 |
 |
| Korean J Ophthalmol > Volume 34(5); 2020 > Article |
|
Dear Editor,
Mooren ulcer is an idiopathic autoimmune disease [1]. A broad variety of medical and surgical approaches for Mooren ulcer treatment have been developed, ranging from systemic immune suppression to conjunctival resection, lamellar keratoplasty, keratoepithelioplasty, deep anterior lamellar keratoplasty with amniotic membrane transplantation, tissue adhesives and tectonic graft [1-4].
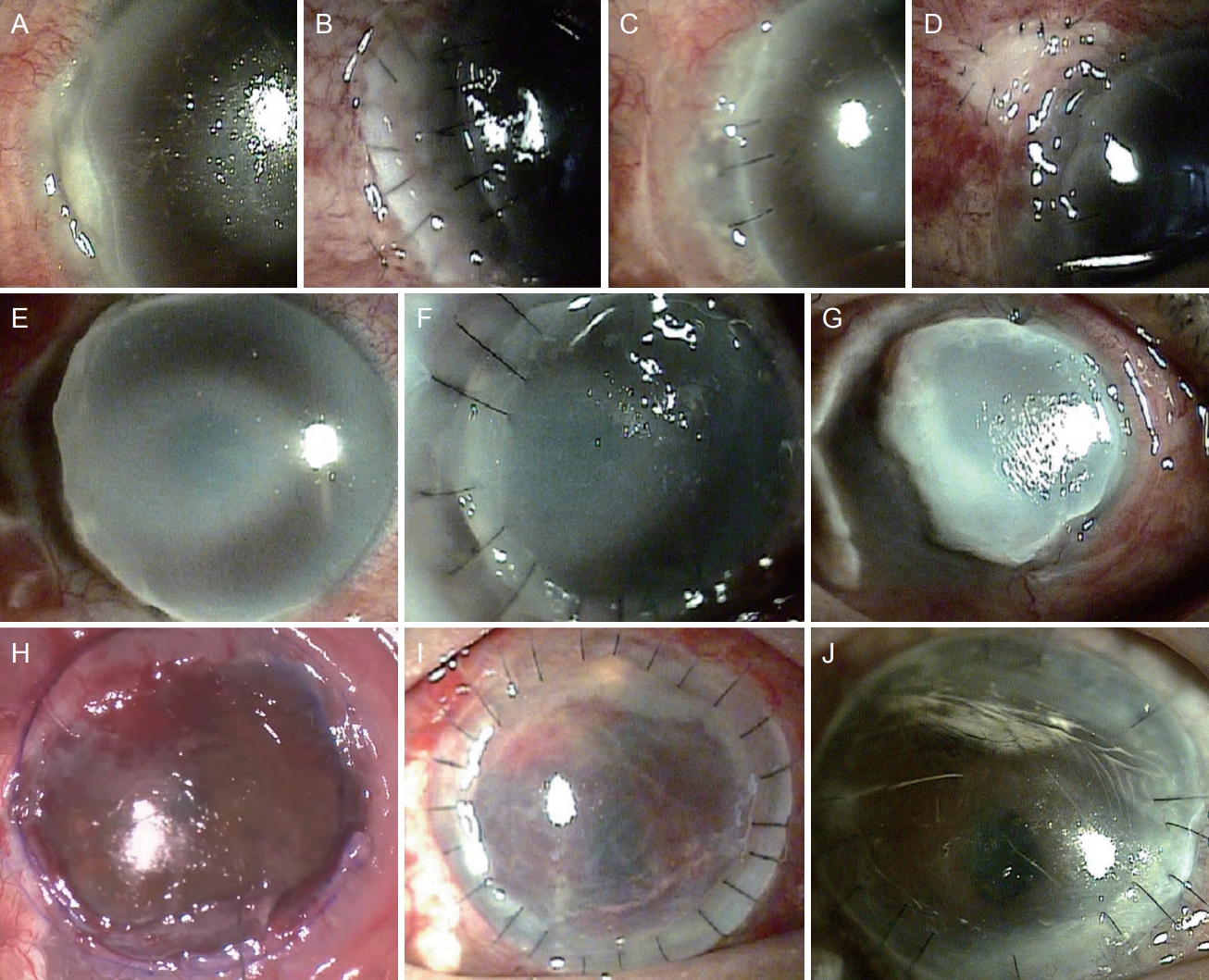
We report a case of Mooren ulcer successfully treated with large-diameter deep anterior lamellar keratoplasty (DALK) after failure of other surgeries. A 40-year-old man presented to our ophthalmology department with pain and decreased visual acuity of the right eye. Upon examination, there was an epithelial defect and corneal thinning on the temporal side of his right eye (Fig. 1A). His corrected visual acuity was 0.6 in his right eye and 0.8 in his left eye (Snellen charts). Intraocular pressure was 12/17 mmHg. We suspected peripheral corneal ulcer reflecting Mooren ulcer or another collagen vascular disease in the right eye. Administered medical treatment included topical moxifloxacin twice a day, fuorometholone twice a day, and solcoseryl eye drops every 2 hours in the right eye.
Despite medical treatment, the corneal ulcer continued to progress and we performed a systemic work up to rule out corneal ulcer caused by collagen vascular disease. Systemic evaluation showed increased total cholesterol level (415 mg/dL, reference120-220 mg/dL), low density lipoprotein cholesterol level (210 mg/dL, reference <130 mg/ dL) and fasting blood sugar (600 mg/dL, reference <100 mg/dL). No signs of rheumatologic diseases or infection were observed.
Based on these diagnostic tests, Mooren ulcer was suspected, and conjunctival resection and lamellar keratoplasty were performed in the right eye (Fig. 1B). After the first surgery, the graft was successful for 3 months, at which point the ulcer started to progress again both centrally and circumferentially despite strong immunosuppressive agents including topical and oral tacrolimus combined with steroid (Fig. 1C). To prevent ulcer progression, we performed keratoepithelioplasty (Fig. 1D), which failed to mitigate ulcer progression (Fig. 1E).
Six months after keratoepithelioplasty, we performed a second conjunctival resection and semi-annular lamellar keratoplasty (Fig. 1F). This graft was well maintained for 3 months with strong immune suppression. However, the graft then started to dissolve, and the remaining central island of the cornea began to melt again. The cornea showed extreme thinning near the point of perforation 4 months after semi-annular lamellar keratoplasty (Fig. 1G). His visual acuity had decreased to 0.02.
Based on these values, additional surgical treatment was proposed, and we performed large-diameter deep anterior lamellar keratoplasty (Fig. 1H, 1I). Visual acuity slowly recovered and the large-diameter corneal graft remained clear with only topical immunosuppression for 9 consecutive months (Fig. 1J). Even with strong immunosuppression such as oral tacrolimus and steroid after surgical treatment, Mooren ulcer progresses and leads to corneal perforation in 11% to 13.3% of patients [1-3].
In intractable Mooren ulcer, there are several surgical treatment options [1-4]. Crescent or semi-annular lamellar keratoplasty can be enough when the ulcer progresses within that meridian. However, when the fulminant course of ulcerative changes continues in the centripetal and circumferential directions, the antigenic source of the cornea needs to be removed before further damage.
We found large-diameter DALK to be a useful alternative for treatment of Mooren ulcer. It can control the inflammatory process by removing the total cornea, except the endothelium and DescemetŌĆÖs membrane, which is the main antigenic stimulus in the pathogenesis of Mooren ulcer. The DALK procedure can be difficult when the cornea is perforated [5], so the decision to remove most of the corneal layer should be made before ulcerative changes lead to corneal perforation.
Fig.┬Ā1.
Corneal change with time. (A) Corneal epithelial defect and thinning with overhanging edge at temporal side in right eye. (B) Crescentic lamella corneal graft at postoperative 1 day. (C) Melting crescentic lamella graft with inflammation. (D) In keratoepithelioplasty, corneal lenticule was sutured on bare sclera. (E) Melting total crescentic lamella graft and corneal lenticule with severe thinning progressing circumferentially and centrally. (F) Semi-annular lamella graft was re-sutured. (G) Melting semi-anuular graft with inflammation. (H) Large (9.5 mm) diameter recipient bed was prepared after removing melted cornea in deep anterior lamella keratoplasty. (I) Large (9.5 mm) diameter anterior lamella graft was sutured. (J) Cornea remained clear without inflammation after large diameter deep anterior lamella keratoplasty. Informed consent for publication of the clinical image was obtained from the patients.
References
2. Krachmer JH, Mannis MJ, Holland EJ. Mooren ulcer. In: Krachmer JH, Mannis MJ, Holland EJ, Cornea. 3rd ed. St. Louis: Mosby/Elsevier; 2011. p. 1149-53.
3. Guindolet D, Reynaud C, Clavel G, et al. Management of severe and refractory MoorenŌĆÖs ulcers with rituximab. Br J Ophthalmol 2017;101:418-22.


- TOOLS
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 2,972 View
- 60 Download
- Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



