 |
 |
| Korean J Ophthalmol > Volume 31(1); 2017 > Article |
Abstract
Purpose
To determine the accuracy of visual estimation of immediate postoperative intraocular pressure (IOP) following microincision cataract surgery (MICS) and the effect of immediate postoperative IOP adjustment on prevention of cystoid macular edema (CME).
Methods
Prospective, randomized analysis of 170 eyes in 135 patients with MICS, performed in a Medicare approved outpatient ambulatory surgery center. Surgical parameters included a keratome incision of 1.5 mm to 2.8 mm, topical anesthetic, case completion IOP estimation by palpation and patient visualization of light, and IOP adjustment before exiting the operating theater. IOPs were classified into three groups: low (<16 mmHg), normal (16 to 21 mmHg), and elevated (>21 to 30 mmHg). IOP measurements were repeated 1 day after surgery. Optical coherence tomography (Stratus OCT, Zeiss) was measured at 2 weeks. An increase in foveal thickness greater than 15 ┬Ąm was used to indicate CME. Statistical analysis was performed using one- and two-tailed Student's t-tests.
Results
Mean minimal foveal thickness averaged 207.15 ┬Ąm in the low pressure group, 205.14 ┬Ąm in the normal IOP group, and 210.48 ┬Ąm in the elevated IOP group 2 weeks following surgery. CME occurred in 14 of 170 eyes (8.2%) at 2 weeks (low IOP, 35.7%; normal IOP, 14.2%; elevated IOP, 50.0%). Change in IOP from the operating theater to 1 day after surgery was within +/ŌłÆ5 mmHg in 54 eyes (31.7%), elevated by 6 to 15 mmHg in 22 eyes (12.9%), and elevated more than 15 mmHg in four eyes (2.3%). IOP was reduced by 6 mmHg to 15 mmHg in 39 eyes (22.9%) and reduced by more than 15 mmHg in nine eyes (5.3%).
Conclusions
Immediate postoperative adjustment of IOP may prevent CME in MICS. Physicians can improve their ability to estimate postoperative IOP with experience in tonometry to verify immediate postoperative IOP. There are patient safety and economic benefits to immediate IOP adjustment in the operating theater.
Cystoid macular edema (CME) is the most common cause of reduced vision and poor visual outcomes following uncomplicated cataract surgery [1,2,3,4]. While previous reports have shown several identifiable causes [5,6,7,8,9,10,11,12,13], there has been no consensus on the exact etiology of CME in the vast majority of cases [6,14]. We propose that abnormal immediate postoperative intraocular pressure (IOP), an easily preventable etiology not commonly considered, may be a major cause of CME in routine cataract surgery cases.
A random block of patients undergoing routine microincision cataract surgery (MICS) by a single surgeon (JJ, Evergreen Eye Center) during a 3-month period from July to September 2008. Three other surgeons participated in IOP testing, but their patients were not examined with ocular coherence tomography (OCT) and thus served as a control group. Verbal informed consent was obtained, and patients chose to have their IOP tested and adjusted in the operating theater. If CME was noted, OCT (Stratus OCT; Zeiss, Dublin, CA, USA) of the macula was tested at 2 weeks and at 6 weeks following the cataract procedure, at no charge to the patient. Institutional review board approval was obtained through the clinical committee at Evergreen Eye Surgery Center, Federal Way, WA. Adjustment of IOP by sterile technique was performed at the conclusion of the MICS cataract procedure using a sterile tip TonoPen (AO Reichert, Buffalo, NY, USA), with a new sterile sleeve used for each patient. If the IOP was considered to be too high (>30 mmHg) or too low (<9 mmHg) or if any wound leaks were present, the IOP was adjusted using a sterile irrigating cannula with balanced salt solution (Allergan, Irvine, CA, USA). If the IOP was between 9 mmHg and 30 mmHg, the pressure was not adjusted but was measured again the following day. Routine preoperative eye drops consisting of cyclopentolate 1% (Cyclogyl; Alcon Laboratories, Fort Worth, TX, USA), ketorolac tromethamine 0.5% (Acular, Allergan), gatifloxicin 1% (Zymar, Allergan), and Neosynephrine 0.5% were instilled per usual preoperative protocol. Postoperative drops including gatifloxicin 1% (Zymar, Allergan), brimonidine 0.1% (Alphagan P, Allergan), and neomycin/polymyxin/dexamethaaone (Maxitrol, Alcon) ointment were instilled so long as no patient allergies were reported. Gentamycin sulfate 20 mg (Henry Schein, Chicago, IL, USA) and methylprednisolone 20 mg (Depo-Medrol, Henry Schein) in 0.5 cc solution was injected in the inferior subconjunctival fornix prior to pressure patching the eye overnight (in over 20,000 cases since this routine was first implemented, the authors observed no cases of endophthalmitisŌĆöhowever we have all now changed to intracameral moxifloxicin [Vigamox, Alcon] antibiotics and no longer give injectibles). The following day, vision testing including a Snellen chart, IOP testing with a TonoPen (AO Reichert, Depew, NY, USA), and slit lamp biomicroscopy was performed in the clinic following removal of the eye patch. An additional 2-week exam was performed on every patient who agreed to participate in the study, including a manifest refraction and Stratus OCT (Zeiss) of the macula in each eye [11,12]. Any patients noted to have reduced vision with macular thickening were placed on a prolonged course of prednisolone acetate 1% (Pred Forte, Allergan) ketorolac 0.5% (Acular, Allergan), four times daily or bromfenac sodium 0.09% (Xibrom; Ista Pharmaceuticals, Irvine, CA, USA) twice daily for 1 additional month, and macular OCT was repeated monthly until resolution of CME or a decrease in macular thickness to normal was noted.
One hundred thirty-five patients agreed to participate in the study and completed all follow-up visits. In total, 170 eyes (64 male and 106 female) qualified for the study. The average age was 70 years, with a range from 42 to 92 years. Eyes were excluded if they experienced iris trauma during the procedure or if they had any known disease other than cataract. The preoperative mean minimal foveal thickness was 185 ┬Ąm with a standard deviation of +/ŌłÆ15 ┬Ąm. Intraocular lenses included Crystalens 5.0, Crystalens HD, Rezoom, Restore, and aspheric acrylic new technology intraocular lenses. The average follow-up was 12 months with a range from 9 to 16 months.
Immediate unadjusted postoperative IOP ranged from 9 mmHg to 87 mmHg as measured following what was deemed by the operating surgeon to be a ŌĆ£safeŌĆØ adjusted IOP on the operating table after the ophthalmic viscoelastic device material was removed mechanically with the irrigation/aspiration tip and the eye was refilled with balanced salt solution. A Weck spear was used to press on the eye to determine the appearance of an indent-able ŌĆ£safeŌĆØ pressure, and the watertightness of the MICS phaco wound was verified. The patient confirmed the ability to visualize the operating microscope light filament, and the IOP was tested with a TonoPen (AO Reichert) using a sterile cover.
Prediction of immediate postoperative IOP varies greatly based on the surgeon and, in the present study, was initially not accurate (Fig. 1). We believe that scleral rigidity, increased elasticity in highly myopic patients, and decreased elasticity in hyperopic or older patients led to erroneously high or low estimates in the immediate postoperative IOP estimation [11]. Using the immediate feedback from the TonoPen measurements while the patient was still on the operating table, we were able to significantly improve predicted postoperative IOP with experience of two to three operating sessions (30 to 50 patients).
An additional finding was that the IOP varied only slightly from the final adjusted value on the operating table to that measured 24 hours later (Fig. 2). This seems to contradict other reported studies [15,16]. RF Brubaker, MD, at the Mayo Clinic (Rochester, MN) stated (September 1987) that the cause of a postoperatively elevated IOP ŌĆ£was unknown, since IOP was found to be elevated on postoperative examination the day following uncomplicated cataract surgery even before viscoelastics (ophthalmic viscoelastic device's) were introduced.ŌĆØ Our study, however, suggests that the IOP at the conclusion of the MICS cataract procedure is nearly the same as that measured at the day one postoperative exam.
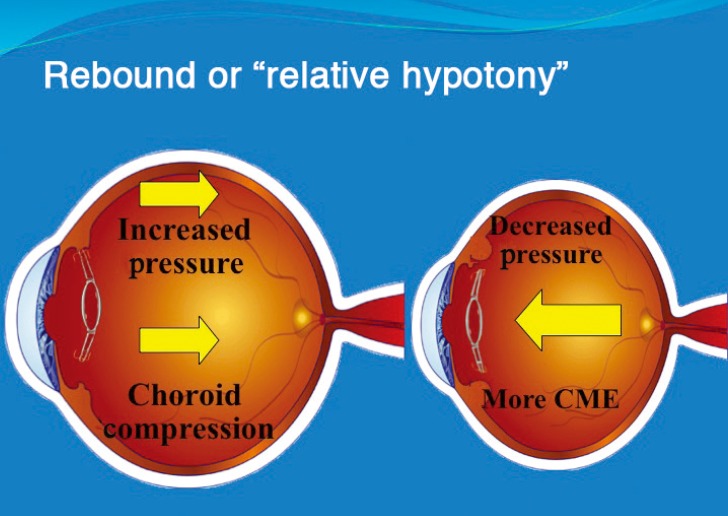
The macular OCT measurements conducted at 2 weeks are shown in Fig. 3. We found that patients with an IOP less than 16 mmHg had a four times greater incidence of CME compared to the control group with 16 mmHg to 21 mmHg (p = 0.012). Patients who had an initial postoperative pressure higher than 21 mmHg were noted to have a 2.5 times greater incidence of macular thickening (p = 0.029). We also confirmed that eyes with an extremely high initial IOP that was immediately adjusted to a safe range were more likely to develop macular thickening possibly due to ŌĆ£decompression retinopathyŌĆØ or ŌĆ£relative hypotony (Fig. 4),ŌĆØ as previously described by Bui et al. [17].
In conclusion, immediate adjustment of postoperative IOP on the operating table at the conclusion of cataract surgery may have a profound effect on preventing development of CME. Additionally, given very little change in IOP from the operating room table to the 1 day postoperative visit, we believe it is imperative to measure IOP immediately following completion of the cataract procedure in the operating theater or to become proficient with a tonometer in order to assure a safe pressure at the conclusion of surgery. The practice of immediate adjustment of postoperative IOP in the operating theater can provide an additional level of safety [18,19] to high-risk glaucoma patients undergoing cataract surgery [20] and to diabetic patients or those with compromised retinal vasculature, who are at higher risk for postoperative pressure spikes after anterior segment surgery [17,19,20,21,22].
Cost savings will result from fewer adjustments of IOP in patients who show unacceptable IOP spikes the day after surgery, who will no longer need tapping of the incision to a lower IOP, pressure-lowering medications, or additional eye drops. In our study, the additional time and expense of placing a lid speculum, tapping the incision with a sterile cannula, and repeat IOP testing if extrapolated over 1 year would cost approximately 44,000 dollars in lost physician and staff time and supplies necessary to adjust elevated postoperative IOP outside of the operating theater in a typical number of cataract patients according to the industrial engineer (KA Boudreau, MS, personal communication, January 2010).
Further studies are recommended to determine whether patient-specific matching of preoperative and postoperative IOP to individual eyes or evaluating whether high pressure phaco systems or excessive irrigating bottle height and relative decompression affect the blood retina barrier and lead to greater occurrence of CME. Micro incision cataract surgery in the future may include continuous control IOP monitoring and adjustment by biosensor feedback or implantable IOP-regulating transducers incorporated into the next-generation phaco systems to reduce the incidence of decompression retinopathy and associated CME.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Jurecka T, Batkova Z, Ventruba J. Macular edema after an uncomplicated cataract surgery. Cesk Slov Oftalmol 2007;63:262-273.

2. El-Ashry M, Hegde V, James P, Pagliarini S. Analysis of macular thickness in British population using optical coherence tomography (OCT): an emphasis on interocular symmetry. Curr Eye Res 2008;33:693-699.


3. Kecik D, Makowiec-Tabernacka M, Golebiewska J, et al. Macular thickness and volume after uncomplicated phacoemulsification surgery evaluated by optical coherence tomography: a one-year follow-up. Neuro Endocrinol Lett 2009;30:610-614.

4. Burling-Phillips L. After cataract surgery: watching for cystoid macular edema [Internet]. San Francisco, CA: EyeNet; 2007. cited 2017 Jan 13. Available from: http://www.aao.org/publications/eyenet/200701/retina.cfm.
5. Yuksel N, Dogu B, Karabas VL, Caglar Y. Foveal thickness after phacoemulsification in patients with pseudoexfoliation syndrome, pseudoexfoliation glaucoma, or primary open-angle glaucoma. J Cataract Refract Surg 2008;34:1953-1957.


6. Chao WJ, Liu SB, Dai RP, et al. Clinical analysis of intraocular pressure elevation following vitreoretinal surgery. Zhonghua Yi Xue Za Zhi 2009;89:318-320.

7. Degenring RF, Vey S, Kamppeter B, et al. Effect of uncomplicated phacoemulsification on the central retina in diabetic and non-diabetic subjects. Graefes Arch Clin Exp Ophthalmol 2007;245:18-23.


8. Biro Z, Balla Z, Kovacs B. Change of foveal and perifoveal thickness measured by OCT after phacoemulsification and IOL implantation. Eye (Lond) 2008;22:8-12.


9. Catier A, Tadayoni R, Paques M, et al. Characterization of macular edema from various etiologies by optical coherence tomography. Am J Ophthalmol 2005;140:200-206.


10. Lobo CL, Faria PM, Soares MA, et al. Macular alterations after small-incision cataract surgery. J Cataract Refract Surg 2004;30:752-760.


11. Cagini C, Fiore T, Iaccheri B, et al. Macular thickness measured by optical coherence tomography in a healthy population before and after uncomplicated cataract phacoemulsification surgery. Curr Eye Res 2009;34:1036-1041.


12. Ching HY, Wong AC, Wong CC, et al. Cystoid macular oedema and changes in retinal thickness after phacoemulsification with optical coherence tomography. Eye (Lond) 2006;20:297-303.


13. Pareja-Esteban J, Moreno-Arrones JP, Drake-Rodriguez-Casanova P, et al. Morphological macular changes after cataract surgery: risk factors. Arch Soc Esp Oftalmol 2009;84:605-610.

14. Belair ML, Kim SJ, Thorne JE, et al. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol 2009;148:128-135.e2.



15. Rhee DJ, Deramo VA, Connolly BP, Blecher MH. Intraocular pressure trends after supranormal pressurization to aid closure of sutureless cataract wounds. J Cataract Refract Surg 1999;25:546-549.


16. Levkovitch-Verbin H, Habot-Wilner Z, Burla N, et al. Intraocular pressure elevation within the first 24 hours after cataract surgery in patients with glaucoma or exfoliation syndrome. Ophthalmology 2008;115:104-108.


17. Bui CM, Recchia FM, Recchia CC, Kammer JA. Optical coherence tomography findings in ocular decompression retinopathy. Ophthalmic Surg Lasers Imaging 2006;37:333-335.


18. Vu MT, Shields MB. The early postoperative pressure course in glaucoma patients following cataract surgery. Ophthalmic Surg 1988;19:467-470.


19. Hayreh SS. Anterior ischemic optic neuropathy. IV: occurrence after cataract extraction. Arch Ophthalmol 1980;98:1410-1416.


20. Shingleton BJ, Rosenberg RB, Teixeira R, O'Donoghue MW. Evaluation of intraocular pressure in the immediate postoperative period after phacoemulsification. J Cataract Refract Surg 2007;33:1953-1957.


Fig.┬Ā1
Case completion estimated intraocular pressure by surgeon. Immediate unadjusted postoperative intraocular pressure estimates varied by surgeon and were initially inconsistent. These estimates improved with surgeon experience over the course of the study.
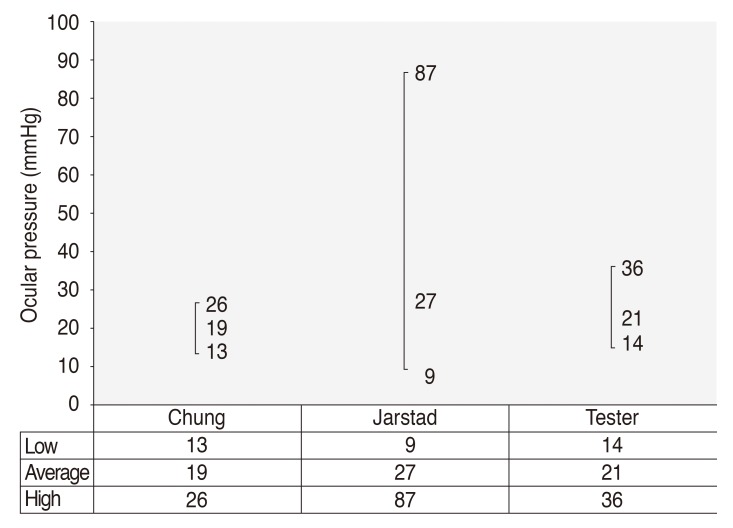
Fig.┬Ā2
Change in intraocular pressure (IOP) from case completion to 1-day postop. Change in adjusted IOP from the operating theater to 1-day postop. Note the distribution showing little change in IOP in the majority of cases from the IOP adjusted on the operating room table to the next day postop. postop = postoperative.
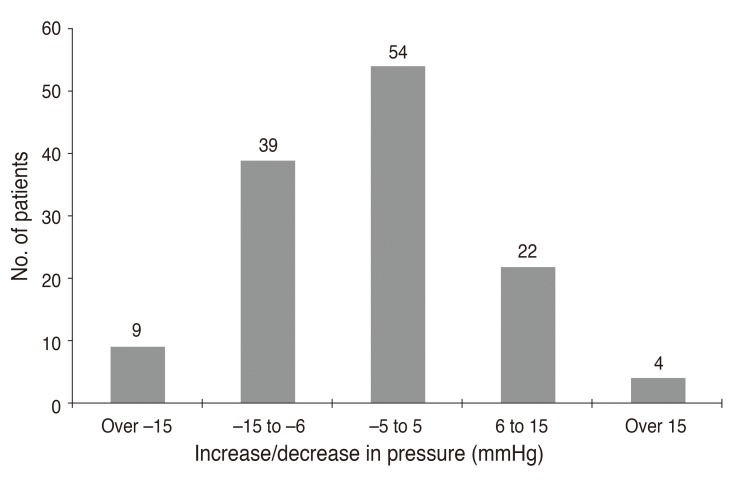
Fig.┬Ā3
Cystoid macular edema (CME) by intraocular pressure (IOP) group. Two week macular thickness in the adjusted IOP group. CME grouped by adjusted postoperative IOP. Note that IOP values greater than 22 mmHg were responsible for 50% of the cases of CME, while normally adjusted IOP had the lowest incidence. *Patients considered to have macular edema if surgical eye is 15 or more microns thicker than non-surgical eye.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




