Traumatic Dislocation of Posterior Chamber Phakic Intraocular Lens into the Berger's Space
Article information
Dear Editor,
Berger's space is a potential compartment that can present behind the crystalline lens but is not open in normal situations. This space is formed by the posterior lens surface and anterior vitreous face and is circumscribed by Weiger's ligament [1]. Except for some congenital abnormalities, Berger's space is rarely involved in ocular disease because of vulnerability of structures surrounding this potential space. We report a case with dislocation of a posterior chamber phakic intraocular lens (IOL) into Berger's space after blunt trauma.
A 45-year-old male visited our clinic with decreased vision after blunt trauma to the right eye. He had undergone posterior chamber phakic IOL (Implantable Contact Lens; STAAR Surgical AG, Nidau, Switzerland) implantation surgery in both eyes 14 years earlier. Distance-corrected visual acuity was finger counting in the right and 20 / 20 in the left eye at the first visit. Intraocular pressure was 19 and 18 mmHg in the right and left eyes, respectively. On slit-lamp examination, dislocation of the phakic IOL into Berger's space was noted (Fig. 1A and 1B). No gross damage was found in other surrounding structures including the iris and crystalline lens. On fundus examination, mild inferior vitreous hemorrhage was found.
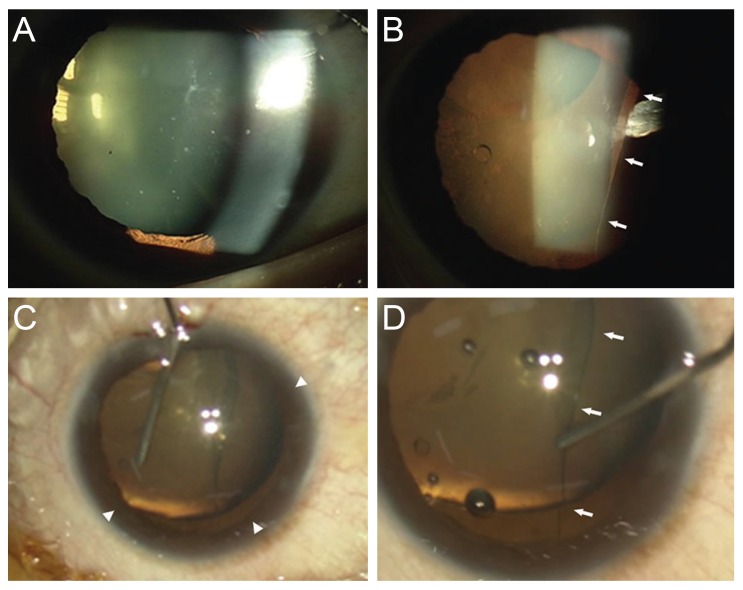
(A) Preoperative slit-lamp photograph of the right eye shows an otherwise normal anterior segment except for mild cataract, which is thought be related to phakic intraocular lens (IOL) implantation. (B) Retro-illumination shows a dislocated phakic IOL behind the crystalline lens. Note the margin of the phakic IOL (arrows). (C) After instillation of viscoelastic material into the anterior chamber through a 2.2-mm clear corneal incision during the operation, extensive zonular dialysis was confirmed (2 to 8 o'clock, arrowheads). (D) The phakic IOL was located between the crystalline lens and anterior hyaloid face (Berger's space). Note the margin of the phakic IOL (arrows).
After days of supportive care for other combined traumatic body injuries such as head trauma and multiple rib and leg fractures, surgical intervention for the dislocated IOL was performed under local anesthesia. After instillation of viscoelastic material into the anterior chamber through a 2.2-mm clear corneal incision, zonular dialysis that extended from 2 to 8 o'clock was confirmed (Fig. 1C). Vitreous prolapse was not found in the anterior chamber, indicating an intact anterior hyaloid face. The dislocated phakic IOL was located just behind the lens, with optic and plate haptics facing the posterior surface of the lens. The dislocated IOL in Berger's space was carefully relocated to the anterior chamber through the inferior zonular defect using a spatula. It was then removed through the main corneal incision using a forceps (Fig. 1D). Phacoemulsification of the crystalline lens was performed without disruption of the posterior lens capsule. However, considering the preoperative IOL power calculation result suggesting zero diopter postoperative emmetropia and an extensive zonular defect, removal of the remaining lens capsule and minimal anterior vitrectomy were performed, leaving the eye in an aphakic state.
Uncorrected distance visual acuity of the right eye improved to 20 / 30, and distance-corrected visual acuity was 20 / 20 1 day postoperatively. At the last follow-up visit at 6 months, no significant sequelae were found. Uncorrected distance visual acuity of the right eye was 20 / 30, and refractive error was -1.25 diopter in a spherical equivalent.
Posterior chamber phakic IOL dislocations to correct myopia are relatively rare compared to traumatic or spontaneous dislocations of IOL for senile cataract surgery. Spontaneous dislocation of a phakic refractive lens into the vitreous cavity 2 months postoperatively has been reported in a highly myopic patient [2]. That patient was treated with lensectomy, pars plana vitrectomy, and phakic refractive lens removal. Silicone phakic IOL dislocation into the vitreous cavity with [34] or without history of ocular trauma [5] have also been reported. To our knowledge, however, dislocation of a posterior chamber phakic IOL into Berger's space without disruption of its surrounding structures including the anterior vitreous face and crystalline lens has not been reported. Zonular weakness or defect caused by axial elongation and subsequent excessive stretching of the zonular fibers may have existed in the high myopic eye [2]. Axial compression and sudden elevation of intraocular pressure caused by blunt trauma of the eye might have produced extensive rupture of the vulnerable zonule, through which the phakic IOL was forced into Berger's space. Axial compression may have created this potential space and facilitated luxation of the phakic IOL. The phakic IOL was also soft enough to be rolled and moved into Berger's space instead of penetrating the anterior hyaloid face and being luxated into the vitreous cavity.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.