standard deviation (range), number, or number (%). The level of control was measured using the LACTOSE (Look And Cover, then Ten seconds of Observation Scale for Exotropia) control scoring system, which evaluates both distant and near control (5-point scales, range 0-4 for each), making total scores of 0 to 8. Higher control scores were indicative of poorer level of control. Controllability was defined when patient had the subjective awareness of exotropia and instinctive ability to correct ocular deviation. The stereoacuity test was conducted using the Lang I test (Lang-Stereotest AG, Kusnacht, Switzerland) and Stereo Fly Stereotest (Stereo Optical, Chicago, IL, USA).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




