Blindness in Sweet's Syndrome
Article information
Dear Editor,
Acute neutrophilic dermatosis, also known as Sweet's syndrome, is an uncommon inflammatory disorder characterized by the abrupt appearance of painful, edematous, and erythematous papules, plaques, or nodules on the skin [1]. Sweet's syndrome develops frequently in patients with hematologic disorders such as acute myeloblastic leukemia, diffuse large B-cell lymphoma, and myelodysplastic syndrome [2]. Ocular inflammation is a common extracutaneous manifestation of Sweet's syndrome. Various ocular manifestations have been reported previously, but blindness has not been described as a manifestation of Sweet's syndrome. We report the first case of blindness in association with Sweet's syndrome in Korea [345].
A 40-year-old man presented to our emergency room with pain, swelling, and redness of the left eye that lasted 10 days. He had been diagnosed with idiopathic thrombocytopenic purpura 8 years prior, but was lost to follow-up.
On admission, his body temperature was 38.3℃ and laboratory analysis revealed a hemoglobin level of 9.6 g/dL (reference range, 12.6 to 17.7), platelet count of 65,000/µL (140,000 to 415,000), and C-reactive protein level of 11.23 mg/L (0.00 to 8.00). Serological investigations, including those for human immunodeficiency virus, yielded negative or normal results.
His corrected visual acuities were 12 / 20 in the right eye and no light perception in the left eye, with intraocular pressures of 10 and 18 mmHg, respectively. The left upper and lower eyelids showed severe swelling with erythema and there was severe chemosis of the left conjunctiva (Fig. 1A). Duction and version of his left eye was limited at all gaze positions. A relative afferent pupillary defect was noted in the left eye, and the left eye also had exophthalmos of 8 mm. Fluorescein angiography did not exhibit any sign of retinal perfusion abnormalities or vasculitis (Fig. 1B). Orbit magnetic resonance imaging demonstrated abnormal streaky enhancement in the left preseptal and retrobulbar space and enlargement of the extraocular muscles. An abnormal diffusion signal from the left optic nerve was observed, which was compatible with acute ischemia (Fig. 1C, 1D). There was no evidence of neurological abnormalities or altered mentality, which could cause visual impairment.
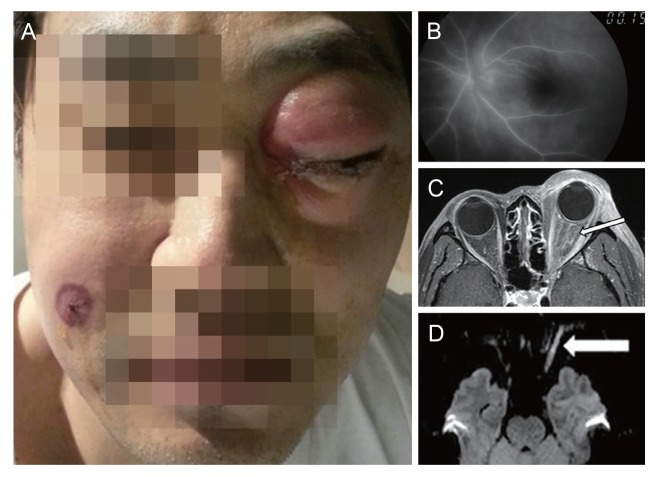
(A) A 40-year-old patient with periocular swelling and severe conjunctival chemosis of the left eye. An erythematous plaque developed on his right cheek. (B) Fluorescein angiography revealed normal vascular perfusion. (C) Orbit magnetic resonance imaging demonstrated an abnormal diffusion signal in the left optic nerve, suggesting acute ischemia (arrow). (D) Abnormal streaky enhancement in the left orbital preseptal area and retrobulbar space (arrow). Informed consent was received from the patient.
Orbital cellulitis, idiopathic orbital inflammation, and a hematologic malignancy-associated orbital lesion, such as high-grade lymphoma, were presumed. Thus, he was admitted to the internal medicine department and intravenous antibiotics (ceftriaxone and vancomycin) and steroid (dexamethasone) were started.
On day 2 of admission, a new erythematous plaque developed on his right cheek. Punch biopsy revealed lympho-neutrophilic infiltration of the entire dermis and epidermis with subepithelial separation. Bone marrow examination showed hypercellular marrow with dyserythropoiesis, dysmegakaryopoiesis, fibrosis, and increased blasts, suggestive of myelodysplastic syndrome or myeloproliferative neoplasm.
After 4 days, fever, eyelid swelling, and chemosis began to subside. Biopsies of the extraocular muscles and conjunctiva were performed and the pathological findings were identical to the previous skin punch biopsy results.
The clinical features of this case, including pyrexia, abrupt-onset erythematous plaques on the face involving the eye, and excellent response to systemic corticosteroid treatment, suggested a diagnosis of Sweet's syndrome. Histopathologic evidence of dense neutrophilic infiltration, abnormally increased laboratory values (e.g., erythropoietin sedimentary rate and C-reactive protein), and association with an underlying hematologic malignancy also supported a diagnosis of Sweet's syndrome.
Two weeks after starting steroid treatment, swelling of the left eyelid and conjunctival chemosis were almost completely resolved, but visual acuity in the left eye remained no light perception.
To the best of our knowledge, this is the first case of total blindness due to orbital involvement of Sweet's syndrome. Based on the magnetic resonance imaging findings of this case, optic nerve ischemia secondary to orbital compression caused permanent vision loss, and the inflammation associated with Sweet's syndrome can thus be severe enough to cause compressive optic neuropathy. In cases of orbital inflammation in patients with an underlying hematologic disorder, Sweet's syndrome must be included in differential diagnosis. Furthermore, it is crucial to consider early interventions such as surgical decompression to improve visual prognosis, especially in rapidly deteriorating cases.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.