 |
 |
| Korean J Ophthalmol > Volume 35(6); 2021 > Article |
|
Abstract
Purpose
This study investigated the efficacy and safety of selective laser trabeculoplasty (SLT) in Korean patients with medically uncontrolled pseudoexfoliation glaucoma (PEXG).
Methods
This retrospective observational study enrolled 43 medically uncontrolled PEXG patients who underwent a 360° SLT and were followed up for at least 12 months after SLT. The intraocular pressure (IOP) before and after SLT at 1 week, 1, 3, 6, and 12 months was evaluated. Treatment success was defined as an IOP reduction of ≥20% from the baseline and an IOP equal to lower than 22 mmHg without additional anti-glaucomatous intervention. Additionally, every follow-up medical record was reviewed to assess any possible side effects of SLT.
Results
Based on the Kaplan-Meier survival analysis, the treatment success rate at 12 months after SLT was 41.9% (18 eyes). For the success group at the 12 months follow-up, SLT showed a mean IOP reduction of 10.3 ± 5.0 mmHg (from 25.6 ± 4.4 to 15.2 ± 2.9 mmHg; 39.3%, p < 0.05). Among the 25 eyes that were considered as the treatment failure group, 14 eyes underwent glaucoma filtering surgeries, four eyes received additional SLT, and further intervention and follow-up was refused for seven eyes. During the overall follow-up period, there were no significant adverse events.
Intraocular pressure (IOP) seems to be the only modifiable risk factor in the development and progression of glaucoma. Therefore, lowering the IOP is currently the standard treatment in the management of glaucoma [1]. Selective laser trabeculoplasty (SLT) uses a 532-nm Q-switched, frequency-doubled Nd:YAG laser with nanosecond pulse duration, which selectively targets the pigmented trabecular meshwork without collateral thermal damage to the adjacent non-pigmented trabecular meshwork and underlying trabecular beams [2]. Many studies have reported that SLT is an effective therapy for lowering IOP in primary open-angle glaucoma (POAG) and ocular hypertension [3-7].
Pseudoexfoliation syndrome is a known significant risk factor for glaucoma, and several studies reported that pseudoexfoliation glaucoma (PEXG) is a common form of secondary open-angle glaucoma [8-10]. It has worse IOP characteristics, resulting in a relatively poor prognosis compared to that of POAG [11-13]. Although there have been several reports that SLT is an effective procedure for lowering the IOP in patients with PEXG [12,14,15], very few studies have reported the treatment outcome of SLT in PEXG patients with uncontrolled IOP despite maximum tolerated medical therapy [15]. Besides, as far as we know, there has never been any research on the IOP-lowering efficacy of SLT exclusively for medically refractory PEXG patients in Korean population. Considering the possible racial difference in the IOP-lowering efficacy of SLT [16], very limited information is available for choosing SLT in Korean medically refractory PEXG patients. The purpose of this study was to investigate the efficacy and safety of SLT in Korean patients with PEXG whose IOP was not adequately controlled with maximum tolerated medical therapy.
This was a retrospective observational study. Eyes with medically uncontrolled PEXG that underwent SLT during the period from February 2012 to August 2017 and met the eligibility criteria were consecutively enrolled from the glaucoma clinic of HanGil Eye Hospital (Incheon, Korea). The study protocol was approved by the institutional review board of HanGil Eye Hospital (Hangil IRB-21002-MI) and the need to obtain informed consent was waived due to the retrospective nature of the study. All study procedures adhered to the tenets of the Declaration of Helsinki.
Patients aged 18 years or older with medically uncontrolled PEXG had to meet the following inclusion criteria: (1) pseudoexfoliative material deposition in the anterior segment, (2) typical glaucomatous optic nerve damage, and compatible visual field defect, and (3) IOP greater than 21 mmHg despite maximum tolerated medical therapy [9,11,16]. Regarding pseudophakic eyes, the following criteria were applied for the diagnosis of pseudoexfoliation. (1) The documentation of pseudoexfoliation syndrome prior to cataract surgery or (2) exfoliation materials were deposited at the pupillary border with pigment loss in the pupillary ruff with or without other characteristic iris changes (i.e., transillumination defects at the iris sphincter region, loss of the pupillary ruff, pigment deposition on the iris surface, and poor and impaired pupillary dilation) [17-19]. In cases where both eyes of a subject were eligible for the study, only one eye was randomly chosen for inclusion.
Eyes with other types of glaucoma, history of other ocular diseases or trauma, intraocular surgery except for uncomplicated cataract extraction, previous laser treatment, and neurologic disease that could affect the visual field were excluded. Patients who could not be followed up for at least 12 months after SLT were also excluded.
We performed SLT with a frequency-doubled Q-switched Nd:YAG laser (Laserex Solo; MedWrench, Brentwood, TN, USA) that delivers a 532-nm wavelength laser light at a pulse duration of 3 ns and a spot size of 400 μm. One drop of 5% proparacaine hydrochloride eye drops was administered before the SLT procedures for anesthesia. A three-mirror Latina SLT Goniolens (Ocular Instruments, Bellevue, WA, USA) was placed on the surface of the eye with 1% methylcellulose. The entire 360° angle was treated. Approximately 100 non-overlapping laser spots were applied over 360° of the trabecular meshwork. To determine the energy level of the SLT for each eye, the laser energy was initially set at 0.6 mJ, and then the energy level was increased by increments of 0.1 mJ until a microcavitation bubble formation was observed. It was also adjusted based on the level of trabecular meshwork pigmentation. The mean energy level used in the present study ranged from 0.6 to 1.0 mJ. No steroids or nonsteroidal anti-inflammatory drugs were used postoperatively.
Prior to the SLT treatment, all patients underwent a complete ophthalmic examination, including measurement of the best-corrected visual acuity (BCVA), IOP by Goldmann applanation tonometry, slit lamp examination, gonioscopy, dilated fundus examination, and standard automated perimetry using the 24-2 Swedish Interactive Thresholding Algorithm program (Humphrey field analyzer II; Carl Zeiss Meditec, Dublin, CA, USA). Within 24 hours after SLT, IOP was measured to detect the IOP spike. Then, patients were followed up at postoperative 1 week and 1, 3, 6, and 12 months after the treatment. At each subsequent follow-up, BCVA measurement, Goldman applanation tonometry, and slit lamp examination were performed. All complications were recorded and treated appropriately. Additionally, ocular medications were reviewed before SLT and at each follow-up. Medication changes were made at the physician’s discretion, considering the target IOP. Significant side effects were defined as IOP spike (when the IOP measured within 24 hours after the procedure increased by more than 5 mmHg compared to the pre-treatment level), hyphema, uveitis, macular edema, or choroidal effusion.
The primary treatment outcome was evaluated by the success rate, which was measured based on the IOP (mmHg) before and after SLT at 1 week, and 1, 3, 6, and 12 months. Success was defined as an IOP reduction of ≥20% from the baseline and an IOP ≤22 mmHg without additional anti-glaucomatous interventions. Failure was defined as an IOP reduction of <20% from the baseline at each visit and/or an IOP >22 mmHg, which required additional treatment. Then, in the case of an adjunctive treatment including systemic medications, repetitive SLT, or filtering surgery, the eye was excluded from further analysis at subsequent follow-up visits. Other outcome measures included changes in the number of IOP-lowering medications and complications.
The efficacy of SLT was assessed by the 12 months survival calculated using Kaplan-Meier survival analysis. Student’s t-test for paired data was used to evaluate the changes in IOP and number of medications at each follow-up visit from the baseline values. To compare the differences in clinical parameters measured at baseline between the success and failure groups, the Mann-Whitney test and chi-square test were used, whenever appropriate. Differences in continuous variables including age, baseline IOP, and visual field mean deviation (MD) were calculated using the Mann-Whitney test. For the comparisons of categorical variables including sex and lens status, the chi-square test was used for the analysis. In addition, we performed univariate and multivariate Cox regression analyses to assess the baseline factors associated with treatment failure. Multiple regression analysis with a backward stepwise variable selection was also performed to investigate the baseline factors that influence IOP reduction following SLT in the treatment success group. All statistical analyses were performed using IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA). A p-value of less than 0.05 was considered statistically significant.
Forty-three eyes of 43 patients (24 males and 19 females) who met the eligibility criteria were consecutively enrolled in the study. The mean age of the study subjects was 74.2 ± 8.2 years. The mean baseline IOP was 26.7 ± 5.8 mmHg and the mean number of IOP-lowering medications was 3.7 ± 0.8. The mean BCVA was 0.25 ± 0.3 logarithm of the minimum angle of resolution and spherical equivalents was −0.25 ± 1.4 diopters. For the baseline visual field parameter, the MD was −18.2 ± 9.2 dB and pattern standard deviation (PSD) was 8.2 ± 4.0 dB (Table 1).
Regular follow-ups were performed after 1 week, 1, 3, 6, and 12 months after SLT. The mean IOP of enrolled patients at each time point of 1 week, 1, 3, 6, and 12 months after SLT were 15.7 ± 3.8, 16.4 ± 3.5, 15.8 ± 2.8, 16.8 ± 3.4, and 15.2 ± 2.9 mmHg, respectively, and all the mean IOP at each time periods after SLT were significantly lower than the baseline IOP (all p < 0.05) (Table 2). Additionally, during the entire follow-up period, there was no serious adverse event following SLT.
According to the Kaplan-Meier survival analysis, the success group at 12 months after SLT included 18 eyes of 18 patients, and the success rate was 41.9% (Fig. 1). The failure group comprised 25 eyes of 25 patients. Among them, 14 eyes underwent filtering surgeries, while four eyes underwent repeated SLT treatment. However, further treatment for the other seven eyes was denied due to old age and poor general conditions. One eye of four eyes retreated by SLT underwent filtering surgery at 13 months after retreatment.
The mean baseline IOP of the treatment success group (n = 18) was 25.6 ± 4.4 mmHg, and the mean IOP following SLT were 15.8 ± 4.2 mmHg at 1 week, 16.3 ± 3.0 mmHg at 1 month, 14.7 ± 2.2 mmHg at 3 months, 15.6 ± 2.9 mmHg at 6 months, and 15.2 ± 2.9 mmHg at 12 months, respectively. The mean IOP at each time period in the success group was significantly lower than the baseline IOP (all p < 0.05) (Fig. 2).
There were no significant differences in age, sex ratio, BCVA, spherical equivalents, or lens status between the success and failure groups (all p > 0.05). The failure group (27.4 ± 5.9 mmHg) showed a higher mean baseline IOP than the success group (25.6 ± 4.4 mmHg); however, there was no significant difference between the two groups (p = 0.128). As for the baseline visual field parameters, there were no significant differences in MD (success group, −17.2 ± 9.9 dB; failure group, −19.0 ± 8.9 dB) and PSD (success group, 8.1 ± 4.9 dB; failure group, 8.2 ± 3.3 dB) (both p > 0.05) (Table 3). As a result of Cox regression analysis to investigate the factors affecting treatment failure, there was no statistically significant association between treatment failure and the following baseline factors: age, sex, BCVA, spherical equivalents, phakic status, number of medications, MD, and baseline IOP.
A multiple regression analysis was performed to assess the baseline factors that affect the IOP reduction in the treatment success group, including that of various possible parameters (age, BCVA, spherical equivalents, baseline IOP, number of medications, MD, and PSD). The baseline IOP was the only parameter that was associated with IOP reduction after SLT (Ɓ = 0.791, R2 = 0.719, p < 0.001), and was positively correlated with the increment of IOP reduction from baseline at 12 months after SLT (p < 0.001, r = 0.86).
In this study, we investigated the efficacy of SLT in PEXG patients with uncontrolled IOP despite maximally tolerated IOP-lowering medications. Overall, the probability of success in lowering the IOP (>20 % of IOP reduction from baseline and IOP equal to or lower than 22 mmHg) for 12 months was 41.9%, and for the success group, mean IOP reduction at 12 months postoperatively was of 10.3 ± 5.0 mmHg, which corresponded to a 39.3% reduction from the mean baseline IOP. No serious adverse events were observed during the 12 months follow-up after SLT.
In the past two to three decades since it was introduced by Latina and Park [2], SLT has become a feasible and common therapeutic modality in patients with ocular hypertension and open-angle glaucoma due to its favorable IOP-lowering efficacy and excellent safety profiles [20-22]. In addition, in PEXG, several studies have reported that SLT as a primary or adjunctive treatment demonstrated an effective IOP-lowering effect, which was comparable to that in OAG [21,23,24].
Shazly et al. [21] investigated the efficacy of 180° SLT as a primary therapy for 18 eyes with PEXG. In that study, the mean baseline IOP was 25.5 ± 3.4 mmHg, and the authors defined failure as the need for medical, surgical, or further laser treatment or the return of the treated IOP <3 mmHg from the baseline IOP. The cumulative probabilities of success were 83% at 9 to 15 months after SLT and 74% at 30 to 32 months after SLT, respectively. After 30 months of follow-up, the success group showed a mean IOP of 18.3 ± 4.7 mmHg (mean IOP reduction, 5.3 mmHg). We estimated that the cause of the difference in success rates between our study (41.9% at 12months) and this study (83.0% at 9-15 months) is that the criteria for success are stricter in our study (IOP reduction ≥ 20% from baseline and ≤22 mmHg). Besides, the patient group is composed of naïve patients, which differs from patients in our study whose IOP was not controlled even with maximal medical therapy.
In practice, eyes with PEXG often require multiple medications at presentation because of the worse IOP characteristics, substantial IOP fluctuation, and increased optic nerve vulnerability to elevated IOP. In addition, in many cases such as those in our study, it is common that the IOP is not controlled despite maximal medical treatments, requiring additional interventions. Thus, SLT has often been used as an adjunct therapy, and several studies have reported the efficacy of SLT in medically refractory PEXG eyes [6,12,15,25]. Among them, the largest (number of study subjects) study, conducted by Goldenfeld et al. [15], investigated the efficacy and safety of SLT in 57 eyes with uncontrolled IOP (>23 mmHg) on maximal medical therapy. After 12 months of follow up, mean IOP decreased from 26.01 ± 2.5 to 17.8 ± 2.8 mmHg (31.5% IOP reduction). In 88% of patients, IOP was controlled below 21 mmHg and in 66% of patients, IOP was controlled below 18 mmHg at 12 months after SLT. In other words, the 12 months treatment outcome was much better than that of our study. We estimated the reason for the gap as follows: Although the mean baseline IOP was similar between the two studies, our study was conducted on patients with much more advanced visual field defects (mean value of MD, −18.2 dB vs. −8.06 dB), and a larger number of medications (3.7 vs. 2.9) than in the previous study. We assumed that this difference in disease severity might have affected the rate of treatment success.
On the contrary, the study of 20 medically uncontrolled PEXG patients by Miraftabi et al. [25] showed poorer treatment outcomes (i.e., 25% success rate at 12 months after a single session of 360º SLT) than ours (41.9%), even though the baseline IOP (25.7 mmHg) and success criteria (defined as IOP reduction ≥20% from baseline without additional medication) were similar to those of our study and the disease severity of study subjects was mild compared to that of our subjects. The study was conducted on younger patients (mean age of subjects, 68.6 years old vs. 74.2 years old in our study) with less advanced visual field defects (mean value of MD, −3.1 vs. −18.2 dB in our study) and fewer numbers of medications (2.5 vs. 3.7 in our study) compared with our study and even the aforementioned study by Goldenfeld et al. [15]. To assess the exact cause of the difference in the treatment outcome, further studies are needed to determine the influence of disease severity and race on the treatment success of SLT in medically refractory PEXG. In addition, Miki et al. [6] reported a 14.5% success rate (same criteria of success as our study) at 12 months after 360º SLT in 23 medically uncontrolled PEXG patients. Since the above-mentioned study included various types of glaucoma subjects (39 eyes with POAG, 23 eyes with PEXG, and 13 eyes with SOAG), they did not present detailed information on the baseline factors for the PEXG subgroup.
In summary, the treatment outcomes of SLT in previous studies varied and differed from those of our study, even at a similar level of baseline IOP. We hypothesized that the unique characteristics of the patient group in our study, that is, the far advanced stage of visual field defect, use of multiple topical medications, and ethnicity (Korean population) might affect the treatment success rate of SLT. However, in our results, there were no statistically significant baseline factors associated with treatment success/failure after SLT in the Cox regression analysis. Even the baseline IOP, the only known evitable predictor for the treatment success of SLT [26,27], was not statistically significant. We supposed that a rather small number of subjects in our study may have affected the statistical insignificance. Furthermore, previously published data to support this hypothesis are limited. Thus, identifying the exact mechanism requires further investigation in a large population using a prospective controlled design.
Since our study was performed on patients with medically uncontrolled IOP, most of whom showed advanced visual field defects, surgical intervention was required immediately after the initial failure of the SLT. Thus, the natural course of IOP 12 months after SLT cannot be investigated. However, in our results, all the mean IOP at each follow-up was significantly lower than the mean baseline IOP, even if the patients who were just corresponding to the failure at that time (i.e., those who would be excluded from the further analysis) are included. Thus, we supposed that SLT had a certain level of IOP-lowering efficacy based on the IOP result at each follow-up.
In particular, for the 18 patients in the treatment success group, IOP was decreased by approximately 10 mmHg from the initial follow-up, and was maintained at a similar level until 12 months. This result showed that, although not in many, but in some patients, SLT showed effective IOP lowering, and once it responded to the SLT, the effect could be maintained for more than 12 months. Surely, this result does not mean that SLT is the best treatment option for every medically uncontrolled PEXG patient. However, patients with PEXG are relatively older and often have significant systemic disease [28]. Therefore, some of them may not be able to undergo or may have to postpone the filtering surgery because of poor general conditions. In this case, SLT can be considered as a feasible alternative treatment option with an acceptable safety profile, which may help in delaying or even avoiding surgery in some patients.
This study had several limitations. First, the study population was not large. Because PEXG requires a low IOP target due to its characteristics that can progress rapidly in a real clinical setting, many clinicians tend to choose the filtering surgery without trying SLT. Results of other previous studies were not much different from those of our study. Second, due to the limitations of the retrospective design, the adverse events were evaluated only by the medical chart review, and there is a risk that some of them were omitted from the review. In addition, in our review, there were no quantitative gradings for trabecular pigmentation, which might affect the treatment outcome of SLT. To compensate for these limitations, further studies with a prospective well-controlled design, precise protocol for assessing adverse events, and the quantitative grading of trabecular pigmentation in a large number of phakic participants will be needed.
In conclusion, this study demonstrated that SLT in patients with medically uncontrolled PEXG showed excellent safety but limited success for 12 months IOP control. Although it is a part of all patients, in the patients responding to SLT, the IOP-lowering efficacy was significant and stable for 12 months after treatment. Thus, SLT can be considered as one of several options of adjuvant therapy, when medical therapy has failed.
Fig. 1
Kaplan-Meier survival curve plotting the cumulative probabilities against time of 43 pseudoexfoliation glaucoma patients who underwent selective laser trabeculoplasty. Cumulative probability of success after selective laser trabeculoplasty at 12 months was 41.9% (18 eyes).
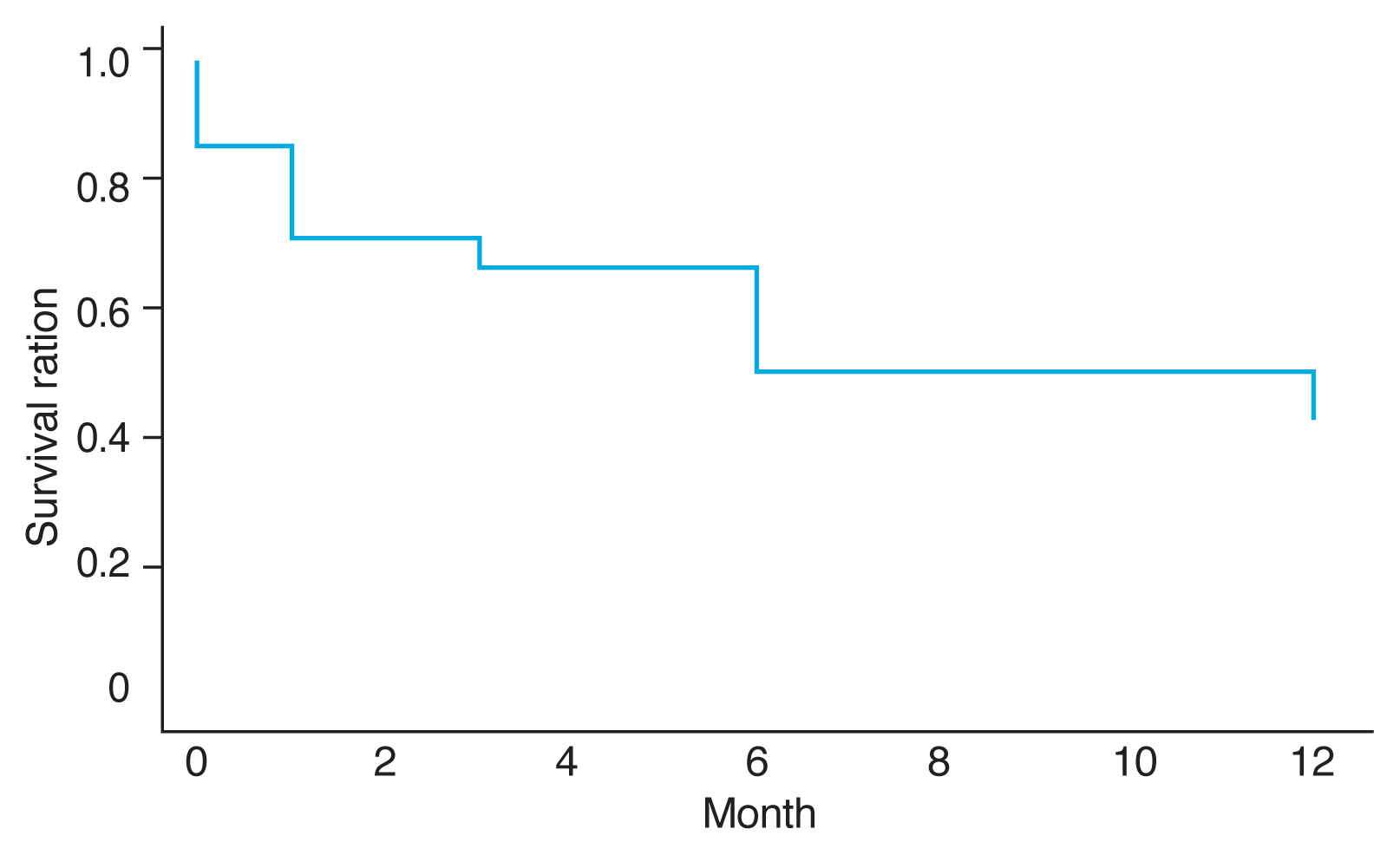
Fig. 2
Mean intraocular pressure of the treatment success group at each period following selective laser trabeculoplasty. *Determined by paired t-test between mean intraocular pressure at each follow-up period and mean baseline intraocular pressure of the treatment success group (n = 18).
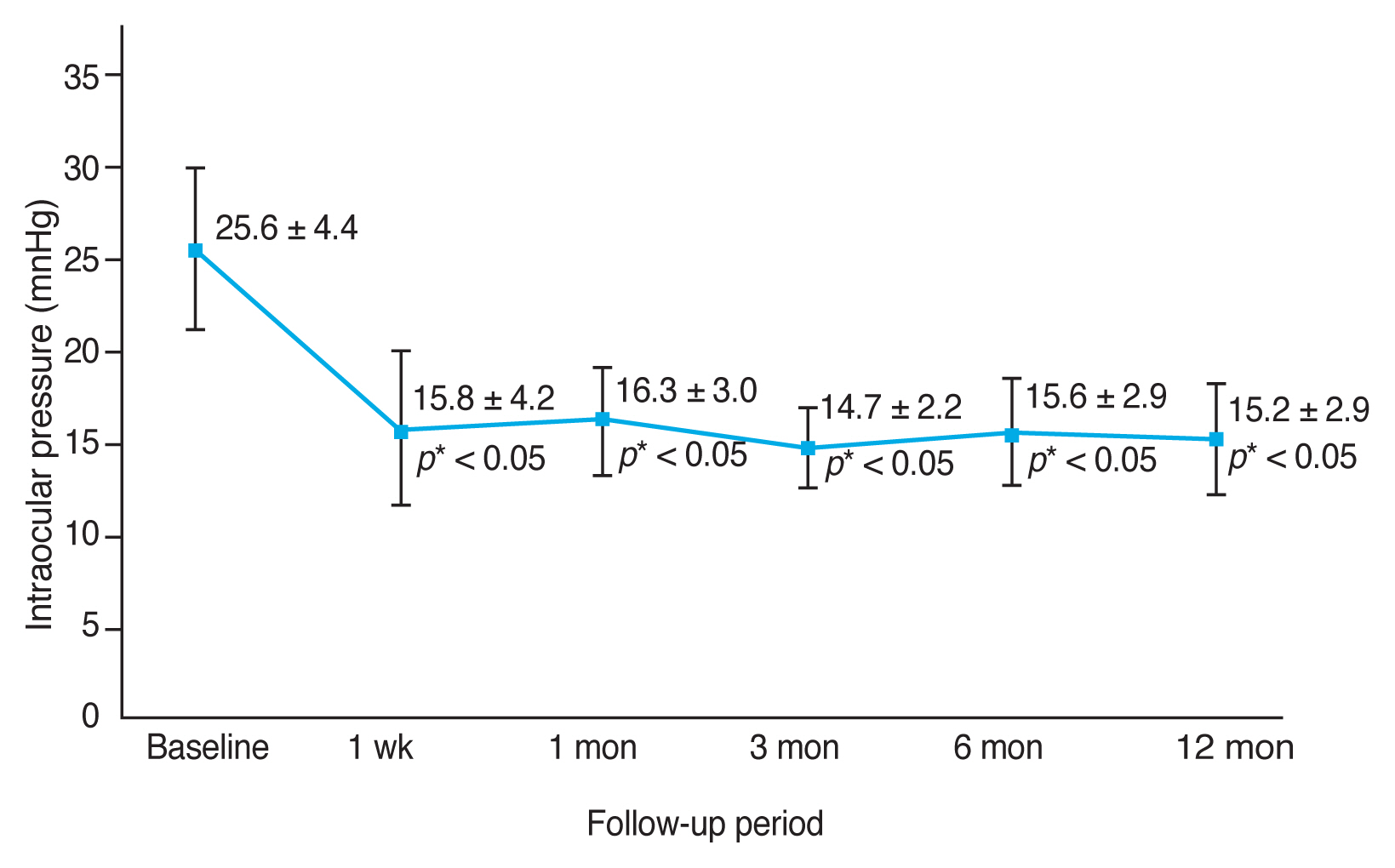
Table 1
Demographics and ocular characteristics of patients with pseudoexfoliation glaucoma
Table 2
Mean IOP of enrolled patients at each time period
| Follow-up period | No. of eyes included | IOP of the included patients (mmHg) | Baseline IOP of the included patients (mmHg) | p-value* | IOP of the excluded patients† (mmHg) |
|---|---|---|---|---|---|
| Baseline | 43 | 26.7 ± 5.8 | NA | NA | NA |
| 1 wk | 31 | 15.7 ± 3.8 | 26.5 ± 5.0 | < 0.05 | 23.8 ± 6.1 (12) |
| 1 mon | 26 | 16.4 ± 3.5 | 27.0 ± 5.1 | <0.05 | 25.2 ± 7.9 (5) |
| 3 mon | 25 | 15.8 ± 2.8 | 27.0 ± 4.6 | <0.05 | 22.0 (1) |
| 6 mon | 24 | 16.8 ± 3.4 | 26.9 ± 4.5 | <0.05 | 28.0 (1) |
| 12 mon | 18 | 15.2 ± 2.9 | 25.6 ± 4.4 | <0.05 | 24.5 ± 7.2 (6) |
Values are presented as number, mean ± standard deviation, or mean ± standard deviation (No. of eyes excluded).
† Patients who were just corresponded to failure at that time (i.e., those who would be excluded from the further analysis) because they failed to meet the criteria for success (≥20% reduction in IOP from baseline and IOP ≤22 mmHg at 12 months after treatment without additional anti-glaucomatous intervention).
Table 3
Comparison of the baseline characteristics between the treatment success and failure groups at 12 months after selective laser trabeculoplasty
| Parameter | Success group* (n = 18 eyes) | Failure group (n = 25 eyes) | p-value |
|---|---|---|---|
| Age (yr) | 73.2 ± 8.5 | 70.8 ± 8.3 | 0.482† |
| Sex (male : female) | 10 (55.6) : 8 (44.4) | 14 (56.0) : 11 (44.0) | 0.977‡ |
| Baseline IOP (mmHg) | 25.6 ± 4.4 | 27.4 ± 5.9 | 0.128† |
| Phakia : pseudophakia | 11 (61.1) : 7(38.9) | 10 (40.0) : 15 (60.0) | 0.172‡ |
| BCVA (logMAR) | 0.16 ± 0.3 | 0.31 ± 0.4 | 0.085† |
| Spherical equivalents (diopters) | 0.01 ± 0.9 | −0.41 ± 1.6 | 0.461† |
| MD (dB) | −17.2 ± 9.9 | −19.0 ± 8.9 | 0.595† |
| PSD (dB) | 8.1 ± 4.9 | 8.2 ± 3.3 | 0.882† |
IOP = intraocular pressure; BCVA = best-corrected visual acuity; logMAR = logarithm of the minimum angle of resolution; MD = mean deviation; PSD = pattern standard deviation.
References
1. Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 2003;121:48-56.


2. Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res 1995;60:359-71.


3. Chi SC, Kang YN, Hwang DK, Liu CJ. Selective laser trabeculoplasty versus medication for open-angle glaucoma: systematic review and meta-analysis of randomised clinical trials. Br J Ophthalmol 2020;104:1500-7.


4. Garg A, Vickerstaff V, Nathwani N, et al. Efficacy of repeat selective laser trabeculoplasty in medication-naive open-angle glaucoma and ocular hypertension during the LiGHT trial. Ophthalmology 2020;127:467-76.


5. Kennedy JB, SooHoo JR, Kahook MY, Seibold LK. Selective laser trabeculoplasty: an update. Asia Pac J Ophthalmol (Phila) 2016;5:63-9.

6. Miki A, Kawashima R, Usui S, et al. Treatment outcomes and prognostic factors of selective laser trabeculoplasty for open-angle glaucoma receiving maximal-tolerable medical therapy. J Glaucoma 2016;25:785-9.


7. Park HW, Han SS, Park JW. The Effectiveness of selective laser trabeculoplasty in patients with medically uncontrolled open-angle glaucoma. J Korean Ophthalmol Soc 2017;58:828-35.

10. Kanthan GL, Mitchell P, Burlutsky G, et al. Pseudoexfoliation syndrome and the long-term incidence of cataract and cataract surgery: the blue mountains eye study. Am J Ophthalmol 2013;155:83-8.


11. Choi J, Park KH. Clinical characteristics of Korean patients with pseudoexfoliation syndrome. J Korean Ophthalmol Soc 2006;47:577-86.
12. Gracner T. Intraocular pressure response of capsular glaucoma and primary open-angle glaucoma to selective Nd:YAG laser trabeculoplasty: a prospective, comparative clinical trial. Eur J Ophthalmol 2002;12:287-92.


13. Vesti E, Kivela T. Exfoliation syndrome and exfoliation glaucoma. Prog Retin Eye Res 2000;19:345-68.


14. Katsanos A, Konstas AG, Mikropoulos DG, et al. A review of the clinical usefulness of selective laser trabeculoplasty in exfoliative glaucoma. Adv Ther 2018;35:619-30.



15. Goldenfeld M, Geyer O, Segev E, et al. Selective laser trabeculoplasty in uncontrolled pseudoexfoliation glaucoma. Ophthalmic Surg Lasers Imaging 2011;42:390-3.


16. Goosen E, Coleman K, Visser L, Sponsel WE. Racial differences in selective laser trabeculoplasty efficacy. J Curr Glaucoma Pract 2017;11:22-7.



17. Kaliaperumal S, Rao VA, Harish SB, Ashok L. Pseudoexfoliation on pseudophakos. Indian J Ophthalmol 2013;61:359-61.



19. Park KA, Kee C. Pseudoexfoliative material on the IOL surface and development of glaucoma after cataract surgery in patients with pseudoexfoliation syndrome. J Cataract Refract Surg 2007;33:1815-8.


20. Melamed S, Ben Simon GJ, Levkovitch-Verbin H. Selective laser trabeculoplasty as primary treatment for open-angle glaucoma: a prospective, nonrandomized pilot study. Arch Ophthalmol 2003;121:957-60.


21. Shazly TA, Smith J, Latina MA. Long-term safety and efficacy of selective laser trabeculoplasty as primary therapy for the treatment of pseudoexfoliation glaucoma compared with primary open-angle glaucoma. Clin Ophthalmol 2010;5:5-10.



22. Garg A, Gazzard G. Selective laser trabeculoplasty: past, present, and future. Eye (Lond) 2018;32:863-76.



23. Ayala M, Chen E. Comparison of selective laser trabeculoplasty (SLT) in primary open angle glaucoma and pseudoexfoliation glaucoma. Clin Ophthalmol 2011;5:1469-73.



24. Lindegger DJ, Funk J, Jaggi GP. Long-term effect of selective laser trabeculoplasty on intraocular pressure in pseudoexfoliation glaucoma. Klin Monbl Augenheilkd 2015;232:405-8.


25. Miraftabi A, Nilforushan N, Nassiri N, Nouri-Mahdavi K. Selective laser trabeculoplasty in patients with pseudoexfoliative glaucoma vs primary open angle glaucoma: a one-year comparative study. Int J Ophthalmol 2016;9:406-10.



26. Hodge WG, Damji KF, Rock W, et al. Baseline IOP predicts selective laser trabeculoplasty success at 12 months post-treatment: results from a randomised clinical trial. Br J Ophthalmol 2005;89:1157-60.


- TOOLS
-
METRICS

-
- 2 Crossref
- 0 Scopus
- 2,674 View
- 71 Download
- Related articles
-
Cases of Pseudophakic Pseudoexfoliation in Glaucoma Patients2012 October;26(5)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



