Eyelid Swelling and Subconjunctival Infiltration as Ophthalmic Manifestations in a Child with Idiopathic Hypereosinophilic Syndrome
Article information
Dear Editor,
Hypereosinophilic syndrome (HES) is a rare eosinophilic disorder characterized by idiopathic hypereosinophilia (absolute eosinophil count >1,500 cells/µL for >1 month) with target organ damage [1]. Up to 50% of HES patients exhibit ocular manifestations, such as retinal/choroidal vessel occlusion and uveitis [1234]; however, pathologically proven eosinophilic infiltration of the eye has not been previously reported. Herein, we describe a 7-year-old girl with HES who presented with subconjunctival infiltration and recurrent upper eyelid swelling caused by eosinophilic infiltration.
The patient was referred to our clinic from the pediatric department to evaluate a conjunctival lesion and recurrent eyelid swelling. She had a history of recurrent genital swelling, chronic cough, and idiopathic hypereosinophilia (absolute eosinophil count 6,114 cells/µL) without a clear underlying cause. Her pediatrician had initiated empirical steroid therapy (0.8 mg/kg initially for 3 days and then a taper every 3 days) to control her hypereosinophilia before her visit to our clinic. At the initial examination, a yellowish infiltrative lesion was observed in the temporal conjunctiva of her left eye (Fig. 1A). However, the eyelid swelling had already improved. During the follow-up period, the subconjunctival infiltration and hypereosinophilia resolved while tapering her steroid dose. Thus, we discontinued steroid treatment. Two weeks after cessation of steroid therapy, eyelid swelling recurred with a palpable mass in her left eye (Fig. 1B); she exhibited no lymphadenopathy or abnormality on orbital computed tomography. Because of the relapsed hypereosinophilia (absolute eosinophil count: 13,629 cells/µL) and the ocular manifestations, the patient's pediatrician performed systemic evaluations, including echocardiography and liver function tests; there were no specific findings, except bone marrow hypereosinophilia. Therefore, we performed a biopsy of the eyelid mass to confirm tissue eosinophilia, which is essential for a definitive diagnosis of HES, in conjunction with the synchronous clinical course of ocular events and eosinophilia. Ocular events (subconjunctival infiltration/eyelid swelling) occurred when the absolute eosinophil count was >2.0 × 103 cells/µL and resolved when the eosinophilia improved. A whitish-yellow, semi-hard mass was located at the level of the preaponeurotic fat. Histopathological examination revealed dense eosinophilic infiltration (Fig. 1C, 1D), and a final diagnosis of HES was made. Since then, her pediatrician has treated her with hydroxyurea and oral steroids to control the blood hypereosinophilia.
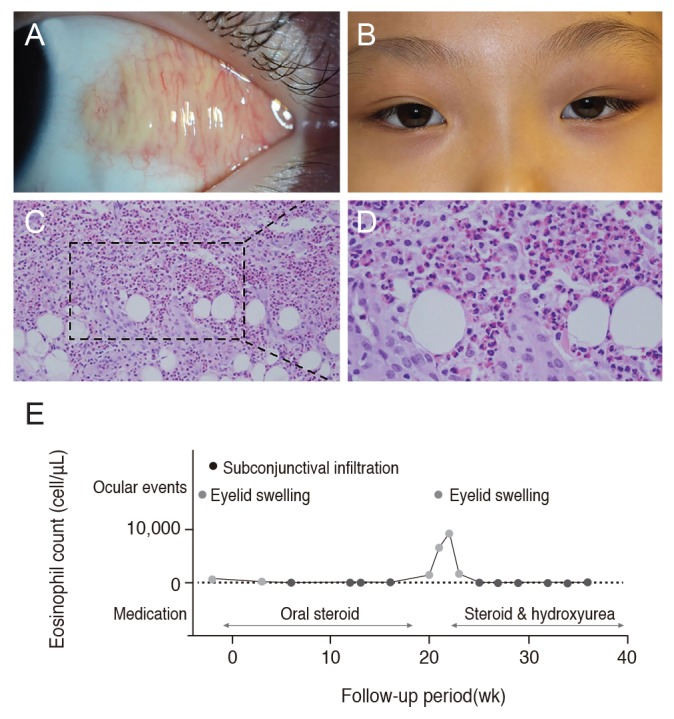
Ocular events and clinical course in a young girl with idiopathic hypereosinophilic syndrome. (A) A 7-year-old girl presenting with a yellowish subconjunctival infiltrative lesion in her left eye. (B) Two weeks after discontinuation of steroid treatment, newly developed left eyelid swelling, caused by a semi-hard mass, was observed. Informed consent has been obtained from patient for treatment and publication. (C,D). Histopathological examination of the tissue obtained from the mass, which was located at the level of the preaponeurotic fat pad, shows dense eosinophilic infiltration (the square magnified on the right shows infiltrating eosinophils in the mass). (C) H&E, ×20. (D) H&E, ×50. (E) Relationships among eosinophil count, ocular events, and immunosuppressive therapy. Ocular events (eyelid swelling and subconjunctival infiltration) occurred when the absolute eosinophil count was >2.0 × 103 cells/µL (red dots) and resolved when the eosinophilia improved (blue dots). This finding suggests that the ocular events were associated with eosinophilia and may provide an index of eosinophilia in patients with hypereosinophilic syndrome.
This 7-year-old girl was finally diagnosed with HES based on the following diagnostic criteria: eosinophilic infiltration in her eyelid and idiopathic hypereosinophilia for >6 months (Fig. 1E) [1]. Although she had a history of hypereosinophilia, we did not suspect eosinophil infiltration in the eyelid/conjunctiva because HES with eyelid swelling/mass/subconjunctival infiltration had not been previously reported in the literature.
Currently, the reported ocular manifestations of HES mainly consist of retinal/choroidal vessel occlusion secondary to systemic thromboembolic events [2]. Although uveitis [3] or retinal vasculitis [4] in HES (suggestive of direct eosinophil infiltration) has been reported, those cases were not pathology proven for tissue eosinophilia. To the best of our knowledge, this is the first report of pathologically proven ocular eosinophilic infiltration in a patient with HES.
Although HES was originally reported to have a poor prognosis [5], advances in treatment and early diagnosis have improved the survival rate. However, diagnosis in the early stage of this disease remains challenging because HES is a rare disease that manifests with various nonspecific symptoms such as weakness, chronic cough, and fever [1]. Furthermore, pathologic confirmation, which is essential for the diagnosis, is difficult in frequently involved organs (hematologic, cardiovascular, pulmonary, and gastrointestinal systems) [1]. In this case, eyelid biopsy played a pivotal role in our patient's diagnosis and treatment, as there was no other clinical evidence of eosinophilic target organ damage. Our findings suggest that HES can manifest as eyelid swelling and subconjunctival infiltration even when vital organ damage is not clinically evident.
Our findings suggest that ophthalmologists suspect ocular manifestations of HES in patients who present with hyper-eosinophilia and recurrent eyelid swelling or subconjunctival infiltration. A biopsy should also be considered in these cases for timely diagnosis and appropriate treatment.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.