Effectiveness of Toric Orthokeratology in the Treatment of Patients with Combined Myopia and Astigmatism
Article information
Abstract
Purpose
The purpose of this multi-institute, single-group clinical trial was to evaluate the effectiveness and safety of toric orthokeratology lenses for the treatment of patients with combined myopia and astigmatism.
Methods
A total of 44 patients were included in this clinical trial. The patients ranged in age from 7 to 49 years, with myopia of -0.75 to -6.0 diopters (D) and astigmatism of 1.25 to 4.0 D. After excluding 21 subjects, 23 subjects (39 eyes) were analyzed after toric orthokeratology lens use. The subjects underwent ophthalmologic examination after 1 day and 1, 2, 3, and 4 weeks of wearing overnight toric orthokeratology lenses.
Results
A total of 19 subjects (31 eyes) completed the trial after five subjects (eight eyes) dropped out. In the patients who completed the study by wearing lenses for 4 weeks, the myopic refractive error decreased significantly by 2.60 ± 2.21 D (p < 0.001), from -3.65 ± 1.62 to -1.05 ± 1.64 D. The astigmatic refractive error were also significantly decreased by 0.63 ± 0.98 D (p = 0.001), from 2.07 ± 0.83 to 1.44 ± 0.99 D. The mean uncorrected and corrected visual acuities before wearing the lenses were 2.14 ± 0.80 logarithm of the logMAR (logMAR) and 0.05 ± 0.13 logMAR, respectively, which changed to 0.12 ± 0.30 logarithm of the logMAR (p < 0.001) and 0.01 ± 0.04 logMAR (p = 0.156) after 4 weeks. No serious adverse reactions were reported during the clinical trial.
Conclusions
Our results suggest that toric orthokeratology is an effective and safe treatment for correcting visual acuity in patients with combined myopia and astigmatism.
Although corneal cutting procedures such as laser-assisted in situ keratomileusis and laser-assisted subepithelial keratectomy are commonly used to adjust corneal thickness and in order to restore or improve deteriorated vision, several side effects of these procedures have been reported. Specifically, laser-assisted in situ keratomileusis and laser-assisted subepithelial keratectomy are associated with lack of visual acuity correction, development of astigmatism, and various corneal diseases [12]. As an alternative, investigators and clinicians have begun to focus on the use of orthokeratology lenses to prevent the progression of myopia. Importantly, orthokeratology can be used in patients for whom surgery is not financially viable or who do not want to undergo laser treatment [34].
Orthokeratology is a reversible method used to correct vision, and a number of reports have been published since Jessen first attempted in 1962 to change the corneal curvature using a polymethyl methacrylate contact lens, which at the time was referred to as orthofocus [5]. With the recent development of rigid gas-permeable (RGP) contact lenses, which have high oxygen permeability, there has been increased interest in orthokeratology due to the decreased potential for side effects of wearing lenses during sleep [67].
Unlike common contact lenses, the lenses used in orthokeratology are designed with a ‘reverse geometry’ in which the curvature in the center is flatter than that at the periphery [7]. Importantly, the inner surface of the lens presses down on the elevated corneal center to reshape the cornea [5]. This reshaping acts to correct myopia by maintaining the cornea in a depressed state for a certain period. In this way, vision can be improved with minimal corneal damage.
However, in order to correct myopia, orthokeratology lenses must be precisely placed at the corneal center, which is difficult in patients with astigmatism resulting from a difference in corneal curvature between the long and short axes [34]. Consequently, the vision-correction success rate of patients with both myopia and astigmatism is markedly decreased compared to that of patients without astigmatism. In addition, the prevalence of astigmatism is as high as that of myopia in Korea and East Asia, almost 60%, and this value significantly increases with age [8].
In order to correct astigmatism caused by corneal curvature defects, orthokeratology lenses must have more than two aspherical curvatures that match the shape of the corneal surface, which allows the lens to be placed precisely at the center of the cornea [910]. Thus, toric orthokeratology lenses with more than two curvatures are expected to be useful in correcting the vision of patients with both myopia and astigmatism. On this basis, we investigated the effectiveness and safety of toric orthokeratology lenses for the correction of myopia combined with astigmatism.
Materials and Methods
This was a multi-institute, single-group clinical trial conducted at Seoul St. Mary's Hospital and Uijeongbu St. Mary's Hospital from February 6, 2014 to June 20, 2014. Approval was granted by the respective institutional review boards of each institute, and a clinical trial permit was obtained from the Ministry of Food and Drug Safety. This study was carried out in accordance with the tenets of the Declaration of Helsinki.
Subjects
At the screening visits, the investigators informed the subjects of the complete details of the clinical trial, after which the subjects signed a written consent form. We then obtained demographic information, history of ocular diseases, and current disease information from each subject and determined visual acuity, refractive error, corneal topography, slit-lamp microscopy, corneal endothelial cell count, central corneal thickness (CCT), intraocular pressure, Schirmer's test result, and tear break-up time.
The inclusion criteria for subjects were as follows: (1) age between 7 and 49 years, (2) myopic refractive error of -0.75 to -6.0 diopters (D) and astigmatic refractive error of 1.25 to 4.0 D, (3) radius of corneal curvature within the range of 46.00 to 39.75 D (7.34 to 8.5 mm), (4) horizontal corneal diameter larger than 11.0 mm, (5) occupation and environment allowing wear of lenses for more than 7 hours during sleep, (6) ability to follow instructions during the clinical trial, and (7) willingness to participate in the clinical trial and provide signed written consent.
The exclusion criteria were: (1) Schirmer test result less than 10 mm or tear break-up time shorter than 10 seconds, (2) abnormal findings during slit-lamp microscopy; inflammation, erosions, ulcers, or angiogenesis in the cornea after wearing the lens for a 30-minute trial period, (3) allergies, (4) eye diseases that would have made participation in the trial difficult as judged by the investigator, (5) contraindication for wearing contact lenses, (6) wearing of RGP lenses within the 2 weeks prior to the screening visit, (7) diagnosed strabismus, (8) past corneal refractive surgery, (9) pregnancy, nursing, or planning to become pregnant, and (10) significant disease that would have made participation in the clinical trial difficult as judged by the investigator. Candidates who met any one of the above criteria were excluded from the trial.
Examinations
At the first visit (day 1), subjects tried the toric orthokeratology lenses prescribed at the screening visit and were informed of the precautions that must be taken when wearing the lenses, as well as the potential adverse reactions. Slit-lamp microscopy was performed, the refractive error was measured, and any adverse reactions to wearing the lenses were assessed. Fit was confirmed during slit-lamp microscopy, along with determination of abnormal corneal findings. To confirm fit, we verified that there was pressure on the cornea, and that a space was maintained between the back of the toric orthokeratology lens and the cornea. While monitoring the changes in the kerato-conjunctiva, the ocular status in each subject's anterior segment was scored from 0 to 4 points using the Efron grading scale [11]. Moderate to severe scores in this test were considered as indicators of an adverse reaction. Any other clinically significant findings in the kerato-conjunctiva were also recorded as adverse reactions.
In cases of poor lens fit, subjects were able to request up to three new prescriptions. All subjects were instructed to wear the lenses for an average of 7 hours during sleep and to not wear the lenses during the day.
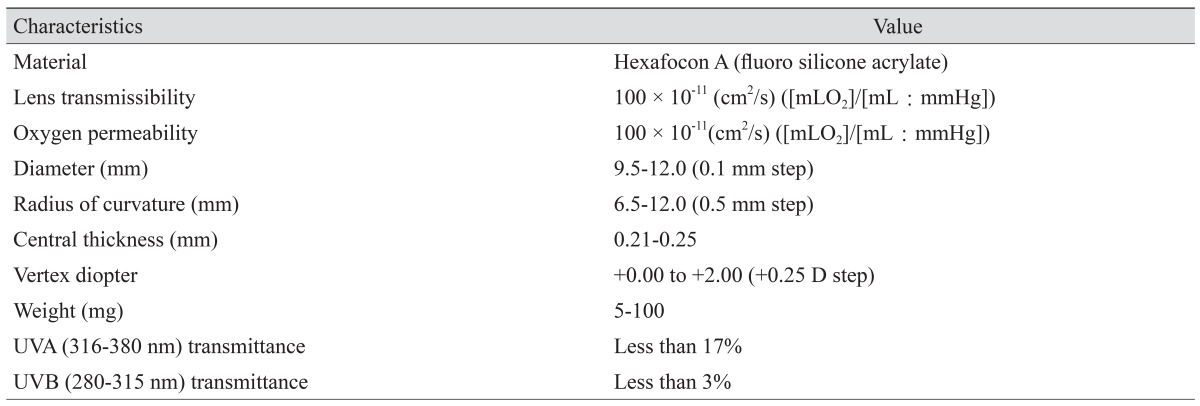
The second visit (day 2) took place 1 day after wearing the toric orthokeratology lenses overnight. Both uncorrected visual acuity and refractive error were measured, and slit-lamp microscopy was performed. Compliance and adverse reactions were assessed. The same tests were repeated after 1, 2, and 3 weeks of lens wear. On the last visit (week 4), in addition to performing the tests described above, corneal endothelial cell count and CCT were measured. The toric orthokeratology lenses used in the trial were Toric LK Lens (Lucid Korea, Bonghwa, Korea). The characteristics of the lens are described in Table 1.
Statistical analysis
The primary outcome measures in this study were myopic and astigmatic refractive errors after toric orthokeratology lens use. For convenience of analysis, the astigmatic refractive error represented only corneal astigmatism not lenticular astigmatism. Limbus-to-limbus astigmatism was not included in this study. Secondary study outcomes included visual acuity, corneal curvature, time to reach the target uncorrected vision of 16 / 20 after wearing the lenses. To assess safety, slit-lamp microscopy was performed, and the ocular status score in the anterior segment was recorded. Corneal endothelial cell count and CCT were also measured, and the total incidence of adverse reactions was evaluated. Statistical analyses of myopic and astigmatic refractive errors were performed using a two-tailed, paired t-test. For all other outcomes we used a two-tailed, paired t-test or Wilcoxon's signed-rank test as appropriate. The change in ocular status score in the anterior segment, as determined using slit-lamp microscopy, was input into a split table (frequency, ratio) and analyzed using Bowker's test. For all statistics, a p-value <0.05 was considered significant. For missing values and when subjects dropped out before the trial was completed, the data from the subject was not included in our analysis.
Results
In this clinical trial, a total of 79 eyes (44 subjects) were screened at one of two trial-conducting institutes; 40 eyes (21 subjects, 50.63%) were excluded after screening, leaving a total of 39 eyes (23 subjects, 49.37%) to be tested after lens use. Thirty-one eyes (19 subjects, 39.24%) completed the trial. Details of the subjects' eyes at registration are presented as a schematic diagram in Fig. 1. The participants comprised 21 women (77.78%) and six men (22.22%). The mean age was 21.81 ± 8.89 years, with a range of 7 to 39 years. There were no pregnancies among the 19 women of childbearing age that were included in the study.

Numbers of subjects recruited for the study and who dropped out. The reasons for exclusion and drop-out are described. TBUT = tear break-up time.
Myopic and astigmatic refractive error
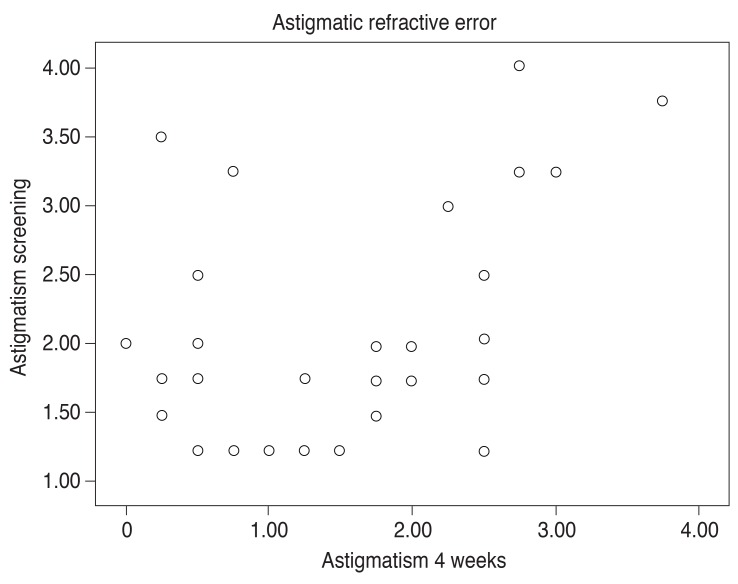
The mean myopic refractive error changed from -3.65 ± 1.62 to -1.05 ± 1.64 D after wearing the lenses for 4 weeks, which constituted a statistically significant decrease of 2.60 ± 2.21 D (p < 0.001). The correction of myopia by toric or-thokeratology lenses resulted in a superior refractive state (Table 2 and Fig. 2). The mean astigmatic refractive error changed from 2.07 ± 0.83 to 1.44 ± 0.99 D after wearing the lenses for 4 weeks, which constituted a statistically significant decrease of 0.63 ± 0.98 D (p = 0.001). The correction of astigmatism by toric orthokeratology lenses resulted in a superior refractive state (Table 2 and Fig. 3).
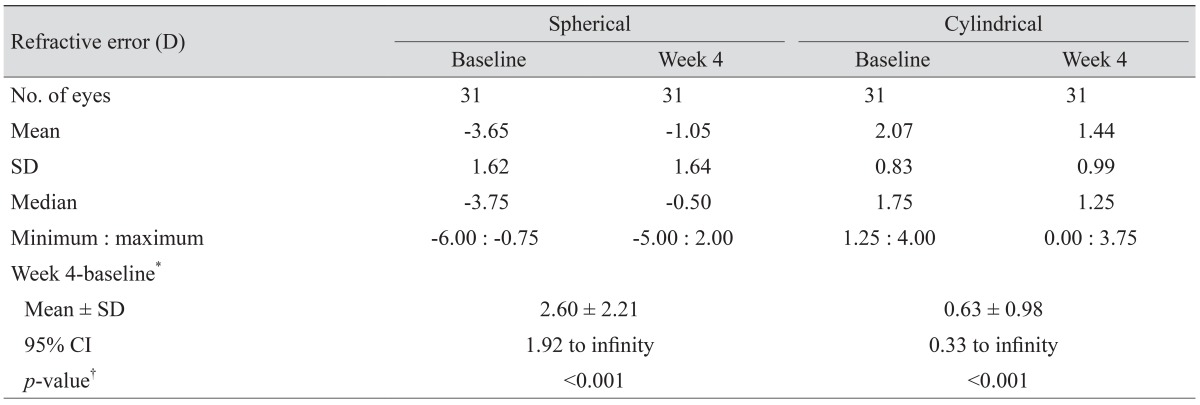
Spherical and cylindrical refractive errors measured at screening and after 4 weeks of toric orthokeratology lens use
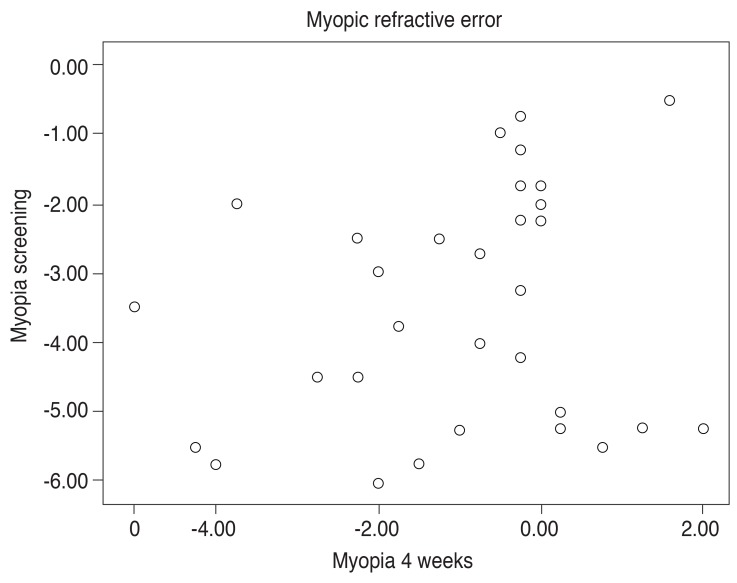
Scattergram showing subject distribution according to myopic refractive error at the time of screening and at the end of the study.
Uncorrected and corrected visual acuity
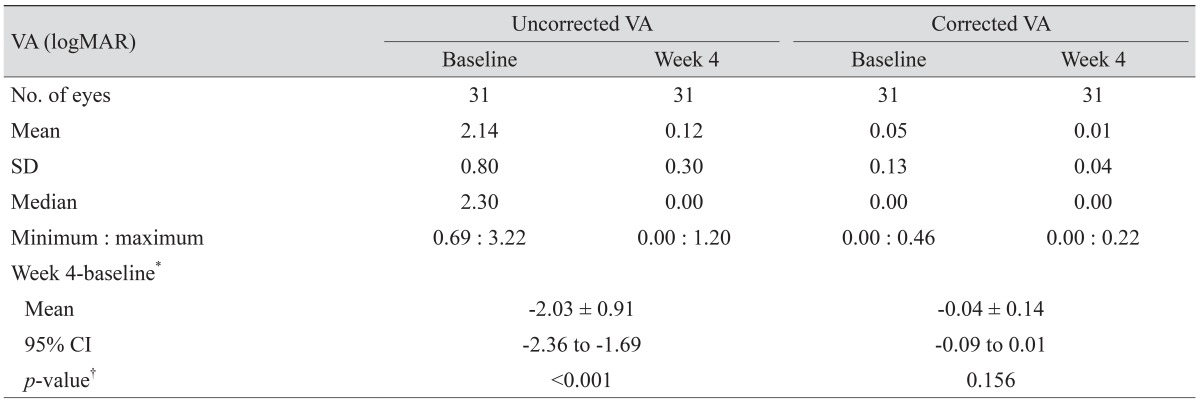
The mean uncorrected and corrected visual acuities at the screening visit were 2.14 ± 0.80 and 0.05 ± 0.13 logMAR, respectively. The equivalent values after wearing the toric orthokeratology lenses for 4 weeks were 0.12 ± 0.30 and 0.01 ± 0.04 logarithm of the minimal angle of resolution (logMAR), respectively. The difference in uncorrected visual acuity was -2.03 ± 0.91 logMAR, which was statistically significant (p < 0.001). The difference in corrected visual acuity was -0.04 ± 0.14 logMAR, which was not statistically significant (p = 0.156) (Table 3). After wearing the lenses for 1 week, corrected visual acuity was greater than 16 / 20 in 29 eyes (93.55%). All of the eyes achieved a corrected visual acuity greater than 16 / 20 after wearing the lenses for 2 weeks.
Corneal topography and thickness
At the screening visit, the mean corneal curvature was 42.54 ± 1.06 D, and the mean corneal diameter was 11.78 ± 0.28 mm. After wearing the toric orthokeratology lenses for 4 weeks, the mean corneal curvature was 40.92 ± 1.38 D and the mean corneal diameter was 11.76 ± 0.35 mm. A representative topographic pattern of corneal astigmatism is shown in Fig. 4A and 4B. After treatment, the difference in corneal curvature was -1.62 ± 0.96 D, which was statistically significant (p < 0.001). However, the difference in corneal diameter was -0.02 ± 0.35 mm, which was not statistically significant (p = 0.710). The mean CCT values before and after wearing the lenses were 560.21 ± 38.64 and 545.76 ± 61.37 µm, respectively. The mean difference was -14.45 ± 37.46 µm, which constituted a statistically significant decrease (p = 0.047) (Table 4).
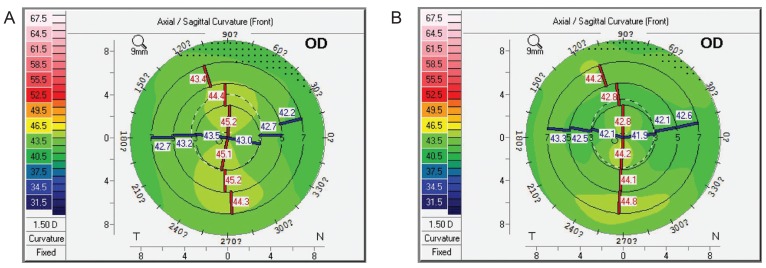
Typical topographic pattern of corneal astigmatism of subjects at screening (A) and at the end of the study (B). The average corneal astigmatism of subjects decreased from 1.9 to 1.6 diopters. OD = right eye.
Corneal endothelial cell counts
The mean corneal endothelial cell count at the screening visit was 3,196.55 ± 237.80 cells/mm2, which increased by 40.72 ± 207.67 cells/mm2 to 3,237.28 ± 277.25 cells/mm2 after 4 weeks of toric orthokeratology lens use. However, this difference was not statistically significant (p = 0.300). The difference in hexagonality was -0.07 ± 12.07, which was also not statistically significant (p = 0.976). The coefficient of variation before and after wearing the lenses was 0.31 ± 0.05 and 0.33 ± 0.07. The difference of 0.02 ± 0.06 was statistically significant (p = 0.027) (Table 4).
Slit-lamp microscopy
The Efron grading scale scores during the trial were normal for all eyes in all categories except for “corneal staining,” in which 38 eyes (97.44%) were normal, and one eye (2.56%) was graded as trace before wearing the lenses. After 4 weeks of lens use, 25 eyes (80.65%) were normal, four eyes (12.90%) were graded as trace, and two eyes (6.45%) were graded as mild. The difference in grading before and after lens use was not statistically significant (p = 0.815).
Adverse reactions
A total of five adverse reactions developed in five subjects, consisting of one case of ‘ocular pain’ (3.23%), one case of ‘conjunctival hyperemia’ (3.23%), one case of ‘foreign body sensation in the eyes’ (3.23%), and two cases of ‘common cold’ (6.45%). In all cases, the adverse reactions ceased after the patients were prescribed additional artificial tears and were provided additional education regarding the proper wear and removal of the lenses. None of the patients in this study dropped out due to an adverse reaction.
Discussion
With the introduction of orthokeratology by Wesley and Jessen in the early 1960s, many clinicians and researchers have attempted to correct myopia using rigid contact lenses; however, these attempts have been limited by patient discomfort and hypoxic corneal damage [5]. The development of RGP lens material combined with advancements in contact lens manufacturing technology has led to the development of overnight orthokeratology, which enables patients to wear myopia-correcting contact lenses during sleep. In overnight orthokeratology, the reverse-geometry lens is designed with both a flatter central curvature and steeper peripheral curvature such that a tear reservoir can be formed, and the lens is precisely placed in the corneal center.
In 2000, Nichols et al. [7] reported that overnight orthokeratology by the programmed application of RGP contact lenses with a reverse geometrical design is an effective means of temporarily reducing myopia. Furthermore, they suggested a possible mechanism of corneal remodeling through central corneal thinning.
A number of clinical trials to date have concluded that orthokeratology can effectively reduce moderate to high myopia, and control the progression of myopia [12131415161718]. In addition, several reports have addressed the correction of astigmatism using orthokeratology lenses, although these effects are typically insufficient due to lens decentration [341920].
To address the issue of decentration, Chen et al. [9] examined the efficacy of toric orthokeratology in correcting myopia combined with moderate to high astigmatism. In their study, subjects aged 6 to 12 years with myopia of 0.50 to 5.00 D and with with-the-rule astigmatism of 1.25 to 3.50 D were fitted with toric orthokeratology lenses. They reported that manifest myopia was significantly reduced from 2.53 ± 1.31 to 0.41 ± 0.43 D (p < 0.001), and that astigmatism was also decreased from 1.91 ± 0.64 to 0.40 ± 0.39 D (p < 0.001) after 1 month of lens wear. Similarly, in 2013, Chen et al. [10] conducted a non-randomized clinical study in which toric orthokeratology was found to effectively control myopia in children with accompanying moderate-to-high astigmatism.
To our knowledge, this is the first prospective, multi-center clinical trial to have investigated the effectiveness of toric orthokeratology in Korea. Specifically, we evaluated the effectiveness and safety of toric orthokeratology lenses in patients with both myopia and astigmatism. Patients wore the toric orthokeratology lenses during sleep for an average of 7 hours and for up to 4 weeks (28 days). The results showed than overnight toric orthokeratology reduced both myopia and astigmatism, although the degree of chance in astigmatism was relatively small. We attributed this small change to a weakened effect of the toric orthokeratology lenses to reshape the cornea during the night, as the subjects in this study visited our institute primarily in the afternoon. Thus, additional studies regarding the clinical effectiveness of toric orthokeratology in correcting astigmatism are needed. Unlike astigmatism, uncorrected visual acuity was significantly improved in our study, although there was no change in corrected visual acuity. Thus, our results suggest that toric orthokeratology lenses do not change the ocular features associated with corrected visual acuity, which reflects the safety of this approach.
A number of studies have suggested that various ocular parameters (corneal thickness in particular) are modifiable or predictive values for myopic reduction in orthokeratology [212223242526]. In 2000, Lui and Edwards [21] reported that CCT is the most predictive value of myopic reduction based on the results of a randomized controlled clinical trial involving 14 subjects who wore orthokeratology lenses during the daytime. Specifically, they suggested that a thicker initial central cornea is associated with a greater reduction in myopia. In addition, Li at el. [26] conducted a meta-analysis that included a total of 10 studies with 339 eyes from 239 patients in order to assess the change to CCT by orthokeratology lens use in myopic patients. They found that CCT was reduced significantly between 1 day and 1 week, and that the most significant reduction occurred between 1 day and 1 month. In our study, CCT was significantly decreased (p = 0.005) after 4 weeks of lens wear but remained within the normal range. This might have been due to the reverse-geometry lens pressing down on the corneal center, causing rearrangement of the epithelium [727].
Among the five adverse reactions noted in five subjects during our trial, reactions exclusively concerning the lenses comprised four cases (12.90%), all of which were mild in nature and recovered fully. According to silt-lamp microscopy and other examinations of ocular parameters, there were no significant changes except for the CCT and coefficient of variation, although CCT remained within the normal range after 4 weeks. On the other hand, the change in coefficient of variation was considered to be a common effect of all types of contact lenses on corneal polymegathism, and the extent of the increase was not large relative to that noted in other studies [28]. Together, these data indicate that use of toric orthokeratology lenses does not cause any significant changes in ocular conditions. On the basis of these findings, our results suggest that toric orthokeratology lenses do not have any serious harmful effects.
One limitation of this clinical trial was that the follow-up period was only 4 weeks. Based on our results, additional studies with a longer-term follow-up are indicated. The purpose of these studies should be to elucidate further aspects and complications of toric orthokeratology, such as maintenance of lens centration or changes in ocular features.
In conclusion, the effectiveness of toric orthokeratology lenses in correcting myopia combined with astigmatism was verified statistically. Orthokeratology lenses are currently limited to the correction of myopia; however, our results provide an experimental basis for broadening the scope of orthokeratology lenses to include the correction of astigmatism. Importantly, there were no notable adverse reactions or significant abnormal findings caused by use of toric orthokeratology lenses as determined by silt-lamp microscopy and other examinations. Therefore, toric orthokeratology can be considered an effective and safe treatment for correcting visual acuity in patients with combined myopia and astigmatism.
Acknowledgements
This study was funded by the Korea Health Industry Development Institute (HI13C0307). The funding organization had no role in the design or conduct of this research.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.