 |
 |
| Korean J Ophthalmol > Volume 32(4); 2018 > Article |
Abstract
Purpose
To report the surgical results of unilateral pediatric cataracts from uncertain causes in relatively older children and to identify factors related to better visual outcomes.
Methods
We retrospectively evaluated the medical records of 39 patients who underwent surgery between the ages of 3 and 10 years for unilateral pediatric cataracts of no known cause. All patients underwent primary intraocular lens implantation and postoperative amblyopia treatment. A postoperative final visual acuity better than 20 / 30 was considered to be a good visual outcome.
Results
The mean age of patients was 6.0 ± 1.8 years at the time of surgery. The mean preoperative visual acuity was 1.07 ± 0.71 logarithm of the minimum angle of resolution (range, 0.15 to 3.00), while the mean final postoperative visual acuity was 0.47 ± 0.54 logarithm of the minimum angle of resolution (range, 0.00 to 2.00). Of 39 patients, 18 (46.2%) achieved a good visual outcome. Only the preoperative visual acuity maintained a significant association with a good visual outcome according to our multivariate analysis (p = 0.040). A preoperative visual acuity of 20 / 100 or better was found to increase the chance of achieving a good visual outcome by 13.79-fold (95% confidence interval, 1.13 to 167.58).
Despite developments in surgical techniques and intraocular lenses, the management of unilateral pediatric cataracts is still clinically challenging. Better visual outcomes are usually obtained with early surgical correction and vigorous amblyopia treatment [1,2,3,4]. The critical period for surgical treatment of unilateral congenital cataract was reported to be within the range of 6 to 17 weeks in several studies [1,2,3].
In general, pediatric cataract patients under three years of age who require surgery under general endotracheal anesthesia are referred to tertiary hospitals. However, screening tests for visual acuity are not easy to administer to patients who are less than three years old, and diagnoses of cataract are rare in clinical practice. Therefore, children with decreased visual acuity who have been diagnosed with cataract undergo cataract surgery much later than the reported critical period (between 6 and 17 weeks of age) for congenital cataract surgery. However, good postoperative visual function in pediatric cataract surgery requires careful surgical treatment, early correction of refractive errors, and rigorous attention to the postoperative treatment of amblyopia. Previous studies have reported that the prognosis of unilateral pediatric cataract is even less favorable [3,4]. The results of the surgery in our hospital, however, have not been always less favorable, even when the morphology of the cataracts indicates that they are congenital. The purpose of this study was to evaluate the results of surgery for unilateral pediatric cataract of uncertain cause in our hospital and to analyze factors related to a better visual outcome.
This retrospective study was conducted at the Department of Ophthalmology of Kim's Eye Hospital at Konyang University. The study protocol was approved by the institutional review board at Kim's Eye Hospital in Seoul, Korea (B-2011-001). All procedures conformed to the guidelines of the Declaration of Helsinki. Patients were informed of the study objectives and the examination processes and were asked to provide written consent. We retrospectively reviewed the medical records of patients who underwent surgery for pediatric cataract (age range, 3 to 10 years old) at Kim's Eye Hospital between 1 January 2001 and 31 December 2010. We identified 104 patients without history of previous intraocular surgery. Patients were excluded if they had bilateral cataracts, traumatic cataract, ocular abnormalities unrelated to cataract, or any developmental delays. Prospective patients were also excluded if their postoperative follow-up period was less than one year in length (Fig. 1).
Patients typically underwent cataract surgery within four months of diagnosis. Surgery was performed when the patient recognized decreased subjective and objective visual accuity due to cataract and after consulting with their parents. All surgeries were performed by one experienced surgeon (BYK). Under general anesthesia, anterior continuous curvilinear capsulorhexis, lens aspiration, posterior continuous curvilinear capsulorhexis, and anterior dry vitrectomy were performed through either a limbal or a scleral tunnel incision. An intraocular lens (IOL) is traditionally implanted in the capsular bag; in cases of polymethyl methacrylate IOL (Single-piece Polymethyl Methacrylate Posterior Chamber IOL 604A Rayner; Rayner, East Sussex, UK), the IOL optic was captured through a posterior continuous curvilinear capsulorhexis opening. In recent years, IOLs have been implanted in the sulcus to simplify later replacement. The power of the IOL was calculated using the SRK-II formula, and the target refraction was determined according to age and refractive error of the fellow eye and modified to minimize anisometropia. The refraction goals of IOL target diopters were adjusted according to age as follows: 3 to 5 years, +2 to +3; 5 to 7 years, +1 to +2; 7 to 10 years, plano to +1.00. The IOL target diopters were adjusted according to refractive error of the fellow eye, in addition, there was no more than ±1 diopter difference when the targeting diopters were more myopic compared with the fellow eye. The incision was closed with 10-0 nylon sutures.
Postoperatively, 0.3% tobramycin (Tobrex; Alcon, Fort Worth, TX, USA) and 0.1% fluorometholone (Ocumetholone; Allergan, Irvine, CA, USA) eye drops were administered four times daily for about one month. A large portion of patients took 10 mg of oral prednisolone (Solondo; Yuhan Medical, Seoul, Korea) for several days to control moderate to severe anterior chamber reaction in the immediate postoperative period.
We cooperated with two pediatric ophthalmologists for the amblyopia treatment of our patients. Spectacles with or without monocular occlusion were prescribed postoperatively. The number of patching hours ranged from six to all waking hours each day, and the maintenance level was modified on an individual basis according to visual acuity and age.
Visual acuity was measured at each visit using either a standard Snellen chart or a tumbling E chart for young illiterate children. Two patients (one male patient, 2 years 11 months old; one female patient, 1 year 7 months old) were unable to have their visual acuity checked preoperatively due to poor cooperation. Strabismus surgery was performed when needed. Data were collected with regard to gender, type of cataract, age at diagnosis, age at surgery, presence of strabismus, preoperative and postoperative visual acuity (best-corrected visual acuity) of each eye, preoperative and postoperative refractive error in each eye, axial length at surgery, amblyopia treatment, and follow-up period.
A final postoperative visual acuity better than 20 / 30 was considered a good visual outcome. We chose a cutoff point of 20 / 30, which was relatively high compared to other studies because visual acuity was sufficient only if it did not seriously disturb daily life. Patients were divided into either the Va (≥ 20 / 100) or the Vb (< 20 / 100) group according to preoperative visual acuity. Snellen acuity data were converted into the logMAR format for statistical analyses.
Univariate analysis using chi-square test, Fisher exact test, and Student's t-test was performed, and multiple logistic regression analysis was carried out to identify significant factors associated with good visual outcome. The SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA), was used for our statistical analysis, with statistical significance defined as p-values < 0.05.
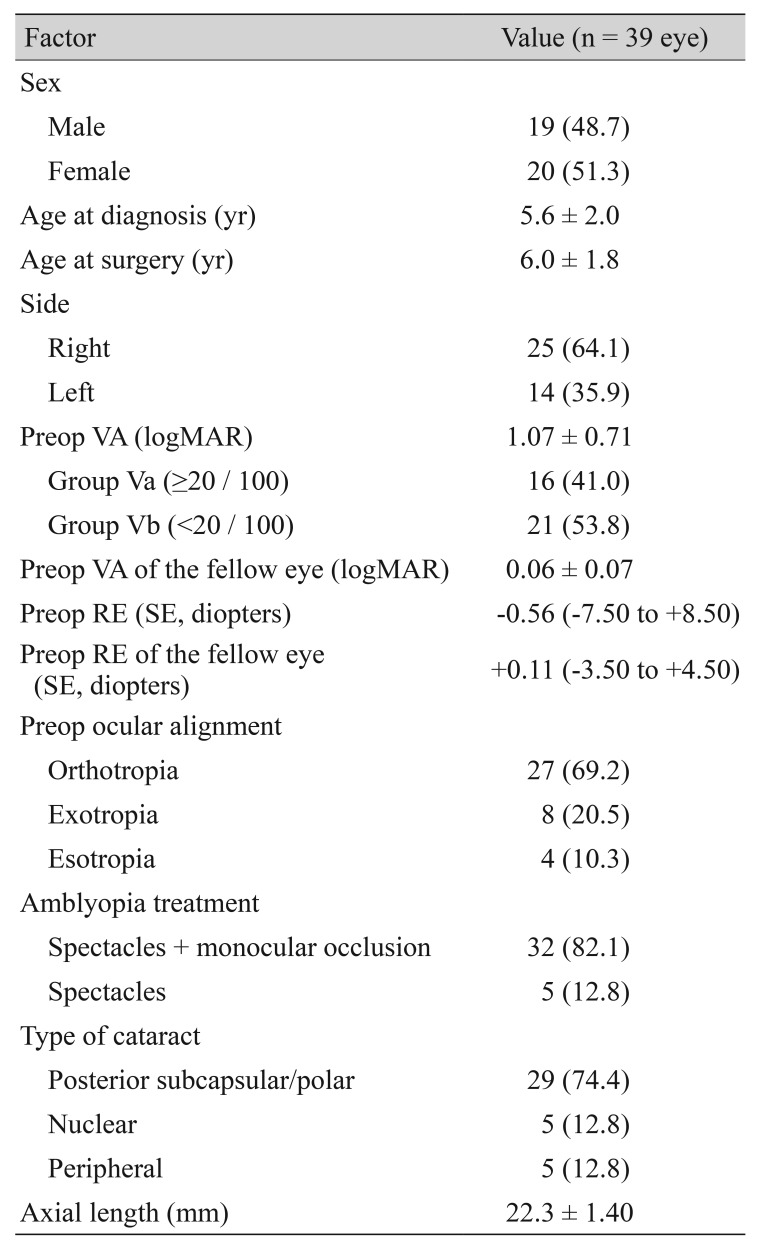
Thirty-nine patients were included in the data analysis after excluding 65 patients who were not eligible because of bilateral cataracts (40), traumatic cataract (18), ocular abnormality unrelated to cataract (2), developmental delay (1), and less than one year of follow-up (4) (Fig. 1). Table 1 shows the patient demographic data. The mean age at surgery was 6.0 ± 1.8 years (range, 3 to 10 years). The mean duration of follow-up after surgery was 3.9 ± 2.9 years (range, 1.0 to 10.3 years).
The mean final postoperative visual acuity was 0.47 ± 0.54 logarithm of the minimum angle of resolution (logMAR; range, 0.00 to 2.00) in the operated eye. Fig. 2 shows the changes in visual acuity in these eyes. Eighteen eyes (46.2%) of 39 patients achieved a good visual acuity of 20 / 30 or better. For the fellow eye, the mean final visual acuity was 0.02 ± 0.04 logMAR (range, 0.00 to 0.10). Twelve eyes with strabismus showed a mean final visual acuity of 0.73 ± 0.52 logMAR, 0.51 ± 0.34 logMAR in eight eyes with exotropia and 1.18 ± 0.57 logMAR in four eyes with esotropia. Strabismus surgery was eventually required in three children (two patients with esotropia and one patient with exotropia). Patients treated with a combination of monocular patching and spectacles achieved a mean final visual acuity of 0.55 ± 0.56 logMAR, while the acuity was 0.11 ± 0.17 logMAR with spectacles alone. Patching was not always tolerated well, especially in school-aged children.
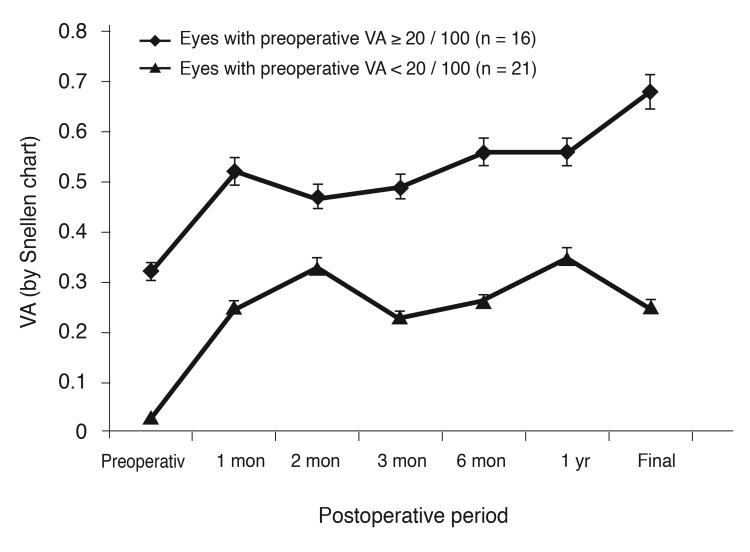
The mean target refraction was 0.90 ± 1.25 diopters (D; range, −1.21 to +3.50), and the mean final refractive error was −1.48 ± 2.97 D (range, −7.75 to +8.50) in the operated eye. Fig. 3 shows changes in refractive error in these eyes. The mean rate of refractive change per year was −0.65 D (range, −2.50 to +0.60). For the fellow eyes, the mean final refractive error was −0.85 ± 1.72 D (range, −6.50 to +2.50).
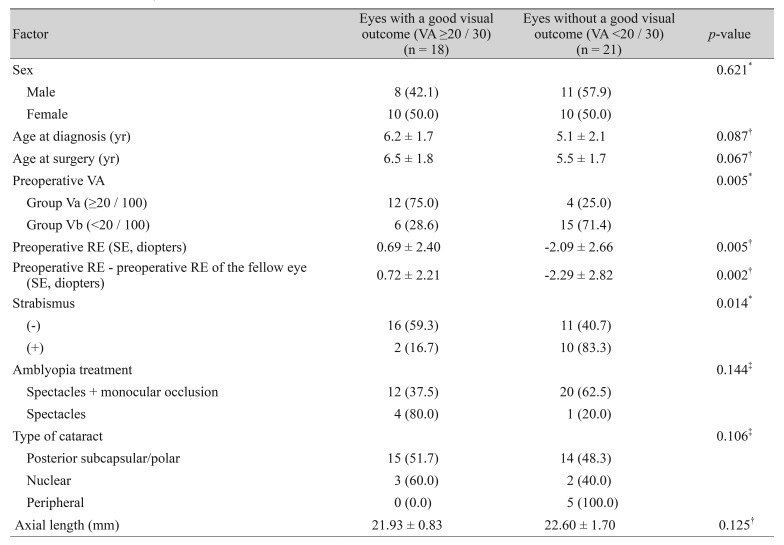
Table 2 shows the characteristics of patients who achieved or did not achieve good visual acuity (final postoperative visual acuity >20 / 30) and the results of a univariate analyses. A good visual outcome was significantly associated with better preoperative visual acuity, smaller preoperative refractive error, smaller difference in preoperative refractive errors between the operated and the fellow eyes, and absence of strabismus (p = 0.005, 0.005, 0.002, and 0.014, respectively). Preoperative refractive error was excluded from the multiple logistic regression analysis to reduce multicollinearity. The other three variables and “age at surgery,” which are known to have a decisive effect on surgical outcome, were also included in the analysis. Only preoperative visual acuity remained significant (p = 0.040) (Table 3). Twelve (66.7%) of the 18 patients with a good visual outcome had a preoperative visual acuity of 20 / 100 or better. Patients with a preoperative visual acuity of 20 / 100 or better had a 13.79-fold increased chance of achieving good visual acuity compared to those with a preoperative visual acuity <20 / 100 (95% confidence interval, 1.13 to 167.58). Fig. 4 illustrates this tendency.
An exudative membrane in the anterior chamber either with or without posterior synechia developed in nine eyes (23.1%) in the immediate postoperative period. This problem resolved rapidly without any further complications with systemic steroid treatment for one or two weeks. No other postoperative complications were recognized.
There are plenty of arguments about the best age for congenital cataract surgery, and earlier surgery is generally accepted to have a positive correlation with a better visual outcome, especially in eyes with unilateral pediatric cataract [1,2,3,4,5,6]. The critical period for this type of surgery has been reported to be from 6 to 17 weeks of age in several studies [1,2,3]. In clinical practice, however, ophthalmologists often encounter older children with unilateral cataracts for whom the critical period for surgery has already passed. If it is the children's first visit to an ophthalmology clinic, it is not easy to determine if the cataract is congenital or developmental. Patients in this study also had no history of ocular trauma or other ophthalmic problems, which made the onset and cause of cataracts unclear. The appearance of lens opacities suggested that they were congenital or developmental. Nevertheless, contrary to the aforementioned studies, nearly half of these patients achieved a good postoperative visual acuity of 20 / 30 or better.
Several studies on pediatric cataracts have achieved good postoperative visual acuity even after late surgeries. Zwaan et al. [7] showed visual acuities of 20 / 40 or better in 44% of eyes, visual acuities of 20 / 50 to 20 / 80 in 27% of eyes, and better visual acuity in children older than four years of age (p = 0.001) despite their inclusion of traumatic and secondary cataracts. The posterior capsular bag IOL of cataract surgery has resulted in good visual acuity (20 / 40 or better in 85.3%) in both unilateral and bilateral developmental and traumatic cataract patients over the age of two years [8]. In unilateral cataract cases, visual acuity was 20 / 50 or better in 74% of eyes; a best corrected visual acuity of 20 / 30 or better was achieved in 95% of eyes in bilateral cataract cases [9]. In a retrospective study of 139 eyes with pediatric cataract, the mean visual acuity was better in bilateral versus unilateral cases (p < 0.001), and that study found that an older age at surgery was correlated with a better visual acuity outcome in both unilateral and bilateral cases [10]. Early surgery was not a prerequisite for a good postoperative outcome in past studies or in the current study, which might be because the lens opacities started to develop after the critical period of visual development or were not significant during that period. The patients whose cataracts were already severe during infancy were more likely to be discovered earlier. The strabismus proportion was 30.8% in this study, which was much lower than the rate reported by others [3]. Our findings also suggest that lens opacities were not severe enough to disturb ocular alignment, which could be one of the reasons caregivers only belatedly took their children to the clinic. Moreover, Fig. 2 indicates that the postoperative visual acuity mostly improved during the first postoperative month but made less progress after. This result implies that low preoperative visual acuity resulted from lens opacity rather than amblyopia, and the depth of amblyopia was not that severe.
The reported predictors of visual outcome in unilateral pediatric cataracts are age at surgery, preexisting nystagmus and strabismus, refractive error, compliance with amblyopia therapy, cataract type, and interocular axial length difference [1,2,3,4,5,11,12,13,14]. Preoperative visual acuity was the only factor that affected the surgical outcome for unilateral pediatric cataractin patients over three years old in this study (p = 0.040); in our study, patients with preoperative visual acuity of 20 / 100 or better had a 13.79-fold increased chance of achieving good visual acuity compared to those with preoperative visual acuity <20 / 100. That is, in the presence of good preoperative visual acuity, the visual outcome might be satisfactory even after the known critical period for congenital cataract surgery. Strabismus was not an affecting factor in our multivariate analysis. However, strabismus was found preoperatively in only 2 children out of 18 who achieved a good postoperative visual outcome; 4 children with esodeviation demonstrated a postoperative visual acuity <20 / 30. Weisberg et al. [11] and Lambert et al. [12] showed that preoperative strabismus was a clinical indicator of impending dense amblyopia and indicated a compromised visual prognosis in unilateral cataract. Our experience with pediatric cataract surgery was in agreement with these findings. Therefore, the results of a multivariate analysis indicated that preoperative visual acuity affects surgical outcome even after excluding the effect of strabismus.
Cataract type showed no significant effect on postoperative visual outcome, which was contrary to the report of Parks et al. [5]. The extent of lens opacity and the degree of obscuring visual axis appeared to be more influential than the type of cataract. Amblyopia treatment did not influence visual outcome in this study, but the study was limited in two points from drawing this conclusion. First, the immediate postoperative visual acuities of those who did not need monocular occlusion or spectacles were already satisfactory. Second, many children had trouble maintaining occlusion therapy, especially school-aged children; therefore, the accurate measurement of compliance with occlusion therapy was not possible in this retrospective study. Unfortunately, interocular axial length difference data were not available in this study because the axial length of the fellow eye was not measured in many cases.
Late surgery for pediatric cataract has the advantage of being performed with simultaneous IOL implantation. Posterior chamber IOL implantation has been reported to provide a better visual outcome than lensectomy followed by contact lens use in unilateral pediatric cataract [10,15,16]. Moreover, pseudophakic eyes show a lesser rate of myopic shift and a lower incidence of glaucoma than aphakic eyes [17,18,19]. The second advantage is that older children undergo less myopic shift resulting from changes in axial length [9,20]. In other words, the target refraction can be determined close to the emmetropia, which aids in amblyopia treatment. Finally, visual acuity could be checked more accurately. Thirty-seven of 39 children had their visual acuity checked using either a Snellen chart or a tumbling E chart preoperatively, and the other two were also cooperative after the surgery.
We are unaware of any previous reports that focused on only unilateral pediatric cataract of no known cause and that was past the critical period for cataract surgery. Our study found that almost half of the patients achieved a good postoperative visual outcome even after this critical period, and the most important predicting factor for surgical outcome was preoperative visual acuity. The result may be helpful in treating and counseling patients with unilateral pediatric cataract after three years of age.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Drummond GT, Scott WE, Keech RV. Management of monocular congenital cataracts. Arch Ophthalmol 1989;107:45-51.


2. Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci 1996;37:1532-1538.


3. Lundvall A, Kugelberg U. Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scand 2002;80:588-592.


4. Allen RJ, Speedwell L, Russell-Eggitt I. Long-term visual outcome after extraction of unilateral congenital cataracts. Eye (Lond) 2010;24:1263-1267.


5. Parks MM, Johnson DA, Reed GW. Long-term visual results and complications in children with aphakia. A function of cataract type. Ophthalmology 1993;100:826-840.


6. You C, Wu X, Zhang Y, et al. Visual impairment and delay in presentation for surgery in chinese pediatric patients with cataract. Ophthalmology 2011;118:17-23.


7. Zwaan J, Mullaney PB, Awad A, et al. Pediatric intraocular lens implantation. Surgical results and complications in more than 300 patients. Ophthalmology 1998;105:112-118.


8. Crouch ER Jr, Pressman SH, Crouch ER. Posterior chamber intraocular lenses: long-term results in pediatric cataract patients. J Pediatr Ophthalmol Strabismus 1995;32:210-218.


9. Crouch ER, Crouch ER Jr, Pressman SH. Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. J AAPOS 2002;6:277-282.


10. Ledoux DM, Trivedi RH, Wilson ME Jr, Payne JF. Pediatric cataract extraction with intraocular lens implantation: visual acuity outcome when measured at age four years and older. J AAPOS 2007;11:218-224.


11. Weisberg OL, Sprunger DT, Plager DA, et al. Strabismus in pediatric pseudophakia. Ophthalmology 2005;112:1625-1628.


12. Lambert SR, Lynn M, Drews-Botsch C, et al. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. J AAPOS 2001;5:70-75.


13. Gochnauer AC, Trivedi RH, Hill EG, Wilson ME. Interocular axial length difference as a predictor of postoperative visual acuity after unilateral pediatric cataract extraction with primary IOL implantation. J AAPOS 2010;14:20-24.


14. Lal G, Trivedi RH, Wilson ME Jr, et al. Interocular axial length difference in eyes with pediatric cataracts. J AAPOS 2005;9:358-362.


15. Congdon NG, Ruiz S, Suzuki M, Herrera V. Determinants of pediatric cataract program outcomes and follow-up in a large series in Mexico. J Cataract Refract Surg 2007;33:1775-1780.


16. Greenwald MJ, Glaser SR. Visual outcomes after surgery for unilateral cataract in children more than two years old: posterior chamber intraocular lens implantation versus contact lens correction of aphakia. J AAPOS 1998;2:168-176.


17. McClatchey SK, Dahan E, Maselli E, et al. A comparison of the rate of refractive growth in pediatric aphakic and pseudophakic eyes. Ophthalmology 2000;107:118-122.


18. Superstein R, Archer SM, Del Monte MA. Minimal myopic shift in pseudophakic versus aphakic pediatric cataract patients. J AAPOS 2002;6:271-276.


Fig. 2
Changes in visual acuity in all eyes. The mean final postoperative visual acuity was 0.34 ± 0.29 (0.47 ± 0.54 logarithm of the minimum angle of resolution) in the operated eye. Visual acuity was mostly improved during the first postoperative month. Error bars indicate standard deviation.

Fig. 3
Changes in refractive error. The mean refractive error was 0.12 ± 2.51 diopters (D) one year postoperatively, and the mean final refractive error was −1.48 ± 2.97 D in the operated eye. The mean rate of refractive change per year was −0.65 D. Error bars indicate standard deviation.
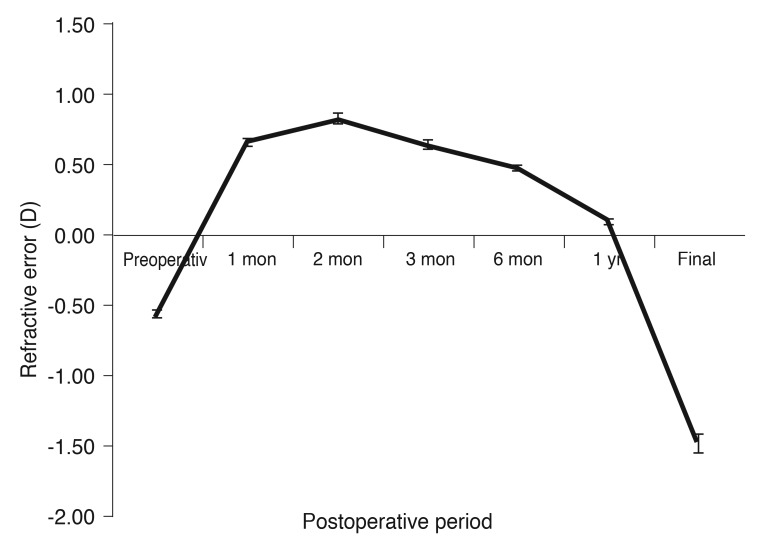
Fig. 4
A comparison of changes in visual acuity (VA) according to the preoperative VA. Patients with a preoperative VA of 20 / 100 or better had an increased chance of achieving a good visual outcome compared to those with a preoperative VA less than 20 / 100. Error bars indicate standard deviation.
- TOOLS
-
METRICS

-
- 2 Crossref
- 0 Scopus
- 2,416 View
- 22 Download
- Related articles
-
Clinical Characteristics and Outcomes of Cataract Surgery in Highly Myopic Koreans2011 April;25(2)





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



