 |
 |
| Korean J Ophthalmol > Volume 34(1); 2020 > Article |
|
Abstract
Purpose
To investigate the influence of donor age on corneal graft survival following primary penetrating keratoplasty (PK) with imported donor corneas.
Methods
The eyes of patients who underwent primary PK with imported donor corneas were classified retrospectively into two groups according to a donor-age cutoff of 65 years. Primary outcome measures were rejection-free graft survival and graft survival. Cox proportional hazard regression analysis was used to assess the factors affecting graft survival. Survival analysis was performed using the Kaplan-Meier method, while differences between groups were examined using a log-rank test. A subgroup analysis of low- and high-risk eyes according to preoperative diagnosis was also performed.
Results
A total of 140 eyes from 138 patients (age, 58 ┬▒ 18 years) were enrolled. Cox regression analysis revealed that the donor age of 65 years or older group presented an increased risk of both graft rejection and failure. Survival analysis revealed that rejection-free graft survival and graft survival rates were higher in eyes in the donor age of less than 65 years group. Finally, in the subgroup analysis, both rejection-free graft survival and graft survival rates were significantly higher in the donor age of less than 65 years group than in the donor age of 65 years or older group, but only in the low-risk subgroup.
The highly successful nature of penetrating keratoplasty (PK) is dependent upon the availability of suitable donor tissue [1,2]. The physiological and morphological characteristics of the donor corneal endothelium are important factors impacting the viability of corneal grafts [3]. Since several authors reported a decline in corneal endothelial cell density (ECD) with age [4,5,6], it has been considered that increasing donor age is associated with a higher risk of graft failure of PK. In recent decades, many researchers have wrestled with the issue of the impact of donor age on endothelial cell characteristics and the outcome of primary PK [7,8,9,10,11,12]; however, a precise correlation between donor age and the risk of graft failure has yet to be shown.
The Cornea Donor Study (CDS) was designed to determine the role of donor age in corneal graft survival in order to possibly increase the pool of available corneal donors by expanding the allowable age limits. The Specular Microscopy Ancillary Study (SMAS), which included CDS cohort patients followed for five years without graft failure, also determined the effect of donor age on long-term donor ECD [7]. The CDS five-year outcomes data revealed that five-year cumulative probability of graft survival (86%) was not different between the two donor age groups (12- to 65-year-olds and 66- to 75-year-olds) [9], while SMAS detected a slightly greater endothelial cell loss in relation to older donors [10]. Thereafter, with the extended follow-up, the investigators found that, although 10-year success rates were not different between the ages of 12 to 65 years (77%) and 66 to 75 years (71%), there was evidence of a donor age effect at the extremes of the age range; specifically, a higher success rate was noted when involving extremely young donors (96%, aged 12 to 33 years) and a lower success rate was noted when involving extremely older donors (62%, aged 72 to 75 years) [11]. The SMAS at 10 years also showed the rate of endothelial cell loss as being slightly greater with older donor age [12].
Imported donor corneas are commonly used in South Korea due to a shortage of donor tissue [13]. Wagoner et al. [5] reported comparable graft survival with imported donor corneas as compared with a Western series performed with domestic donors. However, their results showed that increasing donor age is significantly associated with decreased graft survival. In Korean studies, donor age was not associated with graft survival [14,15], but only a few studies to date have been carried out to evaluate such. This study was conducted to investigate the influence of donor age on graft survival in primary PK with imported donor corneas.
We retrospectively reviewed the medical records of patients who underwent primary PK between June 2005 and December 2017 at Seoul National University Bundang Hospital, Seongnam, Korea. A total of 140 eyes of 138 patients who underwent primary PK were included in this study. This study was approved by the institutional review board (B-1905-540-105) of Seoul National University Bundang Hospital and the requirement for informed patient consent was waived. The study complied with the guidelines of the Declaration of Helsinki.
We evaluated baseline characteristics of both the tissue transplant recipientsŌĆöincluding age, sex, history of diabetes, and preoperative diagnosesŌĆöand of the donorsŌĆöincluding age, sex, race, ECD (cells/mm2), graft diameter, death to harvest time, and harvest to operation time.
The eyes were classified into two groups according to donor age with 65 years acting as the cutoff age, similar to as in the CDS [7,11]. Many United States eye banks have also set an upper age limit for donor eligibility as 65 years [9]. Additional survival analyses were replicated in four data-derived donor age subgroups (<35, 35-49, 50-64, and Ōēź65 years), which showed relatively constant numbers of cases within each of the four subgroups.
The eyes were also classified into two groups according to preoperative diagnoses for subgroup analysis, a high-risk group that included eyes whose preoperative diagnoses were corneal perforation or thinning or infectious keratitis and a low-risk group included eyes with preoperative diagnoses of corneal opacity, bullous keratopathy, keratoconus, or stromal dystrophy.
All PK procedures were performed by a single experienced surgeon (JYH), and all procedures were standardized [16]. All donor corneas were obtained from an eye bank in the United States (SightLife Eye Bank, Seattle, WA, USA). All donor corneas were preserved in Optisol-GS (Bausch & Lomb, Irvine, CA, USA) and stored at 4Ōäā. We did not match human leukocyte antigens between donors and recipients. All grafts were allocated randomly regardless of human leukocyte antigens and sex. The donor corneas were punched through the corneal endothelium, measuring 7.0, 7.25, 7.5, 7.75, or 8.0 mm in diameter, using a radial vacuum trephine (Barron Precision Instruments; Katena Products, Denville, NH, USA). The recipient corneas were trephined either to exactly match the size of the donor cornea or as 0.25 or 0.5 mm smaller than the donor cornea according to the patient's preoperative diagnosis or eye condition. The donor corneas were sutured with interrupted sutures with 10-0 nylon (Alcon Laboratories, Fort Worth, TX, USA). Directly after PK, both 0.5 mL of gentamicin 4% and 0.5 mL of dexamethasone 0.8% were injected subconjunctivally. All patients were treated with topical prednisolone acetate 1% eye drops and moxifloxacin 0.5% eye drops four times daily during the first three months after surgery; the doses were gradually tapered and continued once a day for the first year after surgery [17].
Primary outcomes measures were rejection-free graft survival and graft survival; rejection-free graft survival was defined as the time span from keratoplasty to the first diagnoses of graft rejection and graft survival was defined until graft clarity was maintained without graft failure. Graft rejection was defined as corneal edema and the appearance of an endothelial rejection line or inflammation (e.g., stromal infiltrate, keratic precipitates, cells in the anterior chamber, ciliary injection) in a graft that was previously clear. Patients with clinical evidence of rejection were managed with a combination of oral prednisolone (1 mg/kg body weight) and topical prednisolone acetate 1% given at one-hour intervals, with rapid tapering following the resolution of rejection. Graft failure was defined as a loss of central graft clarity that compromised vision for a minimum of three consecutive months.
At first, Cox proportional hazard regression analysis was used to assess the relationship between baseline factors and graft survival. After confirming the influence of donor age on graft survival, we compared the baseline characteristics of two groups according to donor age with the chi-squared and Fisher exact tests. Survival analysis was performed using the Kaplan-Meier method. Differences between groups were assessed using the log-rank test. We also evaluated survival analysis with other baseline factors that could affect graft survival. To evaluate the trend of ECD across the four donor age subgroups, the Jonckheere-Terpstra test was conducted, while the Kruskal-Wallis test and the Mann-Whitney test were used for comparison of the ECD among the four donor age subgroups. Subgroup analyses of low- and high-risk eyes according to preoperative diagnoses were also performed. All calculations were completed using the IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). A p-value of less than 0.05 was considered to be statistically significant.
A total of 140 eyes of 138 patients who underwent primary PK were included in this research. The mean ┬▒ standard deviation age at the time of PK was 58 ┬▒ 18 years, and 99 (71%) of recipients were men. Preoperative diagnoses of high-risk patients included those with corneal perforation or thinning (13 eyes, 9.2%) and infectious keratitis (10 eyes, 7.1%), while the low-risk group included patients with corneal opacity (71 eyes, 50.7%), bullous keratopathy (35 eyes, 25.0%), keratoconus (7 eyes, 5.0%), and stromal dystrophy (4 eyes, 2.9%).
Table 1 shows the baseline characteristics of recipients and donors in the two donor age groups. Eyes from donors aged three to 64 years old were included in the donor age of younger than 65 years group (group 1; n = 107, 76%), while those from donors aged 65 to 75 were included in the donor age of 65 years or older group (group 2; n = 33, 24%). Group 1 was subdivided into three subgroups (subgroups 1, 2, and 2) of donor age younger than 35 years (n = 16), donor age of 35 to 49 years (n = 27), and donor age of 50 to 64 years (n = 64). The mean donor age among all eyes was 52 ┬▒ 15 years (48 ┬▒ 14 years in group 1 and 67 ┬▒ 2 years in group 2, p < 0.001). There were no significant differences in baseline characteristics of the recipients and donors between the younger and older age groups except for mean donor age. The mean donor ECD was not significantly different between the two donor age groups (p = 0.131, paired t-test; 2,873 ┬▒ 375 vs. 2,766 ┬▒ 275 cells/mm2 for groups 1 and 2, respectively). However, when ECD was compared among the four donor age subgroups, the Jonckheere-Terpstra test revealed a significant trend for lower ECD values with increasing age (p = 0.003) (Fig. 1), while the Kruskal-Wallis test also suggested a significant difference among the four subgroups (p = 0.015). It was revealed that subgroup 1 had significantly higher ECD values than subgroups 2 and 3 (p = 0.008 and p = 0.016, respectively, Mann-Whitney U-test). Preservation time factors (i.e., death to preservation time and preservation to operation time) were not different between the two main groups. The mean follow-up period was 34 months (range, 3 to 112 months).
Of the 140 eyes, 70 eyes (50%) experienced graft rejection and 48 eyes (34%) experienced graft failure during the follow-up period. The primary cause of graft failure in all 48 eyes with graft failure was graft rejection.
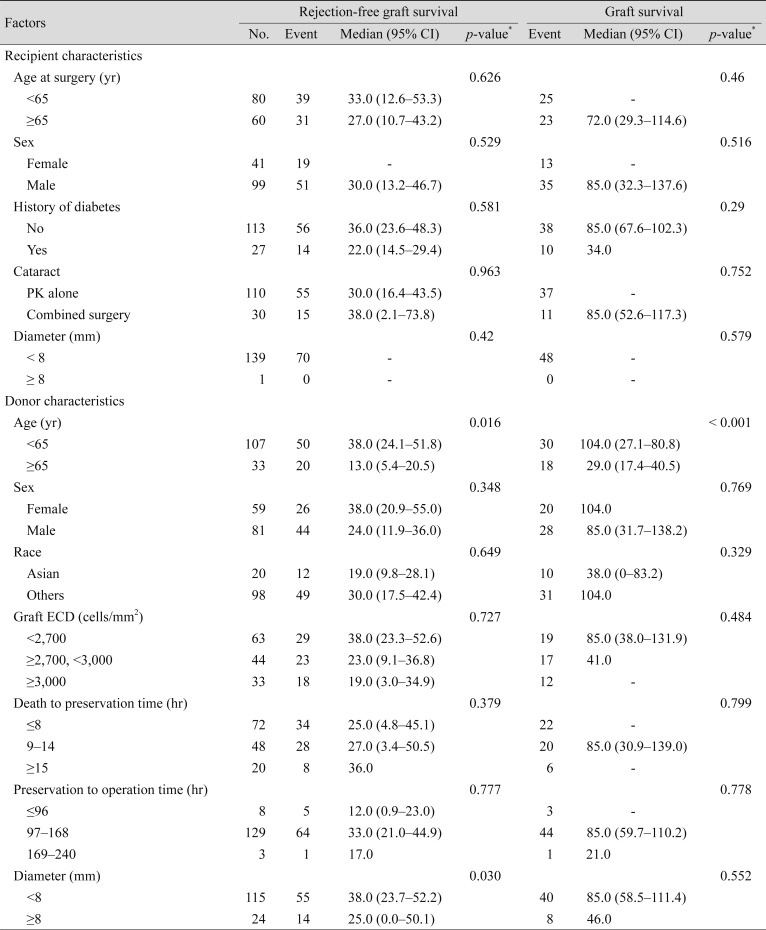
During multivariate analysis using Cox proportional hazard regression, donor age and graft diameter were associated with graft rejection but only donor age was associated with graft failure, with group 2 eyes at an increased risk of both graft rejection and graft failure (hazard ratio, 1.955; 95% confidence interval [CI], 1.151-3.321; p = 0.013 and hazard ratio, 2.83; 95% CI, 1.261-5.132; p = 0.001, respectively).
Table 2 shows the results of the log-rank test for possible risk factors for rejection-free graft survival and graft survival in all eyes. Among all possible risk factors, donor age was associated with rejection-free graft survival and graft survival (log-rank test; X2 = 5.825, p = 0.016 vs. X2 = 13.058, p < 0.001, respectively), while graft diameter was associated with rejection-free graft survival (log-rank test, p = 0.03).
Rejection-free graft survival and graft survival were significantly higher among patients in group 1 than group 2 (log-rank test; X2 = 5.825, p = 0.016 vs. X2 = 13.058, p < 0.001, respectively) (Fig. 2A, 2B).
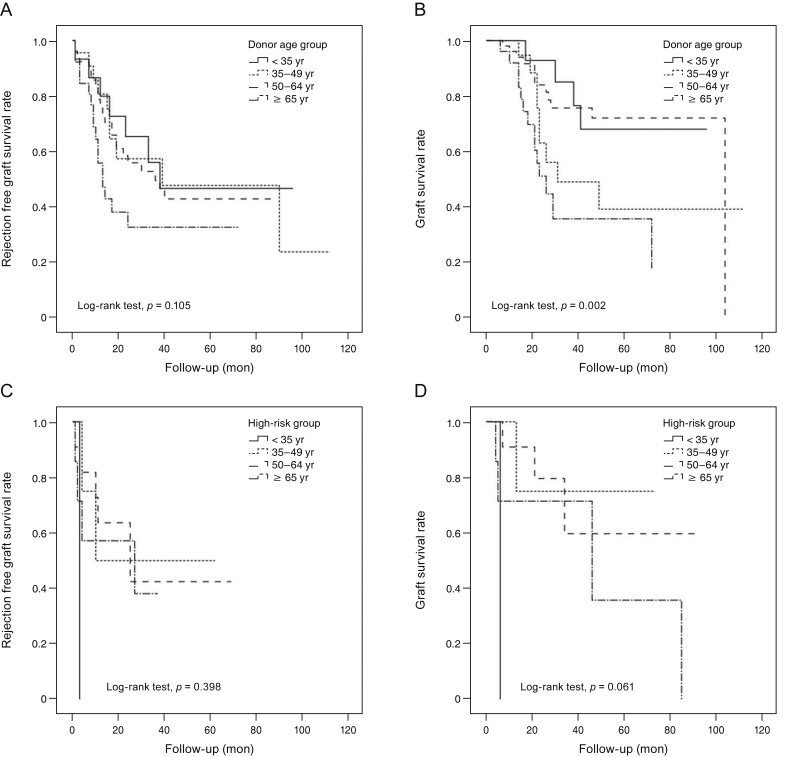
In the subgroup analysis of low- and high-risk groups according to preoperative diagnoses, 91 low-risk eyes (77.8%) and 16 high-risk eyes (69.6%) were included in group 1 and 26 low-risk eyes (22.2%) and seven high-risk eyes (30.4%) were included in group 2. It was found that both rejection-free graft survival and graft survival rates were significantly higher in group 1 than group 2 but only among low-risk patients (log-rank test; X2 = 5.916, p = 0.015 vs. X2 = 12.472, p < 0.001, respectively) (Fig. 3A, 3B). In the high-risk group, both rejection-free graft survival and graft survival rates were not significantly different between the two donor age groups (log-rank test; X2 = 0.104, p = 0.747 vs. X2 = 1.153, p = 0.283, respectively) (Fig. 3C, 3D).
In exploring this association further across the entire donor age distribution by incorporating the three donor age subgroups, it was found that rejection-free graft survival rate was not found to be significantly different but the graft survival rate was significantly different among the groups (log-rank test; X2 = 5.895, p = 0.117 vs. X2 = 14.355, p = 0.002, respectively) (Fig. 4A, 4B). In a subgroup analysis according to preoperative diagnoses of the four donor age groups (three subgroups and group 2), it was also found that the rejection-free graft survival rate was not significantly different but the graft survival rate was significantly different among subgroups in the low-risk eyes (log-rank test; X2 = 6.131, p = 0.105 vs. X2 = 14.907, p = 0.002, respectively) (Fig. 5A, 5B). In the high-risk group, however, both rejection-free graft survival rate and graft survival rate were not significantly different among the groups (log-rank test; X2 = 2.957, p = 0.398 vs. X2= 7.385, p = 0.061, respectively) (Fig. 5C, 5D).
This study investigated the impact of donor age on graft survival in primary PK. According to our results, donor age was the only factor that was associated with graft failure in multivariate analysis performed using Cox proportional hazard regression. Survival analysis also confirmed that both rejection-free graft survival and graft survival rates were significantly higher in eyes with a donor age of younger than 65 years. However, in subgroup analyses performed according to preoperative diagnoses, the result was valid only in the low-risk group. We suggest therefore that donor age might have an association with graft survival in primary PK with imported donor corneas, especially in preoperatively low-risk eyes. It is thought that certain preoperative diagnoses have a greater influence on graft survival in comparison with donor age.
In prior study of the CDS cohort that evaluated 10-year success rates, the investigators reported that there was evidence of a donor age effect at the extremes of the age rangeŌĆöthat is, the success rate was higher for donors aged 12 to 33 years and lower for donors aged 72 to 75 yearsŌĆöin most PK procedures performed for endothelial disease [11], which suggests a significant effect of donor age on graft survival. To evaluate the donor age effects in further detail, we subdivided group 1 into three donor age subgroups and still observed a consistent finding of a lower survival rate in the oldest donor age group aged above 65 years, which was marked in the low-risk eyes. However, it was difficult to clearly observe the difference in survival rates according to increasing age among the three younger age subgroups below 65 years. We believe that donor age could have an influence on graft survival in PK with imported donor corneas, although the exact range of age is not apparent yet. Our finding of similar graft survival rates in the younger age groups may be related to the relatively small number of eyes were included and not controlling for preoperative diagnoses.
Bohringer et al. [18] reported that advanced donor age exerts a significant negative effect on chronic endothelial cell loss. There is no doubt that relatively low ECD is more frequently found in the corneas of older donors [5,6]. In our results, ECD tended to decrease with increasing age grade, which is a consistent result of prior studies and could explain the hypothesis that greater cell loss with increased donor age would have a negative effect on graft survival. However, there was no difference in ECD between the donor age of less than 65 years and donor age of 65 years or more groups, which couldn't explain clearly why the lower ECD leads to a lower survival rate in eyes with a donor age of 65 years or more. We suggest not only relatively low ECD but also other characteristics of donor corneas, such as configuration and flexibility, metabolic status, and level of histocompatibility antigen expression are thought to be impacted by donor age, which we couldn't evaluate in this study or using other clinical methods [19].
Since the number of domestic corneas is insufficient in Korea, using imported donor corneas is an important part of managing many patients in need of corneal transplantation. Previous studies have reported that PK performed with imported donor corneas is as effective and safe as when using domestic donor corneas, despite the longer preservation time [13,20,21]. It is predicted that corneal transplantation using imported donor corneas will continue to be performed due to the reported success rates achieved with imported corneas comparable to domestic corneas, lack of domestic corneas, and increasing cases of endothelial keratoplasty with their higher successful rates [22]. In our study, although there was no difference in preservation-to-surgery time between group 1 (mean, 129 hours) and group 2 (mean, 130 hours), the times were relatively long as compared with those of previously reported studies in Korea using domestic donor corneas. Effects of prolonged storage time of donor tissue may be another possible factor that may have some kind of influence on the lower survival rate seen with older donor corneas and could be related to the discordance with the results from other reports that saw no influence of donor age on graft survival when using domestic donor corneas with relatively short storage times. Contrary to our expectations, despite quite different death to preservation times between the two groups (9.5 ┬▒ 4.8 hours in group 1 vs. 8.1 ┬▒ 2.9 hours in group 2, p = 0.051), group 1 eyes showed better survival rates, supporting the presence of adverse effects of older donor age on graft survival.
The conditions of the donor cornea can also be taken into account when performing keratoplasty with imported donor corneas, whereas domestic corneas cannot be selected. Transplant surgeons should be informed by good evidence, thus balancing the need to maximize the utilization of donated tissue while maintaining high standards for graft survival and visual outcome. Against the background of an aging population, the results of our study suggest that donor age could be a considerable factor when selecting imported donor corneas among candidate donors, at least in preoperatively low-risk patients with primary PK.
There were some limitations in our study. First, we included only a small number of patients with inhomogeneous preoperative diagnoses, which could result in a limitation in the interpretation of the results. Further studies including a higher number of patients with uniform preoperative diagnoses are necessary. Second, races between donors and recipients (all Korean) were not matched. It may be advantageous though that this study involved data only for Korean recipients, as it could be a reference for other institutions in Korea using imported corneas. Third, the maximum follow-up period was limited. Considering that the cumulative number of immunologic graft reactions was significantly increased with the length of the follow-up period, one might infer that, with a longer follow-up period, the cumulative number of graft reactions would be higher than the number found in this study. Finally, we did not assess actual endothelial cell loss according to donor age. The examination of endothelial cell loss rate in relation to different donor ages could further predict graft survival.
In conclusion, rejection-free graft survival and graft survival rates were significantly higher among eyes with younger donor ages below 65 years as compared with among those with older donor ages of 65 to 75 years in primary PK performed with imported donor corneas. Our results support that considering the donor age in primary PK using imported donor corneas would help increase graft survival, especially in preoperatively low-risk patients. Further controlled studies are necessary to evaluate the exact effects of the donor age not merely on primary PK but also on endothelial keratoplasty, which is the preferred treatment option worldwide for endothelial dysfunction.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Williams KA, Roder D, Esterman A, et al. Factors predictive of corneal graft survival. Report from the Australian Corneal Graft Registry. Ophthalmology 1992;99:403-414.


2. Kim MK, Lee JH. Long-term outcome of graft rejection after penetrating keratoplasty. J Korean Ophthalmol Soc 1997;38:1553-1560.
3. Krohn J, Hovding G. The influence of donor age and cause of death on corneal endothelial cell density. Acta Ophthalmol Scand 2005;83:746-750.


4. Kwon JW, Cho KJ, Kim HK, et al. Analyses of factors affecting endothelial cell density in an eye bank corneal donor database. Cornea 2016;35:1206-1210.


5. Wagoner MD, Gonnah el-S, Al-Towerki AE. King Khaled Eye Specialist Hospital Cornea Transplant Study Group. Outcome of primary adult optical penetrating keratoplasty with imported donor corneas. Int Ophthalmol 2010;30:127-136.



6. Armitage WJ, Jones MN, Zambrano I, et al. The suitability of corneas stored by organ culture for penetrating keratoplasty and influence of donor and recipient factors on 5-year graft survival. Invest Ophthalmol Vis Sci 2014;55:784-791.


7. Sugar A, Gal RL, Beck W, et al. Baseline donor characteristics in the Cornea Donor Study. Cornea 2005;24:389-396.


8. Beck RW, Gal RL, Mannis MJ, et al. Is donor age an important determinant of graft survival? Cornea 1999;18:503-510.


9. Cornea Donor Study Investigator Group. Gal RL, Dontchev M, et al. The effect of donor age on corneal transplantation outcome results of the cornea donor study. Ophthalmology 2008;115:620-626.



10. Cornea Donor Study Investigator Group. Lass JH, Gal RL, et al. Donor age and corneal endothelial cell loss 5 years after successful corneal transplantation. Specular microscopy ancillary study results. Ophthalmology 2008;115:627-632.



11. Writing Committee for the Cornea Donor Study Research Group. Mannis MJ, Holland EJ, et al. The effect of donor age on penetrating keratoplasty for endothelial disease: graft survival after 10 years in the Cornea Donor Study. Ophthalmology 2013;120:2419-2427.


12. Writing Committee for the Cornea Donor Study Research Group. Lass JH, Benetz BA, et al. Donor age and factors related to endothelial cell loss 10 years after penetrating keratoplasty: Specular Microscopy Ancillary Study. Ophthalmology 2013;120:2428-2435.


13. Park SH, Kim JH, Joo CK. The clinical evaluations of the penetrating keratoplasty with imported donor corneas. J Korean Ophthalmol Soc 2005;46:28-34.
14. Kong SJ, Cho K, Kim MS. Analysis of factors affecting the decrease of endothelial cell density in imported donor corneas. J Korean Ophthalmol Soc 2012;53:20-26.

15. Kim DH, Lee JY, Oh JY, et al. Comparative analysis of clinical outcome in penetrating keratoplasty using domestic or imported cornea. J Korean Ophthalmol Soc 2015;56:672-679.

16. Kim MJ, Kim JH, Jeon HS, et al. Effect of histocompatibility Y antigen matching on graft survival in primary penetrating keratoplasty. Cornea 2018;37:33-38.


17. Shimazaki J, Iseda A, Satake Y, Shimazaki-Den S. Efficacy and safety of long-term corticosteroid eye drops after penetrating keratoplasty: a prospective, randomized, clinical trial. Ophthalmology 2012;119:668-673.


18. Bohringer D, Reinhard T, Spelsberg H, Sundmacher R. Influencing factors on chronic endothelial cell loss characterised in a homogeneous group of patients. Br J Ophthalmol 2002;86:35-38.



19. Palay DA, Kangas TA, Stulting RD, et al. The effects of donor age on the outcome of penetrating keratoplasty in adults. Ophthalmology 1997;104:1576-1579.


20. Shimazaki J, Shinozaki N, Shimmura S, et al. Efficacy and safety of international donor sharing: a single-center, case-controlled study on corneal transplantation. Transplantation 2004;78:216-220.


21. Cho EY, Kim MS. Penetrating keratoplasty before and after establishment of Korean Network for Organ Sharing. J Korean Ophthalmol Soc 2006;47:525-530.
Fig.┬Ā1
Comparison of endothelial cell densities (ECDs, cells/mm2) among donor corneas in four donor age subgroups. Mean ECD tended to decrease with increasing age grade (p = 0.003, Jonckheere-Terpstra test). It was revealed that donors aged <35 years had a significantly higher ECD than donors aged 50-64 or >65 years (*Statistical significance; p = 0.008 and p = 0.016, respectively, Mann%Whitney test).

Fig.┬Ā2
Kaplan-Meier plots of (A) rejection-free graft survival and (B) graft survival in donor age <65 years and donor age Ōēź65 years groups (log-rank test; (A) X2 = 5.825, p = 0.016 vs. (B) X2 = 13.058, p < 0.001).
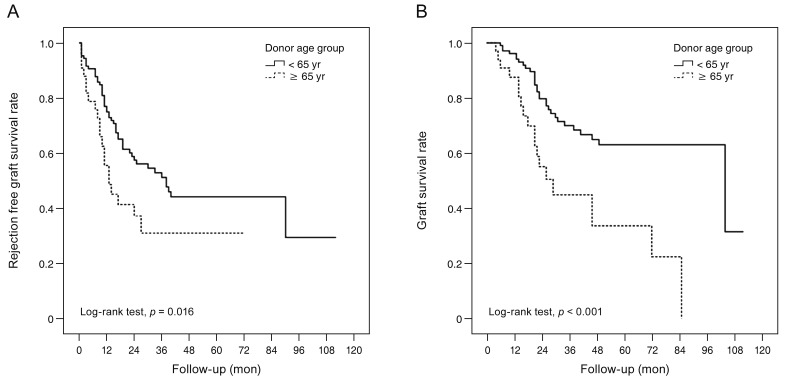
Fig.┬Ā3
Kaplan-Meier plots of rejection-free graft survival and graft survival in the two main donor age groups after division into low- and high-risk groups. In the low-risk group, both (A) rejection-free graft survival and (B) graft survival were significantly higher in the donors age <65 years group than that of Ōēź65 years group (log-rank test; X2 = 5.916, p = 0.015 vs. X2 = 12.472, p < 0.001, respectively). In the high-risk group, both (C) rejection-free survival and (D) graft survival were not significantly different between the two donor age groups (log-rank test; X2 = 0.104, p = 0.747; X2 = 1.153, p = 0.283, respectively).

Fig.┬Ā4
Kaplan-Meier plots of (A) rejection-free graft survival and (B) graft survival in four data-derived donor age subgroups (log-rank test; X2 = 5.895, p = 0.117; X2 = 14.355, p = 0.002, respectively).

Fig.┬Ā5
Kaplan-Meier plots of rejection-free graft survival and graft survival in four data-derived donor age subgroups after division into low- and high-risk groups. In the low-risk group, it was found that (A) the rejection-free graft survival rate was not found to be significantly different, while the (B) graft survival rate was significantly different among the groups (log-rank test; X2 = 6.131, p = 0.105 vs. X2 = 14.907, p = 0.002, respectively). In the high-risk group, both (C) the rejection-free graft survival rate and (D) graft survival rate were not significantly different among the groups (log-rank test; X2 = 2.957, p = 0.398 vs. X2 = 7.385, p = 0.061, respectively).
- TOOLS




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




