 |
 |
| Korean J Ophthalmol > Volume 33(1); 2019 > Article |
Abstract
Purpose
To understand the ophthalmic clinical features and outcomes of facial nerve palsy patients who were referred to an ophthalmic clinic for various conditions like Bell's palsy, trauma, and brain tumor.
Methods
A retrospective study was conducted of 34 eyes from 31 facial nerve palsy patients who visited a clinic between August 2007 and July 2017. The clinical signs, management, and prognosis were analyzed.
Results
The average disease period was 51.1 ┬▒ 20.6 months, and the average follow-up duration was 24.0 ┬▒ 37.5 months. The causes of facial palsy were as follows: Bell's palsy, 13 cases; trauma, six cases; brain tumor, five cases; and cerebrovascular disease, four cases. The clinical signs were as follows: lagophthalmos, 24 eyes; corneal epithelial defect, 20 eyes; conjunctival injection, 19 eyes; ptosis, 15 eyes; and tearing, 12 eyes. Paralytic strabismus was found in seven eyes of patients with another cranial nerve palsy (including the third, fifth, or sixth cranial nerve). Conservative treatments (like ophthalmic ointment or eyelid taping) were conducted along with invasive procedures (like levator resection, tarsorrhaphy, or botulinum neurotoxin type A injection) in 17 eyes (50.0%). Over 60% of the patients with symptomatic improvement were treated using invasive treatment. At the time of last following, signs had improved in 70.8% of patients with lagophthalmos, 90% with corneal epithelium defect, 58.3% with tearing, and 72.7% with ptosis. The rate of improvement for all signs was high in patients suffering from facial nerve palsy without combined cranial nerve palsy.
Conclusions
The ophthalmic clinical features of facial nerve palsy were mainly corneal lesion and eyelid malposition, and their clinical course improved after invasive procedures. When palsy of the third, fifth, or sixty cranial nerve was involved, the prognosis and ophthalmic signs were worse than in cases of simple facial palsy. Understanding these differences will help the ophthalmologist take care of patients with facial nerve palsy.
The facial nerve (the seventh cranial nerve) controls the muscles of facial expression, and dysfunction of facial expression or the blink response occurs with a damaged facial nerve. Blink dysfunction is induced by weakness of the orbicularis oculi and ectropion. Lid retraction, decreased tear production, or a defective tear pump mechanism may also be induced. With facial nerve palsy, ophthalmic signs such as lid malposition, exposure keratopathy, dry eye, and tearing are common.
Facial nerve palsy can be divided into central palsy and peripheral palsy. Central facial palsy is induced by a brain disorder, whereas peripheral facial palsy is induced by a disorder of the facial nerve pathway emanating from the brain. In the case of central facial palsy, main causes include stroke, brain tumor, and trauma. Central facial palsy can be accompanied by palsy of another cranial nerve. Therefore, other neurologic signs (such as hemiparalysis, hypoesthesia, dysphrasia, or visual field defect) may be present. Causes of peripheral facial palsy include Bell's palsy, Ramsay-Hunt syndrome, trauma, and the compression of a facial nerve by tumor. Of these, the main cause is Bell's palsy. In this case, facial nerve damage occurs due to inflammation.
According to a study by Joseph et al. [1], it is very important to administer proper ophthalmic treatment for facial nerve palsy at the right time. This is because exposure keratopathy, which frequently occurs with facial nerve palsy, can cause serious ophthalmic sequelae like vision loss. In the same study, the median time interval from the onset of ocular symptoms to the initial ophthalmologic evaluation was 0.8 years.
Malhotra et al. [2] designed and reported a facial nerve grading instrument (FNGI). The FNGI grades and analyzes periorbital involvement using a combination of objective and subjective parameters. It is a useful tool to facilitate standardized grading and aid in planning case management. FNGI parameters include the extent of punctate epithelial erosion of the cornea; the resting position of the involved brow and eyelids (upper and lower); the dynamic function of the orbicularis oculi and frontalis, as monitored by lagophthalmos; the range of brow movement; and synkinesis. The FNGI represents progress towards a universal agreement in assessing and managing the ophthalmic manifestations of facial nerve palsy. For facial nerve palsy patients, an accurate understanding of ophthalmic features and timely treatment are very important.
The first treatment option for facial nerve palsy patients is nonsurgical in nature, defined by a conservative approach based on symptoms. In many patients, artificial tears, ophthalmic ointment, and taping are prescribed. This is because the most common ophthalmic signs are lagophthalmos, exposure keratopathy, and dry eye. Surgical intervention, botulinum neurotoxin, or filler injection are undertaken only in cases of long-lasting paralysis.
The purpose of this study was to understand the ophthalmic clinical features, methods of treatment, and prognoses for facial nerve palsy patients referred to an ophthalmic clinic. We also sought to understand the difference between patients with and without palsy involving other cranial nerves.
We analyzed 34 eyes from 31 facial nerve palsy patients who were referred to our ophthalmic clinic from August 2007 to July 2017. Patients with palsy involving other cranial nerves were also included. This retrospective study used data from medical records pertaining to past history, trauma history, clinical features, treatment methods, and prognoses. This study was approved by the institutional review board of CHA Bundang Medical Center in Seongnam (CHAMC IRB 2018-12-016-002), South Korea, and was performed in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all study participants.
Diagnosis, determination of treatment methods, operation, and follow-up monitoring were conducted by the same oculoplastic surgeon for each patient. A photo was taken during every visit to objectively record and evaluate signs. The distance from the center of the pupil to the upper eyelid margin (marginal reflex distance 1, MRD1) was measured with ImageJ ver. 1.52 (National Institutes of Health, Bethesda, MD, USA). The mean corneal diameter (11.5 mm) was used as a reference to set the scale for each photograph. If the upper eyelid margin was covered by skin due to brow ptosis or dermatochalasis, we gently lifted the skin of the upper eyelid and took a picture.
Two groups were compared in terms of signs, invasive procedures, and the degree of symptomatic improvement after treatment. The first group included patients with facial nerve palsy only. The second group included patients with both facial nerve palsy and palsy of the third, fifth, or sixth cranial nerve. Palsy of the third cranial nerve can affect Bell's phenomenon, and palsy of the sixth cranial nerve can cause eye movement abnormalities like paralytic strabismus or limitation of motion (LOM). Similarly, palsy of the fifth cranial nerve can cause decreased corneal perception.
Statistical analyses were performed with Windows IBM SPSS Statistics ver. 23 (IBM Corp., Armonk, NY, USA), using the independent sample t-test. A p-value of <0.05 was considered statistically significant.
The 31 patients studied ranged in age from 45 days to 91 years (range, 51.1 ┬▒ 20.6 years). The ratio of male to female was 19 : 12. There were 14 patients with palsy of the right eye, 14 patients with palsy of the left eye, and three patients with palsy of both eyes. Seven patients who also had cranial nerve palsy represented eight eyes. Of these patients, one had third cranial nerve palsy, and two had both fifth and sixth cranial nerve palsy. Four had mixed palsy involving the third, fifth, and sixth cranial nerves.
When classified by the cause of facial paralysis, there were 13 patients with Bell's palsy, six with trauma history, five with brain tumor, four with cerebrovascular disease, two with congenital paralysis, and one with meconium aspiration syndrome (Table 1).
The average disease period until initial ophthalmologic evaluation was 51.1 ┬▒ 119.0 months, ranging from 1 month to 50 years. The average follow-up monitoring duration was 24.0 ┬▒ 37.5 months, ranging 1 month to 10 years.
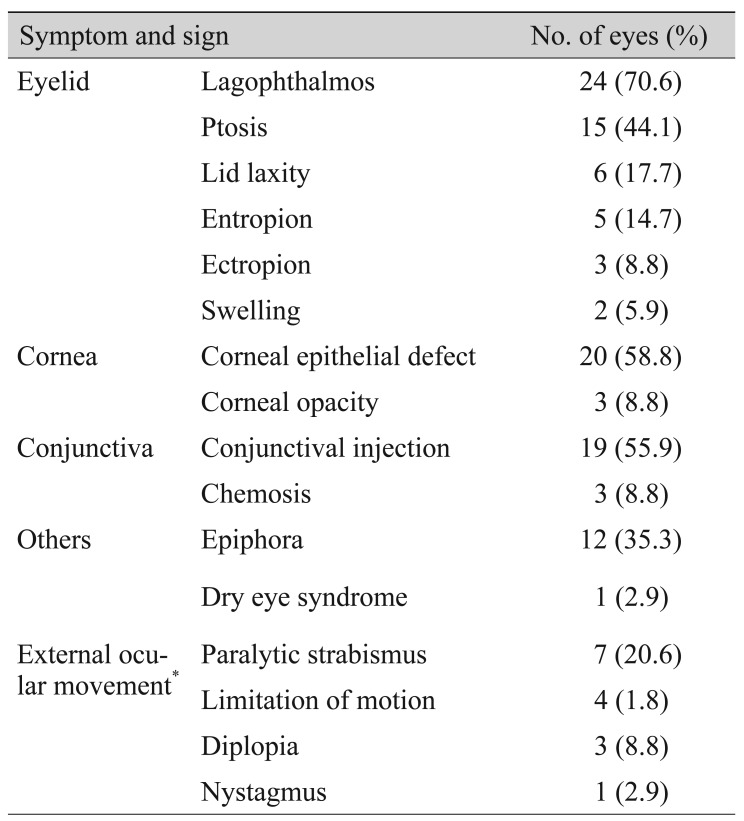
The most common ophthalmic signs caused by facial nerve palsy were lagophthalmos (24 eyes, 70.6%), corneal epithelium defect (20 eyes, 58.8%), and conjunctival injection (19 eyes, 55.9%). We divided these signs into categories: eyelid, cornea, conjunctiva, and eye movement. Signs related to the eyelid were lagophthalmos (24 eyes, 70.6%), ptosis (15 eyes, 44.1%), lid laxity, entropion, ectropion, and swelling. Corneal signs were corneal epithelium defect (20 eyes, 58.8%) and corneal opacity (three eyes, 8%). Conjunctival signs were conjunctival injection (19 eyes, 55.9%) and chemosis (three eyes, 8.8%). Signs related to eye movement were paralytic strabismus (seven eyes, 20.6%), LOM (four eyes, 11.8%), diplopia (three eyes, 8.8%), and nystagmus (one eye, 2.9%). Other symptoms were epiphora (12 eyes, 35.3%) and dry eye syndrome (one eye, 2.9%) (Table 2).
Ophthalmic ointment was prescribed to 21 eyes according to symptoms, and taping was conducted in six eyes. There was one eye which was treated by eye drops made from the patient's serum because of a hard- to- cure corneal epithelium defect, despite surgical intervention, ophthalmic ointment, and taping.
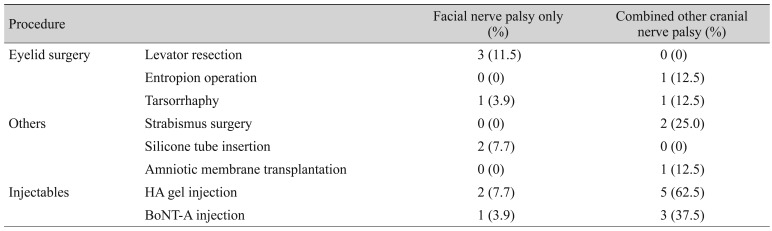
Invasive procedures included lid surgery, strabismus surgery, silicone tube insertion, and injection (Table 3). When comparing the two groups (group 1, facial nerve palsy only; group 2, facial nerve palsy with cranial nerve palsy), eye movement abnormalities like paralytic strabismus, LOM, diplopia, and nystagmus were found only in group 2. Two cases in group 2 included strabismus surgery and botulinum neurotoxin injection in the extraocular muscle. Eyelid surgeries for ptosis (levator resection) were conducted only in group 1.
The mean MRD1 on the facial nerve palsy side was 1.34 ┬▒ 1.89 mm in group 1 and ŌłÆ1.92 ┬▒ 1.24 mm in group 2. This analysis involved only unilateral palsy patients. Retraction (MRD1 >5.0 mm) on the facial nerve palsy or contralateral side was not present in any patients. Ptosis (MRD1 <2.0 mm) on the facial nerve palsy side was noted in nine patients (41.0%) in group 1 and six patients (100.0%) in group 2. Upper eyelid asymmetry, defined as an absolute difference in MRD1 (╬öMRD1) between the facial nerve palsy and contralateral side of greater than 1.0 mm, was present in 10 patients (45.5%) in group 1. Most of these cases (eight of 10, 80.0%) had facial nerve palsy affecting the lower eyelid. In group 2, five patients (83.3%) had facial nerve palsy affecting the lower eyelid. In all five of these cases, patients showed upper eyelid asymmetry (Table 4).
Epiphora was observed only in group 1. Two patients had dacryocystography which showed narrowing of the nasolacrimal duct, so two cases of silicone tube insertion were conducted in group 1. Hyaluronic acid injection was conducted in two patients (7.7%) in group 1 and five patients (62.5%) in group 2. And botulinum neurotoxin injection was conducted in one patient (3.9%) in group 1 and three patients (37.5%) in group 2 (Fig. 1A-1H).
We next compared the prognosis of patients receiving invasive procedures with those receiving conservative care. In the case of lagophthalmos, improvement was found in 13 patients (81.3%) in group 1. Among 16 patients, 12 were treated using conservative care only; the other 4 received invasive procedures like tarsorrhaphy or filler injection. These four patients (100.0%) showed improvement, but three patients (18.7%) who received conservative care only showed no improvement or got worse. In group 2, lagophthalmos was observed in all eight eyes. Among these, invasive procedures were conducted in six eyes. For eyes receiving invasive treatments, four (66.7%) improved. Two eyes (33.3%) receiving conservative care only showed no improvement.
Invasive procedures (such as botulinum neurotoxin injection or strabismus surgery) were conducted in four of seven eyes with paralytic strabismus. Of these four eyes, two showed improvement. In terms of LOM, two patients with improvement underwent an invasive procedure. Two patients with no improvement received conservative care only.
Ptosis was observed in nine eyes belonging to group 1. An invasive procedure was conducted on seven patients, and six showed improvement. Among two patients who received conservative care only, one showed improvement. In general, when active surgical intervention treatment was conducted, the prognosis of patients improved for all signs.
Two out of three patients with bilateral facial palsy had only facial nerve palsy, and the causes were Bell's palsy and brain tumor, respectively. One patient with bilateral facial palsy had fifth and sixth cranial nerve palsy and meconium aspiration syndrome. None of the six eyes had ptosis, and no invasive procedures were given. There was no particular difference between patients with bilateral facial palsy and those with unilateral facial palsy.
Patients with palsy of the third, fifth, and sixth cranial nerves all had severe signs and a poor prognosis. They required high rates of invasive procedures compared to patients with facial nerve palsy only. Of the four patients who had no improvement in lagophthalmos, three were from this group. The fourth patient had palsy of the fifth and sixth cranial nerves. Similarly, the two patients without improvement for corneal epithelial defect had palsy of the third, fifth, and sixth cranial nerves. Most of the patients who failed to improve had brain tumor or trauma, and most of them had been paralyzed for more than a year. Recurrences were most often observed in group 2, with signs of lagophthalmos, entropion, and exposure keratitis (Table 5).
The ophthalmic clinical features of facial nerve palsy are mainly corneal lesion and eyelid malposition [3]. Eyelid retraction is commonly thought to accompany facial nerve palsy, as it is related to unopposed levator function. But according to a study by Sinha et al. [4], this retraction occurs somewhat rarely, and most cases have a high-normal eyelid position (regardless of facial nerve palsy). In other words, patients do not have significant MRD1 asymmetry. Rather, they have a bilateral, relatively symmetric and elevated eyelid position. Nevertheless, the incidence of asymmetry was still higher than one would expect in the general population. The authors found that 15% of their patients had retraction, and 27% had upper eyelid asymmetry greater than 1.0mm (with the facial nerve palsy eyelid higher in most [86%] of these cases). In our study, no patient had retraction, and 53.6% of patients with unilateral facial nerve palsy had upper eyelid asymmetry greater than 1.0 mm (with the facial nerve palsy eyelid lower in most [13 of 15, 86.7%] of these cases). In the study by Sinha et al. [4], ptosis (MRD <2.5 mm) was uncommon on the facial nerve palsy side, with a prevalence of only 8%. But in our study, over 50% of patients had ptosis on the facial nerve palsy side. There could be different reasons for this. Compared to Westerners, Koreans have well-developed subcutaneous fat and more fat in front of the tarsus and orbital septum. Therefore, they have thick eyelids, and the subcutaneous attachment of the levator aponeurosis is weak. A well-developed fat layer and the periorbital soft tissue impede the function of the levator muscle. For this reason, we can predict that Koreans would have a lower retraction frequency compared to Westerners. Second, Korean patients have a smaller palpebral fissure than Western patients, so the standard of retraction may be higher for Korean patients. Third, there are differences in the level of brow ptosis between patients. When a patient has brow ptosis, the eyelids seem to droop, which can be mistaken for blepharoptosis. Ptosis and upper eyelid asymmetry were defined based on the degree of MRD1 in our study and the study by Sinha et al. [4]. But in many cases of brow ptosis, it can be measured. There are many patients with ptosis on the facial nerve palsy side that have upper eyelid asymmetry with a lower facial nerve palsy eyelid. Furthermore, patients with blepharoptosis use the frontalis muscle in order to compensate for an impaired visual field. In this case, the brow can move upward. The brow on the facial nerve palsy side could be placed in a normal position, whereas the brow on the contralateral side may be placed in a higher position. In our study, 11 patients (35.5%) had brow ptosis on the facial nerve palsy side, and eight patients (25.8%) had the brow placed above the superior orbital rim on the contralateral side. We can infer that at least 19 patients (61.3%) had brow ptosis on the facial nerve palsy side. A high rate of brow ptosis can increase the rate of upper eyelid asymmetry (with the facial nerve palsy eyelid lower, and ptosis on the facial nerve palsy side).
It is noteworthy in our study that the mean MRD1 was smaller (p = 0.003), and the mean ΔMRD1 was larger (p = 0.001), in patients who had facial nerve palsy and another cranial nerve palsy. In other words, patients with facial nerve palsy and palsy of another cranial nerve presented severe upper eyelid asymmetry and ptosis. We can speculate that there were confounding effects caused by the paralytic ptosis of patients with third cranial nerve palsy. But when monitoring patients with facial nerve palsy only, there was still significant ptosis on the facial nerve palsy side. Thus, for patients with both facial nerve palsy and third cranial nerve palsy, the main cause of ptosis seems to be the facial nerve palsy.
We next studied certain unusual patient cases. For example, a male patient of 56 years had left facial palsy with pontine intracerebral hemorrhage. A corneal lesion induced by lagophthalmos, lower lid retraction, and entropion were not resolved, even after several lid surgeries. The patient underwent supratarsal fixation (upper lid : left eye), filler injection (lower lid : left eye), skin flap to lower lid graft (lower lid : left eye), and medial and lateral canthoplasty (left eye). But 10 years after the initial paralysis, his left upper lid covered the cornea. This was due to blepharoptosis related to the aging process, and the corneal lesion improved.
As a second example, a female patient of 70 years who suffered from Bell's palsy received a silicone tube insertion to treat a diagnosis of nasolacrimal duct narrowing with epiphora in her left eye. But there was no symptomatic improvement. Botulinum neurotoxin was injected at her left lacrimal gland to treat a diagnosis of hyperlacrimation one month after the operation. This resulted from facial nerve aberrant regeneration.
This was a retrospective study with a relatively small number of patients. As such, there was a difference in terms of sample selection (i.e., the group 1 : group 2 ratio) compared to other studies. The follow-up period varied from 1 month to 10 years, so it was not always easy to obtain data on symptomatic improvement or relapse. A prospective study with many more patients is needed.
Despite these limitations, our study demonstrated the importance of proactively performing invasive procedures to treat facial paralysis. Our data also indicated that the prognosis worsened when a patient had palsy of another cranial nerve. These findings are of significance.
In this study, we observed the ophthalmic signs and prognoses of facial nerve palsy patients. We compared the clinical outcomes of patients with simple facial palsy to patients also suffering from palsy of the cranial nerves. Asians have many differences to Westerners in their periorbital anatomical structures [5]. Understanding the ophthalmological clinical features of Asian facial palsy patients will help the ophthalmologist to diagnose and manage these patients, especially when treating ptosis and eyelid asymmetry.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Joseph SS, Joseph AW, Smith JI, et al. Evaluation of patients with facial palsy and ophthalmic sequelae: a 23-year retrospective review. Ophthalmic Epidemiol 2017;24:341-345.


2. Malhotra R, Ziahosseini K, Litwin A, et al. CADS grading scale: towards better grading of ophthalmic involvement in facial nerve paralysis. Br J Ophthalmol 2016;100:866-870.


3. Chi JJ. Management of the eye in facial paralysis. Facial Plast Surg Clin North Am 2016;24:21-28.


Fig.┬Ā1
Before and after injection of botulinum neurotoxin type A (BoNT-A) and hyaluronic acid. (A-F) The patients with only facial nerve palsy. (G,H) The patient with facial nerve palsy and other cranial nerve paralysis. (A) A 1-year-old male patient who had postpartum right facial nerve injury. (B) A 8-year-old male patient who had postpartum right facial nerve injury after 7 years of injection of BoNT-A and hyaluronic acid. (C) A 70-yearold female patient who had right facial nerve palsy. (D) A 70-year-old female patient who had right facial nerve palsy after 3 months of injection of BoNT-A and hyaluronic acid. (E) A 78-year-old male patient who had left facial nerve palsy. (F) A 78-year-old male patient who had left facial nerve palsy after 3 months of injection of BoNT-A and hyaluronic acid. (G) A 42-year-old male patient who had brain tumor surgery and had facial nerve palsy and other cranial nerve palsy. (H) A 42-year-old male patient who had brain tumor surgery and had facial nerve palsy and other cranial nerve palsy after 1 month of injection of BoNT-A at extraocular muscle and hyaluronic acid at left upper and lower lid. Informed consent was obtained from all study participants.

- TOOLS
-
METRICS

-
- 18 Crossref
- 0 Scopus
- 3,130 View
- 50 Download
- Related articles
-
Prevalence and Clinical Features of Sagging Eye Syndrome in Korean Patients2022 April;36(2)
Clinical Features of Duane Retraction Syndrome: A New Classification2020 April;34(2)
Clinical Features of Benign Essential Blepharospasm in Korean Patients2018 October;32(5)
Ophthalmologic Features of Lennox-Gastaut Syndrome2017 June;31(3)
Clinical Features of Ocular Trauma in Emergency Department.2004 June;18(1)






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



