Dear Editor,
The causes of epiphora can be separated into two categories: (1) reflex epiphora, which is caused by surface damage to the eye or infectious ocular disease, and (2) lacrimal pumping failure, which is caused by anatomical and functional failure in the outflow tract due to abnormal position of the lacrimal puncta or closure of the nasolacrimal duct [1,2]. The abnormal position of the lacrimal punctum in this case was caused by atypical protrusion of the punctum. This case is significant as it presents a rare condition and highlights the importance of punctum location for adequate tear flow in addition to maintaining contact with the tear meniscus. Furthermore, a novel surgical technique of punctal fixation is described that was used to successfully treat the patient.
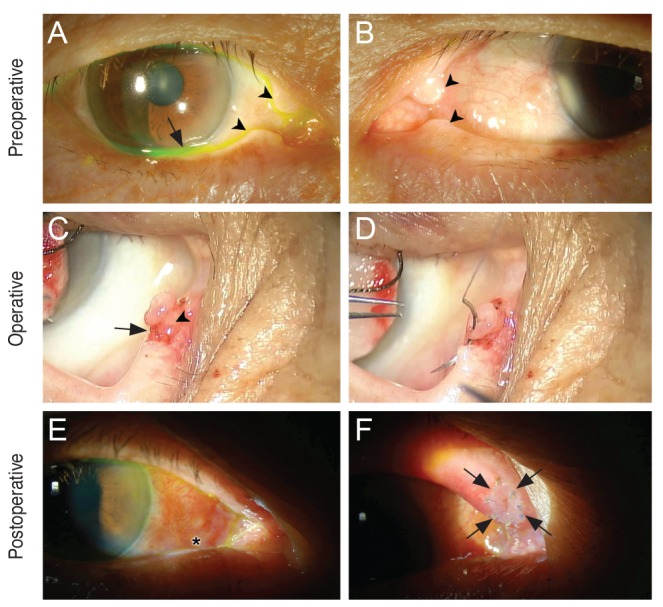
A 75-year-old man was admitted for cosmetic concerns caused by gradual protrusion inside of the upper and lower eyelids and bilateral epiphora for 10 years. Ten years before, he underwent dacryocystorhinostomy in both eyes for bilateral nasolacrimal duct obstruction. Epiphora completely resolved at the time of surgery, but recurred over the past few years, accompanied by gradual protrusion of the lacrimal puncta. Slit-lamp examination revealed protrusion in the upper and lower lacrimal puncta measuring 2.0 and 1.5 mm, respectively, for both eyes (Fig. 1A and 1B). The tear meniscus in both eyes had significantly risen. A diagnostic probing and irrigation test demonstrated normal findings. Although mild eyelid laxity was observed on snap back test, eyelid position did not show significant abnormality. Therefore, secondary lacrimal pumping failure caused by protrusion was suspected. The patient also had cosmetic concerns. A diagnostic and therapeutic punctal fixation was performed. A circular incision was made in the base of the protrusion beneath the lacrimal punctum opening. Partial thickness surrounding tissues were excised from the conjunctival epithelial to the stromal layer in order to preserve the pumping function of the canaliculus while minimizing damage to the punctal opening (Fig. 1C). The incision site and base was sutured radially using 8-0 polyglactin 910 (Coated Vicryl; Ethicon, Somerville, NJ, USA) (Fig. 1D). After 2 weeks, the patient's epiphora was completely resolved. The tear meniscus level had decreased to near normal, and irrigation test showed normal tear drainage (Fig. 1E and 1F). Before the past 2 years, the patient showed no signs of stenosis or eyelid entropion caused by fibrosis, and the tear meniscus level had been normal.
Abnormalities in the position of the lacrimal punctum lead to punctal ectropion in the lower eyelid resulting from decreased tension in the medial canthal tendon. This is accompanied by punctal ectropion or decreased tear drainage [3]. This condition is frequently observed in seniors and is a common cause of chronic epiphora and conjunctival hyperemia [4]. However, positional abnormalities due to lacrimal punctum protrusion have not been previously reported, and only a significant negative correlation between the severity of punctal protrusion and tear clearance has been reported in the literature [5]. The patient showed a lower eyelid laxity of grade 1 during the initial examination and it was unclear whether the inability to discharge tears was caused by protrusion. Early surgical treatment was attempted as the patient also raised cosmetic concerns. Epiphora improved considerably, and it was confirmed that the case was caused by decreased tear flow due to punctum protrusion.
In conclusion, we report a case of epiphora caused by an abnormal lacrimal punctum position due to severe protrusion. The patient was successfully treated with a novel punctal fixation technique.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






