Transscleral suturing is a well-established and effective technique for fixation of posterior chamber intraocular lenses (IOLs) in the absence of sufficient capsular support. Many transscleral suture fixation techniques have been developed, but many of them require intricate surgical maneuvers and are associated with an increased risk for surgical trauma. When it was first reported in 1986, transscleral suture fixation required large incisions that could cause significant surgically-induced astigmatism [
1]. Since then, many improvements have been made regarding the method of suture insertion through the sclera, suture fixation on the haptic, insertion of the IOL, and avoidance of suture erosion [
2].
Previously, we reported our method of temporarily externalizing the haptics through two corneal incisions 180 degrees apart and creating a loop suture on each haptic [
3]. This method is advantageous in that it allows stabilization of the IOL in the anterior chamber with little trauma to the eye, easier identification of the sutures, and thus minimal tangling. This method can be used in dropped IOLs as well as in situations where a new IOL insertion is required. Conventionally used three-piece IOLs can be used with the same usual injector through a small conventional clear corneal incision (CCI) during cataract surgery.
Still, there are some obstacles to overcome for successful transscleral fixation of the IOL. Asymmetric fixation at each haptic can occur, causing IOL decentration and tilting that result in postoperative astigmatism, which can be difficult to correct with glasses [
4]. Furthermore, breakage of polypropylene sutures, the most common cause of reoperation, has been reported to occur in up to 6% to 24% of previous transscleral IOL fixation over a follow up of 5 to 10 years and is more frequent in children [
5,
6]. In order to increase stability with less risk of decentration and tilting, four points of fixation have been used from as early as 1994 [
7,
8,
9,
10,
11,
12,
13,
14,
15,
16]. However, this technique can be associated with greater risk of complications from multiple suture passes through the sclera, uvea, and vitreous cavity. Recently, with the wider usage of small-gauge vitrectomy, total vitrectomy can be performed more easily with less sclerotomy-related complications, thus decreasing the possibilities of these complications related to the passage of sutures through the vitreous cavity.
Therefore, we modified our temporary haptic externalization technique to enhance IOL stabilization and decrease IOL dislocation from suture breakage by suture fixation at two points on each haptic, i.e., a four-point fixation for IOL scleral fixation. We evaluated the surgical outcome of this new technique and its effect on surgically-induced astigmatism and compared it with the outcome of the conventional single-point haptic fixation technique.
Materials and Methods
Patient enrollment
Patients that underwent four-point transscleral fixation of the IOL for insufficient capsular bag support at Seoul National University Hospital between August 2012 and December 2012 were retrospectively reviewed. For comparison with the conventional two-point fixation technique, retrospective review of patients that underwent scleral fixation with the conventional two-point fixation technique with temporary haptic externalization from March 2013 to December 2013 by the same surgeon (HJW) was performed. The study protocol was approved by the institutional review board of Seoul National University Hospital, and the study conformed to the Declaration of Helsinki. All patients gave their written informed consent before participation in the study. Patients that were identified to have inadequate capsular support on preoperative assessment by slit lamp biomicroscopy underwent transscleral fixation of the IOL. Along with assessment of the preexisting condition that warranted transsceral fixation of the IOL, preoperative refractive error measurement with keratorefractometer (KR 8900, Topcon, Tokyo, Japan) and corneal topography measurement with Orbscan II (Bausch & Lomb, Claremont, CA, USA) were performed. Any patients with preexisting ocular diseases that could compromise vision or conditions that could interfere with the measurement of refractive error or corneal topography were excluded.
Surgical technique
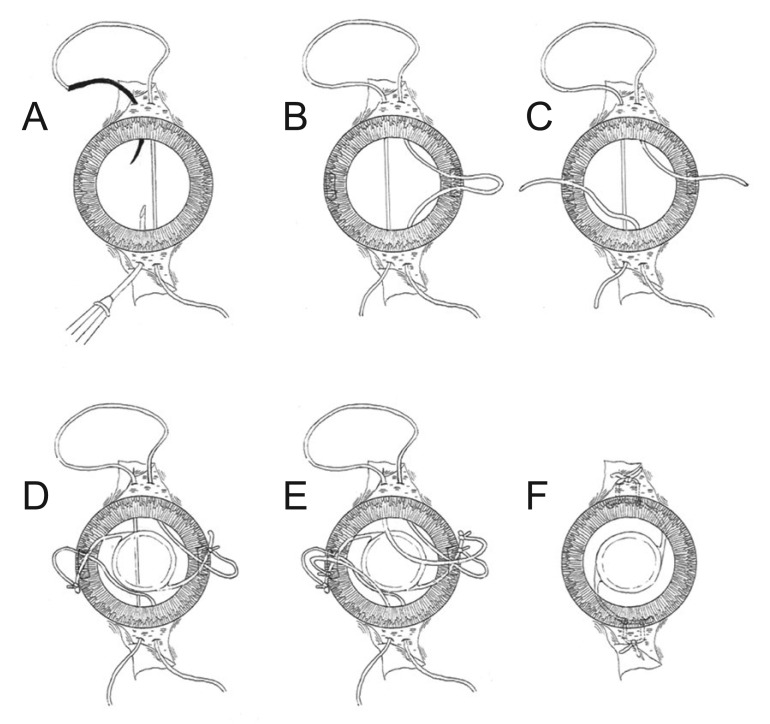
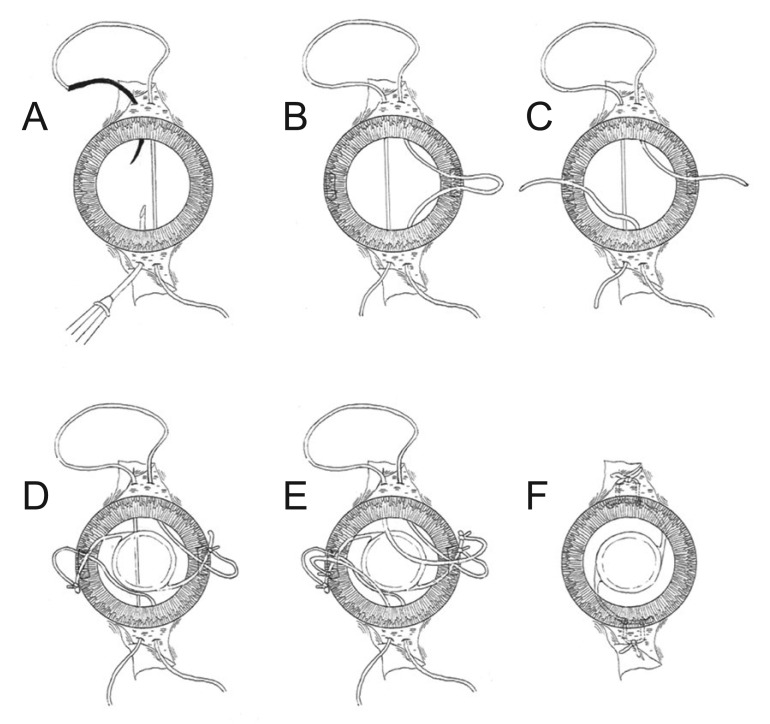
A conjunctival peritomy is created at 12 and 6 o'clock, respectively. Two points, 2 mm from the corneal limbus and 2 mm from each other are marked symmetrically at 12 and 6 o'clock. Double-armed 10-0 polypropylene sutures with two long curved needles on each end are passed through the sclera at the markings and across to the opposite side using a second hallow 26-guage needle for passage, so that two 10-0 polypropylene sutures are passing parallel from 12 to 6 o'clock (
Fig. 1A). Then, a 2.75-mm CCI is created at 3 and 9 o'clock. The suture thread closer to the 3 o'clock side is pulled through the 3 o'clock corneal incision (
Fig. 1B) and cut in two. Then, the 12 o'clock end is pulled out through the 9 o'clock CCI, so that the 6 o'clock strand remains through the 3 o'clock incision, and the 12 o'clock strand exits the 9 o'clock incision (
Fig. 1C). A 3-piece foldable IOL is inserted through the 3 o'clock corneal incision site into the anterior chamber. At this time, the leading haptic is guided out through the opposite 9 o'clock CCI with McPherson forceps. In cases of dropped IOLs, the previous IOL can be used if it is not damaged and should be elevated into the anterior chamber at the beginning of the procedure before the polypropylene sutures are placed. The haptics should be pulled out through the 3 and 9 o'clock incisions at this point. The previously passed sutures are tied securely to each haptic; the 6 o'clock suture at the 3 o'clock incision is tied 2.5 mm from the haptic tip, while the 12 o'clock suture passed through the 9 o'clock incision is tied 0.5 mm from the haptic tip (
Fig. 1D). Then, the other suture is pulled through the 3 o'clock incision and cut, and the 12 o'clock side is pulled out the 9 o'clock incision. Next, the 6 o'clock suture at the 3 o'clock incision is tied 0.5 mm from the haptic tip, while the 12 o'clock suture at the 9 o'clock incision is tied 2.0 mm from the haptic tip, so that the sutures are placed as in
Fig. 1E. The IOL is inserted into the anterior chamber and then into the posterior cavity while gently pulling the sutures at 6 and 12 o'clock, ensuring that they are not tangled (
Fig. 1F). After IOL centering is assessed, the two sutures at 12 and 6 o'clock are tied. The suture knots are buried under the conjunctiva, and the incised conjunctiva is repaired with an 8-0 polyglactin suture.
Postoperative examination and comparison with the conventional two-point fixation technique
Postoperative follow-up was conducted at 1 week, 1 month, 3 months, and 6 months after the operation and as needed thereafter. At each visit, best-corrected visual acuity, refractive error, position of the fixed IOL, and postoperative complications were evaluated. Total astigmatism in the refractive error and corneal astigmatism measured by topography at postoperative 6-month follow-up were used to calculate the lens astigmatism by the method previously described by Munoz-Escriva and Furlan [
17], that is,
S+CŌĆćsin2╬▒ŌłÆCsinŌĆć╬▒cosŌĆć╬▒ŌłÆCsinŌĆć╬▒cosŌĆć╬▒S+CŌĆćsin2╬▒
in the standard notation spherical value (S) / cylinderic value (C) ├Ś axis (╬▒). The postoperative corneal astigmatism was replaced by preoperative corneal astigmatism. The patients were followed thereafter according to the treating physician's discretion, and any occurrence of long-term complications was documented.
Statistical analysis
Statistical analyses were performed with IBM SPSS ver. 21 (IBM Corp., Armonk, NY, USA). Mann-Whitney's U-test was used for comparison of continuous variables between the two groups. A p-value <0.05 was considered statistically significant.
Results
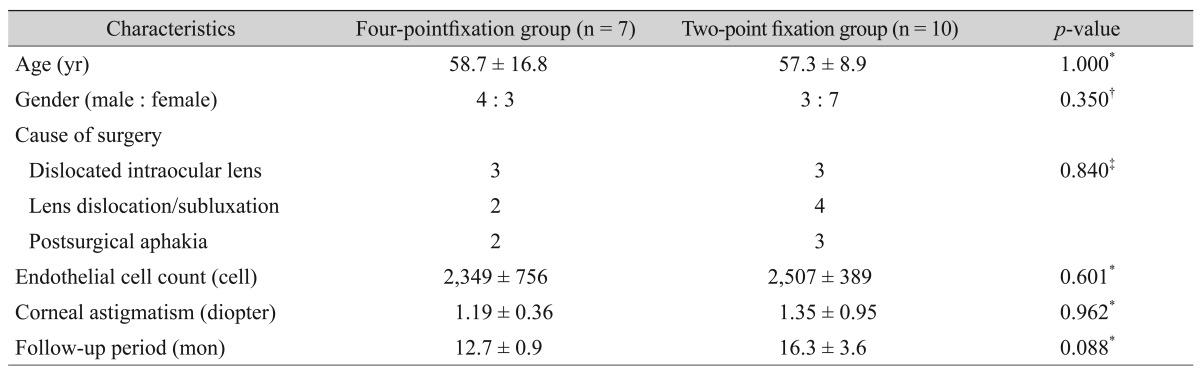
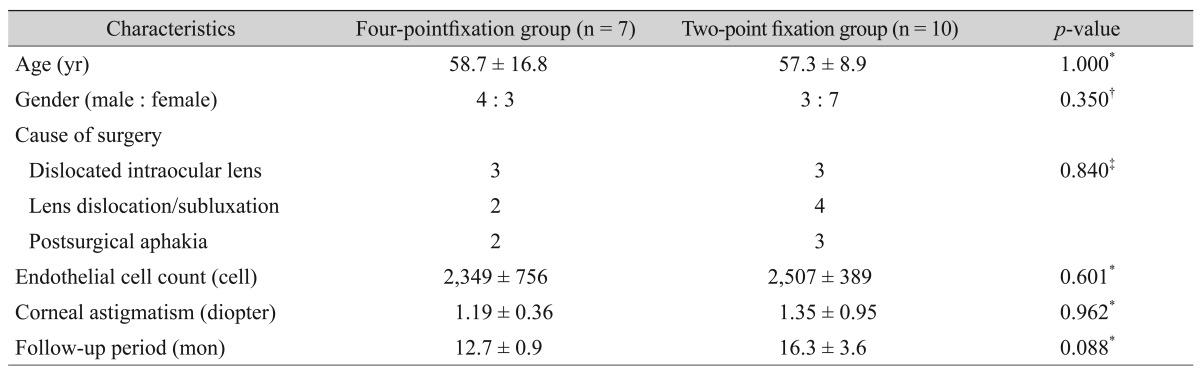
The demographic characteristics of the patients included are shown in
Table 1. Among the 7 patients that underwent four-point fixation, 3 required surgery for dislocated IOLs, 2 for crystalline lens dislocation/subluxation, and 2 for postsurgical aphakia. In the 10 patients that underwent two-point fixation, there were 3 patients with dislocated IOL, 4 patients with crystalline lens dislocation/subluxation, and 3 patients with postsurgical aphakia. All patients showed good centering with stable IOLs at the immediate postoperative period.
Table 2 shows the postoperative astigmatism according to surgical method. Postoperatively, total refractive astigmatism was significantly smaller in the four-point fixation group; 1.00 ┬▒ 0.50 diopters (D) versus 1.80 ┬▒ 0.84 D in the two-point fixation group (
p = 0.033). Corneal astigmatism was similar among the two groups; 1.19 ┬▒ 0.36 D in the four-point fixation group and 1.35 ┬▒ 0.95 D in two-point fixation group (
p = 0.962). The difference was larger with the calculated lens-induced astigmatism, at 1.17 ┬▒ 0.70 D in the four-point fixation group and 2.22 ┬▒ 0.98 D in the two-point fixation group (
p = 0.043).
One patient in the four-point fixation group and one in the two-point fixation group experienced recurrent capture of the optic of the IOL, which required repositioning. Another patient in the four-point fixation group and another patient in the two-point fixation group experienced one event of capture of the optic of the IOL, which resolved spontaneously in both patients. Otherwise, there were no other complications such as suture breakage, IOL dislocation, retinal detachment, cystoid macular edema, increased intraocular pressure, or endophthalmitis.
Discussion
In the continuously-evolving techniques of transscleral suturing of posterior chamber IOLs, the common goals have been reducing the incision size, minimizing tilting and de-centering, increasing the longevity of the polypropylene suture, minimizing complications, and simplifying surgical manipulation in order to decrease trauma to the eye. Our newly developed method of temporary haptic externalization and four-point fixation addresses all of these goals.
The whole procedure can be carried out with only two small CCIs, which enables maintenance of the eye with minimal intraoperative hypotony. This is especially important in vitrectomized eyes, which can easily lose pressure through large scleral incisions. Also, small incision size has advantages in that it can minimize incision-induced astigmatism, as in our previous report [
3]. Usually, no sutures are required for these clear corneal wounds, if created properly, as for CCI for phacoemuslification. This is especially advantageous in cases of insufficient zonular support discovered intraoperatively during cataract surgery, as there is no need for extension of the previously made CCI, although another CCI needs to be created on the opposite side.
The major advantage of fixing the IOL at four points is increased stability and decreased tilt. Our procedure was more effective in minimizing astigmatism resulting from tilting of the IOL and thus decreasing overall refractive astigmatism compared to the conventional two-point fixation technique. This effect results from fixation of sutures at two separate points 2 mm apart on each haptic. The majority of previously reported methods of four-point fixation are limited in that, although four-points in the sclera are punctured, the sutures are tied at the same place on the haptics, usually an eyelet, which is truly not a four-point fixation [
7,
10,
11,
12,
14]. Other previously reported truly four-point fixation techniques used specialized IOLs with two eyelets on each haptic, two perforation channels in each haptic, or four separate haptics [
8,
9,
13,
15,
16]. Another benefit of this method is the decreased dependency on the design of the IOL; any conventional foldable IOL can be used, although three-piece IOLs with sturdy haptics such as polymethylmethacrylate are preferred. Also, in cases of dropped IOL, the previously inserted IOL can be used if there is no damage to the haptics. This is very advantageous in cases with polymethylmethacrylate one-piece IOLs, which are impossible to remove without a large incision.
Since the polypropylene suture is tied on the haptic at two separate points, there can also be an advantage in the case of suture breakage. Usually, in two-point fixation, breakage of one suture results in posterior tilting into the vitreous cavity. However, with two separate sutures on each haptic, both sutures have to break in order to result in dislocation of the IOL, which can increase the longevity of the fixated IOL. Also, distributing the tensile strength on four strands rather than two strands might contribute to decreasing the rate of suture breakage. The long-term effect of this procedure on the rate of suture breakage remains to be clarified in future studies.
There were very few immediate postoperative complications with this method, which reflects the simplicity of the procedure and the limited trauma to the eye. Tying the suture on the haptic while it is externalized through a CCI can be advantageous in increasing the stability of the procedure, as previously reported. The complication rate of the four-point fixation technique was shown to be similar to that of the two-point fixation technique in this study. By separating the two haptics and retaining them in two CCIs 180 degrees apart, entangling of the sutures can be avoided, and the complexity of tying four sutures can be reduced. In all cases, complete vitrectomy was performed, considering the advantage in decreasing complications resulting from multiple passages of sutures through the vitreous vitreous. In eyes with minimal vitreous support, maintaining the IOL in a stable position during manipulation is of increased significance. Although tying four sutures can be complicated and a learning period might be required, this method is simpler than other four-point fixation methods while maintaining or enhancing its benefits.
There are shortcomings of this study in that the follow-up was short. The final IOL position such as tilting or decentration determined through ultrasound biomicroscopy was not analyzed because of the retrospective study characteristics. The preoperative astigmatism type, with-the-rule or against-the-rule, and IOL tilt-induced astigmatism also could not be compared due to the small number of subjects included. In addition, the postoperative corneal astigmatism was regarded as preoperative corneal astigmatism due to lack of postoperative followup examination. Further study with long-term follow-up, large number of subjects, evaluation about precise astigmatism, and IOL position is warranted.
In spite of these limitations, this new method of temporary haptic externalization and four-point IOL scleral fixation showed minimized tilting of the IOL with good intraoperative stability and minimal complications with a simplified procedure using small CCIs and conventional foldable IOLs. This procedure also raises the possibility less IOL dislocation due to suture breakage.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Malbran ES, Malbran E Jr, Negri I. Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction.
Int Ophthalmol 1986;9:151-160.


2. Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support.
Surv Ophthalmol 2005;50:429-462.


3. Kim DH, Heo JW, Hwang SW, et al. Modified transscleral fixation using combined temporary haptic externalization and injector intraocular lens implantation.
J Cataract Refract Surg 2010;36:707-711.


4. Hayashi K, Hayashi H, Nakao F, Hayashi F. Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans-scleral suture fixation surgery.
Ophthalmology 1999;106:878-882.


5. Asadi R, Kheirkhah A. Long-term results of scleral fixation of posterior chamber intraocular lenses in children.
Ophthalmology 2008;115:67-72.


6. McAllister AS, Hirst LW. Visual outcomes and complications of scleral-fixated posterior chamber intraocular lenses.
J Cataract Refract Surg 2011;37:1263-1269.


7. Bergren RL. Four-point fixation technique for sutured posterior chamber intraocular lenses.
Arch Ophthalmol 1994;112:1485-1487.


8. Teichmann KD, Teichmann IA. Haptic design for continuous-loop, scleral fixation of posterior chamber lens.
J Cataract Refract Surg 1998;24:889


9. Cordoves L, Gomez A, Mesa CG, Abreu JA. Sulcus transscleral sutured posterior chamber lenses.
J Cataract Refract Surg 1999;25:156-157.

10. Chakrabarti A, Gandhi RK, Chakrabarti M. Ab externo 4-point scleral fixation of posterior chamber intraocular lenses.
J Cataract Refract Surg 1999;25:420-426.


11. Azar DT, Wiley WF. Double-knot transscleral suture fixation technique for displaced intraocular lenses.
Am J Ophthalmol 1999;128:644-646.


12. Rao SK, Gopal L, Fogla R, et al. Ab externo 4-point scleral fixation.
J Cataract Refract Surg 2000;26:9-10.


13. Sewelam A. Four-point fixation of posterior chamber intraocular lenses in children with unilateral aphakia.
J Cataract Refract Surg 2003;29:294-300.


14. Lin CP, Tseng HY. Suture fixation technique for posterior chamber intraocular lenses.
J Cataract Refract Surg 2004;30:1401-1404.


15. Fass ON, Herman WK. Sutured intraocular lens placement in aphakic post-vitrectomy eyes via small-incision surgery.
J Cataract Refract Surg 2009;35:1492-1497.


16. Fass ON, Herman WK. Four-point suture scleral fixation of a hydrophilic acrylic IOL in aphakic eyes with insufficient capsule support.
J Cataract Refract Surg 2010;36:991-996.


17. Munoz-Escriva L, Furlan WD. Statistical analysis when dealing with astigmatism: assessment of different spherocylindrical notations.
Ophthalmic Epidemiol 2001;8:27-37.


Fig.┬Ā1
Schematic drawing of the procedure of temporary haptic externalization and four-point fixation in scleral fixation of the intraocular lens (surgeon's view from the superior of eye). (A) Double-armed 10-0 polypropylene sutures are passed through the sclera and across to the opposite side. (B) The suture thread closer to the 3 o'clock side is pulled through the 3 o'clock corneal incision and cut in two. (C) 12 o'clock end is pulled out through the 9 o'clock corneal incision. (D,E) A 3-piece intraocular lens is inserted through the 3 o'clock corneal incision site. The haptics should be pulled out through the 3 and 9 o'clock incisions. The previously passed sutures are tied to each haptic. (F) The intraocular lens is inserted into the anterior chamber and then into the posterior cavity while gently pulling the sutures at 6 and 12 o'clock.
Table┬Ā1
Demographic characteristics of patients
Table┬Ā2
Analysis of postoperative astigmatism in patients according to fixation technique

 in the standard notation spherical value (S) / cylinderic value (C) ├Ś axis (╬▒). The postoperative corneal astigmatism was replaced by preoperative corneal astigmatism. The patients were followed thereafter according to the treating physician's discretion, and any occurrence of long-term complications was documented.
in the standard notation spherical value (S) / cylinderic value (C) ├Ś axis (╬▒). The postoperative corneal astigmatism was replaced by preoperative corneal astigmatism. The patients were followed thereafter according to the treating physician's discretion, and any occurrence of long-term complications was documented.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






