Dear Editor,
Idiopathic orbital inflammation (IOI) is a diagnosis of exclusion and accounts for 4.7% to 6.3% of all orbital disease cases. Orbital myositis is included in IOI and shows inflammatory changes in the extraocular muscles (EOMs) [1,2]. Typically, orbital myositis has an acute clinical course in one eye and relapse is common [3]. There have been a few reports of relapse featuring alternating laterality [4]. We describe a patient with relapsing migratory myositis showing alternating laterality after a long period of quiescence.
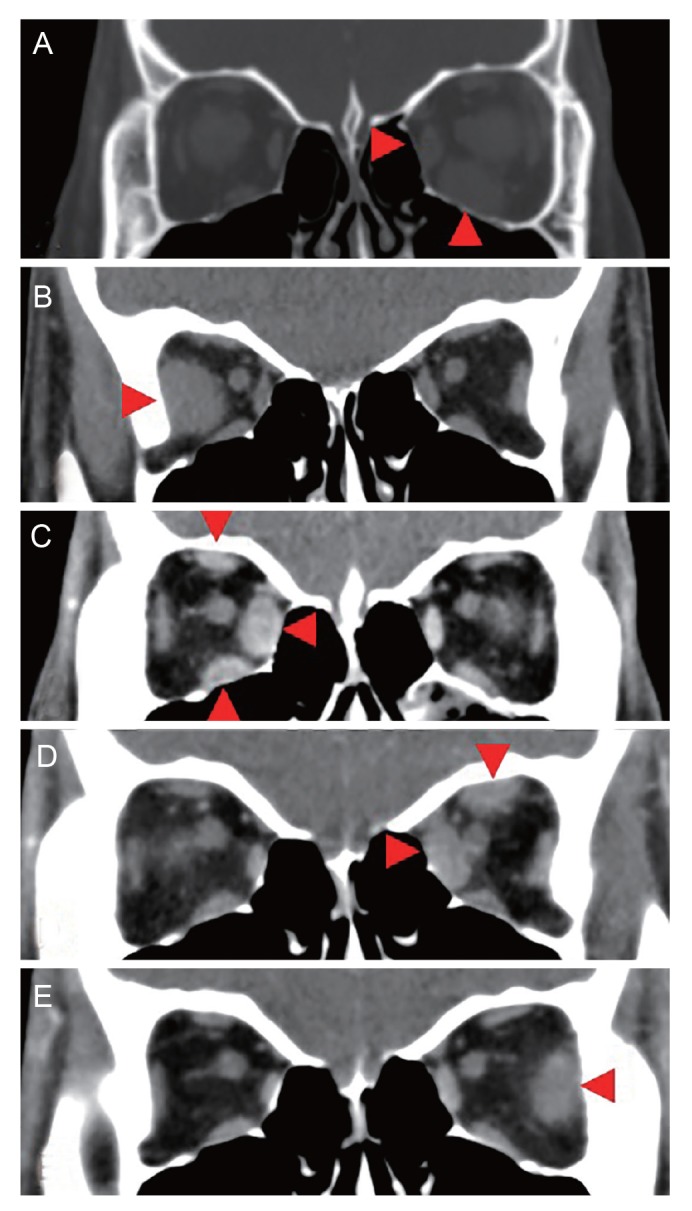
A 21-year-old woman presented with diplopia, periocular pain, proptosis, and restricted vertical gaze in the left eye. Radiographic images showed enlargement of the left medial and inferior rectus muscles involving the tendinous insertions (Fig. 1A). At initial evaluation, her best-corrected visual acuity was 20 / 20 in both eyes. Proptosis measured using a Hertel exophthalmometer was 13 mm in the right eye and 15.5 mm in the left. There were no abnormalities on systemic evaluation, including complete blood count, blood chemistry, thyroid function and thyroid auto-antibody analysis. She was diagnosed with IOI and treated with intravenous (IV) glucocorticoid pulse therapy. A daily dose of 1 g methylprednisolone was administered for 3 days, followed by an oral glucocorticoid. She had a favorable response and the oral glucocorticoid was tapered gradually over a period of several months (30 mg for 14 days, 15 mg for 14 days, 10 mg for 14 days, 5 mg for 14 days, 2.5 mg for 14 days, and was then discontinued). Seven years later, she returned with periocular pain and diplopia in the contralateral eye and orbit computed tomography (CT) showed a markedly swollen right lateral rectus muscle (Fig. 1B). She had radiotherapy in both eyes (total dose of 20 Gy in 10 fractions) after administering an IV glucocorticoid. Her symptoms and signs gradually resolved. Six months after the radiation therapy, conjunctival injection, restricted eye movement, and ocular pain recurred in the right eye; orbit CT showed enlargement of the superior, inferior, and medial rectus muscles in the right eye (Fig. 1C). She was started on oral prednisone immediately and this was then gradually tapered. Swelling and ptosis occurred in the right upper lid while tapering the steroid. The marginal reflex distance 1 was 0 mm in the right eye and 4 mm in the left. After observation for 1 year, she underwent levator resection surgery for the ptosis remaining in the right eye. She was observed without steroid treatment for 1 year after the surgery, but then returned with pain and limited adduction in the left eye. Orbit CT showed thickening of the superior and medial rectus muscles in the left orbit (Fig. 1D). Treatment with an IV glucocorticoid was started and the symptoms improved dramatically. One year later, she presented with left orbital pain and limited abduction in the left eye. Orbit CT showed thickening of the left lateral rectus muscle (Fig. 1E). She was admitted and started on an IV glucocorticoid. She was discharged on oral prednisone and the dose was tapered off.
Over 11 years, she had five episodes of relapsing-remitting myositis, which affected various EOMs with alternating laterality. All of the rectus muscles in both eyes were involved at different times. The time to recurrence ranged from 6 to 84 months, including the 7-year quiescent period until the first recurrence. After the first recurrence, she experienced painful myositis once a year and the pain-free period averaged 10 months. We recommended a biopsy of the EOM to confirm the diagnosis, but the patient refused. Currently, she maintains stable ocular symptoms by using oral steroids intermittently.
Recurrences are common in the same eye during the course of the disease, but are rare in the opposite eye [4]. Our patient had migratory myositis that occurred in different muscles in both eyes alternately (five recurrences). The reported time to first recurrence is 3 to 8 months [3]. There has been no report on alternating migratory orbital myositis with a long quiescent period until the first recurrence, such as in our patient. Our case emphasizes that complete resolution is not absolute, even in orbital myositis with a long symptom-free period. In conclusion, clinicians should be aware that orbital myositis can occur in a different location with alternating laterality and can recur at any time after the first attack.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






